Screening and Genetic Diagnosis of Hemoglobinopathies in Southern and Northern Europe: Two Examples
^Antonio Amato and *Piero C. Giordano
^Associazione Nazionale Microcitemie Italia (ANMI ONLUS), Centro Studi Microcitemie di Roma, Roma, Italia.
*Hemoglobinopathies Laboratory, Human and Clinical Genetics Department, Leiden University Medical Center, The Netherlands
Correspondence to: Piero C. Giordano, Hemoglobinopathies Laboratory, Human and Clinical Genetics Department, Leiden University Medical Center, The Netherlands E-mail: P.C.Giordano@lumc.nl
Published: August 08, 2009
Received: June 30, 2009
Accepted: August 06, 2009
Medit J Hemat Infect Dis 2009, 1(1): e2009007 DOI 10.4084/MJHID.2009.007
This article is available from: http://www.mjhid.org/article/view/4658
This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited
Abstract
Prevention
of Hemoglobinopathies has developed around the world based upon the
experience done in pioneering endemic countries and is now facing a new
phase in non-endemic areas with a recent immigration history. We
describe two situations, taking Latium (central Italy) and The
Netherlands as two models for endemic and non-endemic countries both
confronted with a large multi-ethnic immigrant society. We present
prevention results and discuss aspects such as local knowledge and
organization. We illustrate the importance of issues like information,
carrier diagnostics, screening, counseling and prenatal diagnosis in
particular situation of contrasting interest an different ethical
opinions. We conclude by underlining the importance of implementing
primary prevention at the European level, based upon better
information, diagnostics and counseling.
Introduction:
Hemoglobinopathies (HbP’s) are the most common recessive autosomal disorders in man because carriers are protected against child mortality due to malaria. This advantage has strongly selected the traits in all tropic and sub-tropic areas of the old world were most carriers live today. However, due to ancient and recent migrations HbP’s are now present virtually everywhere including those non-endemic industrialized areas where people from endemic countries migrate in search of work.
Severe Hemoglobinopathies (Thalassemia and Sickle Cell Disease) are conditions affecting our oxygen transport protein hemoglobin A (HbA). This tetramer consists of 4 globin chains (α2/β2) coded by genes located on chromosome 16 (the alpha genes) and 11 (the beta genes). While β-Thalassemia is caused by defects impairing the expression of the β globin genes, Sickle Cell Disease (SCD) is induced by a single β-gene mutation (HbS), either in homozygous form (HbS/S) or in a number of common compound heterozygous conditions such as HbS/β-thal, HbS/C, HbS/D, HbS/E and others.
The WHO has been recommending primary prevention for many years because these severe diseases, although treatable, cannot be “cured” unless a bone marrow transplant is successfully performed. Therefore primary prevention has been offered for the last 30 years to couples at risk in the Mediterranean area where the incidence of β-Thalassemia major in pioneering countries like Cyprus, Italy and Greece has been reduced to almost zero [1-3].
Preface. To day also non-endemic countries are in urgent need of prevention because immigrant couples from endemic countries usually do not mix with Northern European, make more children than average and often with a consanguineous partner. All this keeps the chance of getting a child affected by SCD or Thalassemia major as high as in the country of origin [4].
In the UK, dedicated colleagues were the first who succeeded building up prevention campaigns and to date neonatal screening and early pregnancy diagnostic is available in this country where the expected incidence of the severe conditions is significantly reduced [5].
In other developed Western European countries with large immigrant populations this problem has been neglected for a long time. Only by the turn of the century public health authorities started to realize that prevention had to be offered to these growing communities but with the exception of Belgium, Northern France and The Netherland, no other continental regions of North European have started offering organized prevention options as yet [6].
In The Netherlands in particular only a modest incidence reduction has been achieved thus far in spite of substantial efforts in different directions and the implementation of newborn screening (NBS) in 2007 [7]. In this country only few couples at risk reach prospective prevention after they have been properly informed and virtually none of those couples identified during NBS because they had an affected child has reached a genetic center thus far [8].
In contrast, the Thalassemia prevention program applied in the Latium region, the earliest ever planned and introduced in Italy by Silvestroni and Bianco in the early 602, can be considered as the most successful. Since 1993, prospective primary prevention (offered to couples at risk diagnosed and informed before their first pregnancy) was virtually total, reducing the expected incidence of Thalassemia major to virtually zero in the native population. However, due to the many immigrants from endemic countries that are not reached by information and carrier diagnostics, new problems are arising in Latium as well. The situations both in Latium and in The Netherlands were described as two models for endemic and non-endemic countries.
Methods:
Information and carrier diagnostics are the key elements of prevention. The moment of intervention is crucial and the sooner carriers are detected the better it is for their prevention choices. However, while early, premarital or preconception diagnostics is offered in endemic countries, non-endemic immigration countries have implemented NBS and retrospective prevention for parents of affected children is depending from the advice of pediatricians who may or may not decide to inform the parents about prevention or may or may not refer them to genetic centers.
The Latium prevention program. The long established prevention campaign consists of a focused biology lesson and universal screening for all pupils attending secondary school. The spin off of this screening consists of information of the parents, carrier diagnostics of parents and family and registration on a data base. Carrier’s follow up concern pre-matrimonial or pre-conception diagnostics, identification of couples at risk and genetic counseling, carrier diagnostics in early pregnancy and prenatal diagnosis after informed decision. Due to the rise of incidence among immigrants the information campaigns has been intensified in order to reach the immigrant population.
The Dutch prevention attempts. Prenatal diagnosis has been available in the countries from the late 80 thies at Leiden reference centre but no prevention campaigns are available. Therefore, all laboratories in the countries have been enquired and instructed how to perform basic carrier diagnostics and how to advice control of parents, partner and sibs, or the younger generation when a infant, a young or an elderly carrier have been diagnosed, respectively. However, to perform carrier diagnostics one needs a doctor prescription, Therefore, many post academic teaching courses and at least one publication a year has been dedicated to enduring education of general practitioners and midwifes over the last 10 years. Explanatory and reassuring letters, addressed to the healthy carriers, explaining the importance of prevention, have been used for all patients diagnosed at the reference centre. First pregnancy control has been offered in a pilot setting and is now implemented in the city of Gouda and is on his way to implementation in the city of The Hague. Neonatal screening has started in 2007. Affected children are referred to dedicated pediatricians in academic centers but referral of the parents to genetic centers remains sporadic. Carrier diagnostics in the preconception phase is slowly growing, mainly based upon medical indication (anemia). Carrier diagnostics based upon ethnic origin is depending from the initiative of informed GP’s eventually responding (or not) to the request of informed patients.
Technical methods:
Carrier diagnostic methods are state of the art protocols in both centers. The simple visual single tube osmotic fragility test [9] and the erythromorphology evaluation are applied systematically during school screening for Thalassemia in Latium and are part of the carrier diagnostic protocol at Leiden Reference Center, together with the measurement of standard hematological parameters on automatic counters. Both in Latium and The Netherlands separation and estimation of the hemoglobin fractions, either on alkaline electrophoresis or on capillary electro-phoresis (Capillarys, Sebia France) and on High Performance Liquid Chromatography (HPLC), is done using different dedicated devices among which the HPLC VARIANT II™ (Bio-Rad Laboratories, Hercules, CA, USA), the HA 8160 (Menarini, Florence, Italy) or the Capillay Electrophoresis device (Sebia, Paris France) as described elsewhere[10]. Ferritin or zink proto-porphirine are measured when needed to evaluate iron deficiency.
Molecular analysis is performed in both labs, either routinely or when needed. Genomic DNA is isolated by salt-extraction and point mutation analysis of the globin gene is done by direct sequencing using commercial devices (ABI Prism, USA). Complex cases are studied by globin chain synthesis [11] and eventually in collaboration [12].
Results:
Latium: In the period 2002-2007, 13.597 foreign pupils from 140 different nations, representing the 8.2% of the secondary school population (age 13) were investigated and screened regularly each year. After explaining that school screening is a way to detect healthy carriers and, in due time, couples at risk, 69.4% of the parents responded in favor of prevention sharing the information with their relatives. Screening compliance in immigrants families (64%) was higher than among Italians showing that this initiative is not felt as a stigmatizing issue.
Between 1994 and 2008 a total of 180,477 individuals were examined at the Ambulatory Care Clinic for carrier diagnostics. The share of foreign subjects visiting our structure has increased in this period from 2.7% in 1994, to 9.74% in 2008.
We have found 8,826 foreign individuals non carriers (of which 2,766 were iron deficient and 6,060 normal) and 2,917 carriers or affected. In the last cohort 22.2% were b-thalassemia carriers, 50.25% were suspected -thalassemia carriers, 13.06% were HbS, 3.7% HbE, and 1.64% HbC carriers, while 4.18% were carriers of rare Hb variants and 4.97% were affected with severe conditions deriving from associations with HbS, HbC, HbE, aį-thalassemia (HbH disease) and β-thalassemia mutations uncommon in the native Italian population.
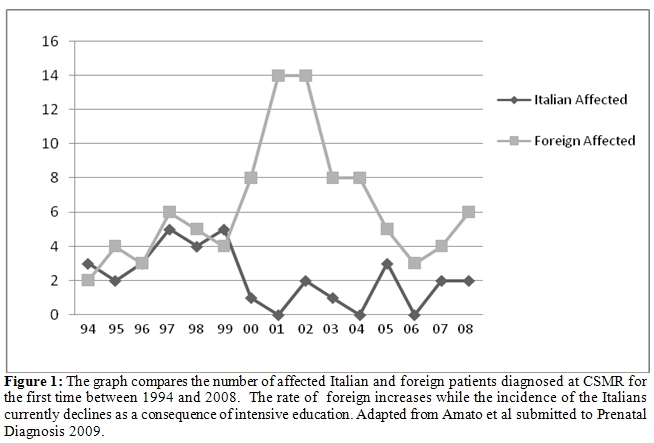
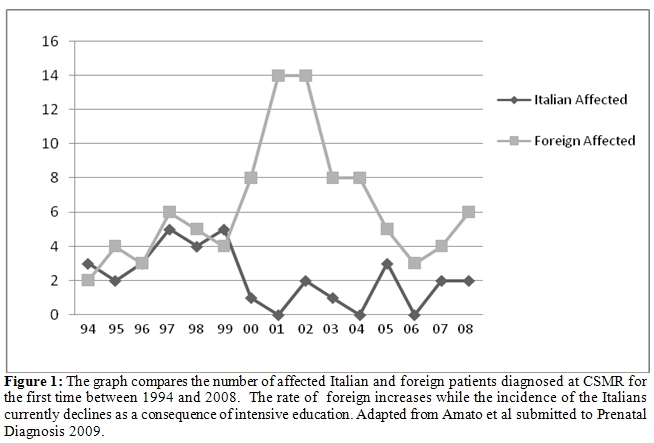
In spite of these efforts, the established prevention program does not reach all immigrants and the incidence of non indigenous affected people has increased. Since 2000 practically all affected children are from recent immigrants. The few patients of Italian origin born after 1994 are from well informed couples at risk who refused prenatal diagnosed as a consequence of a personal choice. Data are shown in Figure 1.
The Netherlands: Although compared with 10 years ago the improvement is substantial, prevention is still blocked at several bottlenecks in The Netherlands.
Most laboratories in the country are able to provide basic carrier diagnostics [13] but GP’s are still not controlling their foreign clients routinely. Referral for carrier diagnostics is eventually done based upon a diagnostic protocol published by the Dutch GP’s organization advising control when anemia persists after iron therapy [14]. Of course following this protocol most carriers of HbS, C, ad D will remain undiagnosed unless dedicated GP’s will refer upon ethnic indication. Unfortunately, control upon ethnic indication is not yet officially advised by the GP’s organization, while it is for diabetes screening in people of Hindu origin [15].
It can be estimated that all together no more than 6.000 analyses for carrier diagnostics are annually requested in this way in the country. Considering the natural incidence and the number of demands for prenatal diagnosis, less then 10% prevention has been reached in The Netherlands thus far, meaning that every year about 230 couples at risk do not reach information and miss their chance to choose for prevention.
The National Public Health Council has recently advised more research on preconception screening based on ethnic origin while recently a study at the theoretical level has proposed a strategy based on ethnic origin for combined carrier screening of Cystic Fibrosis (CF) and Hemoglobinopathy [16], this in spite of the fact that technology and financial effort are totally different.
Early pregnancy control is the most promising initiative. Dedicated midwifes who are taking good care of their clients, advise carrier diagnostics. Pilot studies have been published [17] and other pilot studies are ongoing hopefully leading soon to a new standard national protocol.
Newborn screening (NBS) has started on January 1st 2007, analyzing near 200.000 samples per year in the same 5 labs which are screening for metabolic diseases. The method of choice (HPLC) was tested at the reference lab in Leiden [18] and validated in 2006 in 2 screening laboratories [19-20]. The method detects at 100% sensitivity SCD and TM and all kind of carriers including alpha thalassemia with elevated Hb Bart’s. Nevertheless, the majority of the TM cases was missed during the first 2 years because some labs went on considering 1-2% HbA normal in non premature newborn (Normal +/- 20%) and did not feed back their results to the reference lab. Meanwhile, incidence figures have been prematurely published with a large underestimation for TM [21] while an internal discussion is ongoing whether or not to report high HbBart’s and at which level.
In spite of all that, the system is technically sound and the predicted incidence of at least 60 affected children per year was found [22]. Unfortunately, couples at risk, counseled by pediatricians have totally disregarded prevention so far8, while enquiries among local parents of affected children have long proved that prevention is welcome in more than 80% of the cases in The Netherlands [23]. Carriers of HbS, C, E, D, O, etc… should be reported for primary prevention of serious Hemoglobinopathies. Unfortunately only HbS carriers have been reported so far, also when parents have chosen to be fully informed. GP’s receive insufficient and unclear information regarding the NBS results and the actions to be taken. Therefore they confuse trait with disease and refer parents of HbS carriers to genetic centers making them unnecessarily worried before any risk is proved. Because of these starting problems, some consider carrier detection “unwanted byproducts” that should not be reported and would prefer to have a method that detects patients only. On the contrary, other think that carriers report should be considered also for other diseases. School screening is not available in the country but should be considered as soon as possible, especially in the large cities.
Discussion
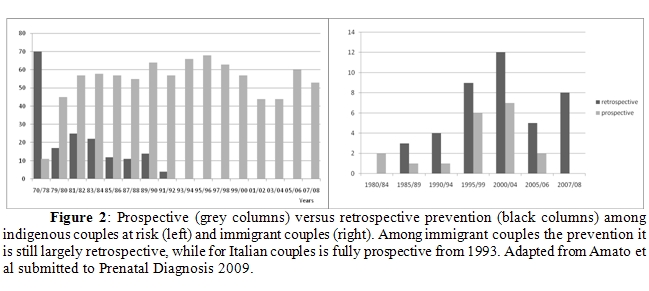
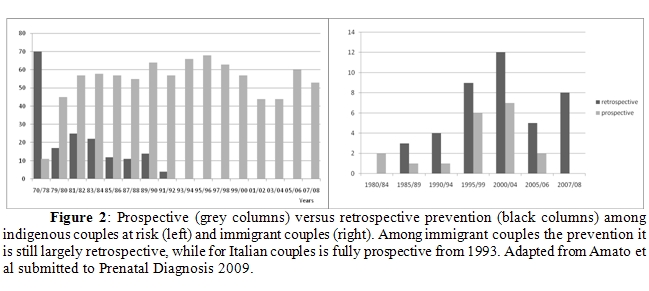
Latium: In spite of the good results in offering prospective prevention to the indigenous population (100% from 1994) the prevention for foreign couples at risk have been also in Latium mainly of the retrospective type so far (70%). Out of 60 foreign couples at risk counseled, 42 had retrospectives prevention after at least one affected child was born and only 18 couples had no affected child at the moment of identification. In spite of that our results show that by improving the information campaigns for the immigrant population prospective prevention is possible also among recent immigrants (Figure 2).
The Netherlands: The Netherlands has neglected primary prevention for the growing ethnic minorities until the turn of the century [24] and have started to give some attention to the problem only after an enduring process of persuasion [25-30].
Unfortunately, initiatives have not been primarily focused on the implementation of primary prevention strategies and in the end the only official initiative so far (NBS) was taken to provide early treatment as it is the case for Phenylketonuria (PKU). This while these patients do not need treatments shortly after birth, but from 6 months on and therefore do not need to be universally screened at birth but could be better selectively diagnosed during the first semester of life based on the ethnic origin if the GP’s would be available to do that (which is not the case at the moment).
Moreover, the NBS advisory commission is composed mainly by pediatricians, mainly interested in early treatment and much less in carrier analysis and prevention. Contrasting interests are often discussed using ethical concepts, heritage of the conservative politic of the 80 thies, based on confusions between recessive traits and late onset dominant genetic diseases. Reasonable in the last case, the right to refuse (genetic) information is improperly applied to the carriers of recessive traits, claiming that healthy carriers could possibly get worried by genetic information and that minors should not be informed until the age of 18, overlooking that in NBS is not the newborn that gets the information but the responsible parents. Under these circumstances primary prevention as a spin off of from NBS has become a tormented history in The Netherlands.
An official implementation of carrier diagnostics in preconception of early pregnancy phase, could also run the risk to become a matter of a long discussion if considered as a national screening. Therefore, carrier analysis should not be considered as a screening to be approved by politics but as a regular diagnostic procedure for which the only approval needed is the one of the informed patient and for which the indication could be a medical one or just the ethnic origin from a high prevalence area. Therefore it is essential to have informed patients requiring carrier diagnostics to informed GP’s and informed labs able to provide the analysis and an explanatory letter.
Information: It seems evident from our paper that, beside politics, information remains the main problem when implementing prevention strategies. When properly provided, information is providing knowledge and is not producing anxiety or stigmatization to ethnic minorities. Therefore information needs to be offered in a better way and to be adapted to the different cultural situations.
Information in endemic countries is directed to the whole of the population, is better understood, is provided by doctors aware of the situation and nobody is stigmatized. Information in non-endemic countries provided by public campaigns may stigmatize immigrants and should therefore be delivered privately by an educated general practitioner who does not confuses trait with disease and by pediatrician that, beside treating affected children in the best possible way, should refer couples at risk to genetic centers.
A comprehensive and reassuring letter to the diagnosed carrier, to be discussed with the family doctor, is in our experience a way to prevent anxiety and provide correct information to carriers and professional knowledge to the unaware GP. Such a letter is a task for the experienced laboratory providing the diagnosis, both in endemic and non endemic countries. Counseling may need some cultural adaptation. However the fundamental elements of counseling that can be used in all cultures are that i) being carriers is not a disease, ii) that carriers will not develop the disease later on and iii) that knowing which of the recessive traits we carry is an advantage that allows partner control and the prevention of severely affected children.
Conclusions
Prevention should be encouraged and financially supported at the European level. Prevention should be introduced based on the experiences made both in the pioneering and in immigration countries, both confronted with newcomers, new mutations, new languages and new cultures. Improved information should be provided there where immigrants do not reach prevention through the local information channels. If we do not intervene properly at the European level more severely affected children will be born, having inherited a trait from two healthy parents who have not been informed and who otherwise would have probably chosen for prevention.
Hemoglobinopathies (HbP’s) are the most common recessive autosomal disorders in man because carriers are protected against child mortality due to malaria. This advantage has strongly selected the traits in all tropic and sub-tropic areas of the old world were most carriers live today. However, due to ancient and recent migrations HbP’s are now present virtually everywhere including those non-endemic industrialized areas where people from endemic countries migrate in search of work.
Severe Hemoglobinopathies (Thalassemia and Sickle Cell Disease) are conditions affecting our oxygen transport protein hemoglobin A (HbA). This tetramer consists of 4 globin chains (α2/β2) coded by genes located on chromosome 16 (the alpha genes) and 11 (the beta genes). While β-Thalassemia is caused by defects impairing the expression of the β globin genes, Sickle Cell Disease (SCD) is induced by a single β-gene mutation (HbS), either in homozygous form (HbS/S) or in a number of common compound heterozygous conditions such as HbS/β-thal, HbS/C, HbS/D, HbS/E and others.
The WHO has been recommending primary prevention for many years because these severe diseases, although treatable, cannot be “cured” unless a bone marrow transplant is successfully performed. Therefore primary prevention has been offered for the last 30 years to couples at risk in the Mediterranean area where the incidence of β-Thalassemia major in pioneering countries like Cyprus, Italy and Greece has been reduced to almost zero [1-3].
Preface. To day also non-endemic countries are in urgent need of prevention because immigrant couples from endemic countries usually do not mix with Northern European, make more children than average and often with a consanguineous partner. All this keeps the chance of getting a child affected by SCD or Thalassemia major as high as in the country of origin [4].
In the UK, dedicated colleagues were the first who succeeded building up prevention campaigns and to date neonatal screening and early pregnancy diagnostic is available in this country where the expected incidence of the severe conditions is significantly reduced [5].
In other developed Western European countries with large immigrant populations this problem has been neglected for a long time. Only by the turn of the century public health authorities started to realize that prevention had to be offered to these growing communities but with the exception of Belgium, Northern France and The Netherland, no other continental regions of North European have started offering organized prevention options as yet [6].
In The Netherlands in particular only a modest incidence reduction has been achieved thus far in spite of substantial efforts in different directions and the implementation of newborn screening (NBS) in 2007 [7]. In this country only few couples at risk reach prospective prevention after they have been properly informed and virtually none of those couples identified during NBS because they had an affected child has reached a genetic center thus far [8].
In contrast, the Thalassemia prevention program applied in the Latium region, the earliest ever planned and introduced in Italy by Silvestroni and Bianco in the early 602, can be considered as the most successful. Since 1993, prospective primary prevention (offered to couples at risk diagnosed and informed before their first pregnancy) was virtually total, reducing the expected incidence of Thalassemia major to virtually zero in the native population. However, due to the many immigrants from endemic countries that are not reached by information and carrier diagnostics, new problems are arising in Latium as well. The situations both in Latium and in The Netherlands were described as two models for endemic and non-endemic countries.
Methods:
Information and carrier diagnostics are the key elements of prevention. The moment of intervention is crucial and the sooner carriers are detected the better it is for their prevention choices. However, while early, premarital or preconception diagnostics is offered in endemic countries, non-endemic immigration countries have implemented NBS and retrospective prevention for parents of affected children is depending from the advice of pediatricians who may or may not decide to inform the parents about prevention or may or may not refer them to genetic centers.
The Latium prevention program. The long established prevention campaign consists of a focused biology lesson and universal screening for all pupils attending secondary school. The spin off of this screening consists of information of the parents, carrier diagnostics of parents and family and registration on a data base. Carrier’s follow up concern pre-matrimonial or pre-conception diagnostics, identification of couples at risk and genetic counseling, carrier diagnostics in early pregnancy and prenatal diagnosis after informed decision. Due to the rise of incidence among immigrants the information campaigns has been intensified in order to reach the immigrant population.
The Dutch prevention attempts. Prenatal diagnosis has been available in the countries from the late 80 thies at Leiden reference centre but no prevention campaigns are available. Therefore, all laboratories in the countries have been enquired and instructed how to perform basic carrier diagnostics and how to advice control of parents, partner and sibs, or the younger generation when a infant, a young or an elderly carrier have been diagnosed, respectively. However, to perform carrier diagnostics one needs a doctor prescription, Therefore, many post academic teaching courses and at least one publication a year has been dedicated to enduring education of general practitioners and midwifes over the last 10 years. Explanatory and reassuring letters, addressed to the healthy carriers, explaining the importance of prevention, have been used for all patients diagnosed at the reference centre. First pregnancy control has been offered in a pilot setting and is now implemented in the city of Gouda and is on his way to implementation in the city of The Hague. Neonatal screening has started in 2007. Affected children are referred to dedicated pediatricians in academic centers but referral of the parents to genetic centers remains sporadic. Carrier diagnostics in the preconception phase is slowly growing, mainly based upon medical indication (anemia). Carrier diagnostics based upon ethnic origin is depending from the initiative of informed GP’s eventually responding (or not) to the request of informed patients.
Technical methods:
Carrier diagnostic methods are state of the art protocols in both centers. The simple visual single tube osmotic fragility test [9] and the erythromorphology evaluation are applied systematically during school screening for Thalassemia in Latium and are part of the carrier diagnostic protocol at Leiden Reference Center, together with the measurement of standard hematological parameters on automatic counters. Both in Latium and The Netherlands separation and estimation of the hemoglobin fractions, either on alkaline electrophoresis or on capillary electro-phoresis (Capillarys, Sebia France) and on High Performance Liquid Chromatography (HPLC), is done using different dedicated devices among which the HPLC VARIANT II™ (Bio-Rad Laboratories, Hercules, CA, USA), the HA 8160 (Menarini, Florence, Italy) or the Capillay Electrophoresis device (Sebia, Paris France) as described elsewhere[10]. Ferritin or zink proto-porphirine are measured when needed to evaluate iron deficiency.
Molecular analysis is performed in both labs, either routinely or when needed. Genomic DNA is isolated by salt-extraction and point mutation analysis of the globin gene is done by direct sequencing using commercial devices (ABI Prism, USA). Complex cases are studied by globin chain synthesis [11] and eventually in collaboration [12].
Results:
Latium: In the period 2002-2007, 13.597 foreign pupils from 140 different nations, representing the 8.2% of the secondary school population (age 13) were investigated and screened regularly each year. After explaining that school screening is a way to detect healthy carriers and, in due time, couples at risk, 69.4% of the parents responded in favor of prevention sharing the information with their relatives. Screening compliance in immigrants families (64%) was higher than among Italians showing that this initiative is not felt as a stigmatizing issue.
Between 1994 and 2008 a total of 180,477 individuals were examined at the Ambulatory Care Clinic for carrier diagnostics. The share of foreign subjects visiting our structure has increased in this period from 2.7% in 1994, to 9.74% in 2008.
We have found 8,826 foreign individuals non carriers (of which 2,766 were iron deficient and 6,060 normal) and 2,917 carriers or affected. In the last cohort 22.2% were b-thalassemia carriers, 50.25% were suspected -thalassemia carriers, 13.06% were HbS, 3.7% HbE, and 1.64% HbC carriers, while 4.18% were carriers of rare Hb variants and 4.97% were affected with severe conditions deriving from associations with HbS, HbC, HbE, aį-thalassemia (HbH disease) and β-thalassemia mutations uncommon in the native Italian population.
In spite of these efforts, the established prevention program does not reach all immigrants and the incidence of non indigenous affected people has increased. Since 2000 practically all affected children are from recent immigrants. The few patients of Italian origin born after 1994 are from well informed couples at risk who refused prenatal diagnosed as a consequence of a personal choice. Data are shown in Figure 1.
The Netherlands: Although compared with 10 years ago the improvement is substantial, prevention is still blocked at several bottlenecks in The Netherlands.
Most laboratories in the country are able to provide basic carrier diagnostics [13] but GP’s are still not controlling their foreign clients routinely. Referral for carrier diagnostics is eventually done based upon a diagnostic protocol published by the Dutch GP’s organization advising control when anemia persists after iron therapy [14]. Of course following this protocol most carriers of HbS, C, ad D will remain undiagnosed unless dedicated GP’s will refer upon ethnic indication. Unfortunately, control upon ethnic indication is not yet officially advised by the GP’s organization, while it is for diabetes screening in people of Hindu origin [15].
It can be estimated that all together no more than 6.000 analyses for carrier diagnostics are annually requested in this way in the country. Considering the natural incidence and the number of demands for prenatal diagnosis, less then 10% prevention has been reached in The Netherlands thus far, meaning that every year about 230 couples at risk do not reach information and miss their chance to choose for prevention.
The National Public Health Council has recently advised more research on preconception screening based on ethnic origin while recently a study at the theoretical level has proposed a strategy based on ethnic origin for combined carrier screening of Cystic Fibrosis (CF) and Hemoglobinopathy [16], this in spite of the fact that technology and financial effort are totally different.
Early pregnancy control is the most promising initiative. Dedicated midwifes who are taking good care of their clients, advise carrier diagnostics. Pilot studies have been published [17] and other pilot studies are ongoing hopefully leading soon to a new standard national protocol.
Newborn screening (NBS) has started on January 1st 2007, analyzing near 200.000 samples per year in the same 5 labs which are screening for metabolic diseases. The method of choice (HPLC) was tested at the reference lab in Leiden [18] and validated in 2006 in 2 screening laboratories [19-20]. The method detects at 100% sensitivity SCD and TM and all kind of carriers including alpha thalassemia with elevated Hb Bart’s. Nevertheless, the majority of the TM cases was missed during the first 2 years because some labs went on considering 1-2% HbA normal in non premature newborn (Normal +/- 20%) and did not feed back their results to the reference lab. Meanwhile, incidence figures have been prematurely published with a large underestimation for TM [21] while an internal discussion is ongoing whether or not to report high HbBart’s and at which level.
In spite of all that, the system is technically sound and the predicted incidence of at least 60 affected children per year was found [22]. Unfortunately, couples at risk, counseled by pediatricians have totally disregarded prevention so far8, while enquiries among local parents of affected children have long proved that prevention is welcome in more than 80% of the cases in The Netherlands [23]. Carriers of HbS, C, E, D, O, etc… should be reported for primary prevention of serious Hemoglobinopathies. Unfortunately only HbS carriers have been reported so far, also when parents have chosen to be fully informed. GP’s receive insufficient and unclear information regarding the NBS results and the actions to be taken. Therefore they confuse trait with disease and refer parents of HbS carriers to genetic centers making them unnecessarily worried before any risk is proved. Because of these starting problems, some consider carrier detection “unwanted byproducts” that should not be reported and would prefer to have a method that detects patients only. On the contrary, other think that carriers report should be considered also for other diseases. School screening is not available in the country but should be considered as soon as possible, especially in the large cities.
Discussion
Latium: In spite of the good results in offering prospective prevention to the indigenous population (100% from 1994) the prevention for foreign couples at risk have been also in Latium mainly of the retrospective type so far (70%). Out of 60 foreign couples at risk counseled, 42 had retrospectives prevention after at least one affected child was born and only 18 couples had no affected child at the moment of identification. In spite of that our results show that by improving the information campaigns for the immigrant population prospective prevention is possible also among recent immigrants (Figure 2).
The Netherlands: The Netherlands has neglected primary prevention for the growing ethnic minorities until the turn of the century [24] and have started to give some attention to the problem only after an enduring process of persuasion [25-30].
Unfortunately, initiatives have not been primarily focused on the implementation of primary prevention strategies and in the end the only official initiative so far (NBS) was taken to provide early treatment as it is the case for Phenylketonuria (PKU). This while these patients do not need treatments shortly after birth, but from 6 months on and therefore do not need to be universally screened at birth but could be better selectively diagnosed during the first semester of life based on the ethnic origin if the GP’s would be available to do that (which is not the case at the moment).
Moreover, the NBS advisory commission is composed mainly by pediatricians, mainly interested in early treatment and much less in carrier analysis and prevention. Contrasting interests are often discussed using ethical concepts, heritage of the conservative politic of the 80 thies, based on confusions between recessive traits and late onset dominant genetic diseases. Reasonable in the last case, the right to refuse (genetic) information is improperly applied to the carriers of recessive traits, claiming that healthy carriers could possibly get worried by genetic information and that minors should not be informed until the age of 18, overlooking that in NBS is not the newborn that gets the information but the responsible parents. Under these circumstances primary prevention as a spin off of from NBS has become a tormented history in The Netherlands.
An official implementation of carrier diagnostics in preconception of early pregnancy phase, could also run the risk to become a matter of a long discussion if considered as a national screening. Therefore, carrier analysis should not be considered as a screening to be approved by politics but as a regular diagnostic procedure for which the only approval needed is the one of the informed patient and for which the indication could be a medical one or just the ethnic origin from a high prevalence area. Therefore it is essential to have informed patients requiring carrier diagnostics to informed GP’s and informed labs able to provide the analysis and an explanatory letter.
Information: It seems evident from our paper that, beside politics, information remains the main problem when implementing prevention strategies. When properly provided, information is providing knowledge and is not producing anxiety or stigmatization to ethnic minorities. Therefore information needs to be offered in a better way and to be adapted to the different cultural situations.
Information in endemic countries is directed to the whole of the population, is better understood, is provided by doctors aware of the situation and nobody is stigmatized. Information in non-endemic countries provided by public campaigns may stigmatize immigrants and should therefore be delivered privately by an educated general practitioner who does not confuses trait with disease and by pediatrician that, beside treating affected children in the best possible way, should refer couples at risk to genetic centers.
A comprehensive and reassuring letter to the diagnosed carrier, to be discussed with the family doctor, is in our experience a way to prevent anxiety and provide correct information to carriers and professional knowledge to the unaware GP. Such a letter is a task for the experienced laboratory providing the diagnosis, both in endemic and non endemic countries. Counseling may need some cultural adaptation. However the fundamental elements of counseling that can be used in all cultures are that i) being carriers is not a disease, ii) that carriers will not develop the disease later on and iii) that knowing which of the recessive traits we carry is an advantage that allows partner control and the prevention of severely affected children.
Conclusions
Prevention should be encouraged and financially supported at the European level. Prevention should be introduced based on the experiences made both in the pioneering and in immigration countries, both confronted with newcomers, new mutations, new languages and new cultures. Improved information should be provided there where immigrants do not reach prevention through the local information channels. If we do not intervene properly at the European level more severely affected children will be born, having inherited a trait from two healthy parents who have not been informed and who otherwise would have probably chosen for prevention.
References
- Angastiniotis M, Kyriakidou S, Hadjiminas
M. The Cyprus Thalassemia Control Program. Birth Defects Orig Artic
Ser. 1988;23(5B):417-32.

- Silvestroni E, Bianco I, Graziani B,
Carboni C, Valente M, Lerone M and D’Arca SU. Screening of thalasseamia
carriers in intermediate school in Latium: results of four years’work.
J Medical Genetics 1980; 17,161-164.

- Fessas P. Prevention of thalassaemia and
haemoglobin S syndromes in Greece. Acta Haematol. 1987;78(2-3):168-72.

- Modell B, Darlison M, Birgens H, Cario H,
Faustino P, Giordano PC, Gulbis B, Hopmeier P, Lena-Russo D, Romao L,
Theodorsson E. Epidemiology of haemoglobin disorders in Europe: an
overview. Scand J Clin Lab Invest. 2007;67(1):39-69. Review.

- Modell B, Petrou M, Layton M, Varnavides L,
Slater C, Ward RH, Rodeck C, Nicolaides K, Gibbons S, Fitches A, Old J.
Audit of prenatal diagnosis for haemoglobin disorders in the United
Kingdom: the first 20 years. BMJ. 1997 Sep 27;315(7111):779-84.

- Giordano PC. Prospective and retrospective
primary prevention of Hemoglobinopathies in multiethnic societies. J
Clin Bioch 2009 (in press).

- Giordano PC. Starting neonatal screening
for haemoglobinopathies in The Netherlands. J Clin Pathol 2009; 62:
18-21.

- Vansenne F, de Borgie C.A.J.M, Bouva MJ, Legdeur MA, van Zwieten R, Petrij F en Peters M. Sikkelcelziekte in de hielprikscreening II. Gerapporteerd dragerschap. Ned Tijdschr Geneeskd. 2009;153:B366.
- Silvestroni E, Bianco I. Il metodo di Simmel per lo studio delle resistenze globulari. Policlinico [Prat] 51:153-155, 1945.
- Van Delft P, Lenters E, Bakker-Verweij M,
de KorteM, Baylan U, Harteveld C.L. and Giordano PC. Evaluating
five dedicated automatic devices for hemoglobinopathy diagnostics in
multi ethnic populations. Int J Lab Hematol. 2009 Apr 17. (Epub ahead
of print).

- Amato A, Cappabianca MP, Ponzini D, Rinaldi S, Di Biagio P, Foglietta E, Grisanti P, Mastropietro F. Hb L'Aquila [beta106(G8)Leu-->Val, CTG-->GTG]: a novel thalassemic hemoglobin variant. Hemoglobin. 2007;31(3):1-4.
- Phylipsen M1, Amato A2 , Cappabianca MP2, Traeger Synodinos J3, Kanavakis E3, Basak AN, Galanello R4, Rosaltelli MC4, Harteveld CL1 and Giordano PC1. Two new β-Thalassemia deletions compromising prenatal diagnosis in an Italian and in a Turkish couple at risk. Cases Presented at the 11th International Thalassaemia Conference, Singapore October 2008 and presently submitted for publication.
- Giordano PC, Smit JW. Herruer M, Huisman W, Pouwels JGJ, Verhoef N, Idema RN en Wijermans P. Dragerschapdiagnostiek en preventie van sikkelcelziekte en thalassemia major; aanbevelingen van de werkgroep HemoglobinopathieŽn. Ned Tijdschr Klin Chem Labgeneesk 2006; 31: 301-305.
- Wijk van MAM, Mel M, Muller PA, Silverentand WGJ, Pijnenborg, L, Kolnaar BGM, NHG Standaard Anemie. Huisarts & Wetenschap 2003; 46:3-11.
- Rutten GEHM, De Grauw WJC, Nijpels G, Gouds¨waard AN, Uitewaal PJM, Van der Does FEE, Heine RJ, Van Ballegooie E, Verduijn MM, Bouma M. NHG-Standaard Diabetes mellitus type 2. Huisarts Wet 2006;49:137-52.
- Lakeman P, Plass AM, Henneman L, Bezemer
PD, Cornel MC, ten Kate LP.Three-month follow-up of Western and
non-Western participants in a study on preconceptional ancestry-based
carrier couple screening for cystic fibrosis and hemoglobinopathies in
the Netherlands. Genet Med. 2008 Nov;10:820-30.

- Giordano PC, Plancke A, Van Meir CA,
Janssen CA, Kok PJ, Van Rooijen-Nijdam IH, Tanis BC, van Huisseling JC,
Versteegh FG. Carrier diagnostics and prevention of hemoglobinopathies
in early pregnancy in The Netherlands: a pilot study. Prenat Diagn.
2006 Aug;26(8):719-24.

- P.C. Giordano. Toward state of the art neonatal screening for secondary and primary prevention of the Hemoglobinopathies in The Netherlands. Report Zon-MW isbn 90-807039-2-3.
- Bouva M, Elvers B, Giordano PC & Loeber G. Pilot newborn screening for hemoglobinopathies in the Netherlands using the Variant NBS. The 6th meeting of the International Society for Neonatal Screening. ISNS 2006 Awaji, Japan.
- Verheul FEAM, Brinkman HBJM, Mohrmann K. Pilot project neonatal screening for hemoglobinopathies using 3 different HPLC systems. The 6th meeting of the International Society for Neonatal Screening. ISNS 2006 Awaji, Japan.
- Peters M, Appel IM, Cnossen MH, Breuning-Boers JM en Heijboer H. Opgespoorde Kinderen in het eerste jaar. Ned Tijdschr Geneeskd. 2009;153:B359.
- Giordano PC, Harteveld CL. Prevention of hereditary haemoglobinopathies in The Netherlands. Ned Tijdschr Geneeskd. 2006 Sep 30;150(39):2137-41.
- Giordano PC, Dihal AA and Harteveld CL.
Estimating the attitude of immigrants toward primary prevention of the
hemoglobinopathies Prenat Diagn 2005; 25: 885–893.

- Schulpen TW, van der Lee JH, van der Most van Spijk MW, Beemer FA.Genetic carrier screening for hemoglobinopathies in the Netherlands is not opportune. Ned Tijdschr Geneeskd. 1998; 142(18):1019-1022.
- Giordano PC, Harteveld CL, Bernini LF. The need for diagnosis and prevention of hemoglobinopathies in Northern Europe: The Dutch situation. Haematologica 1999; 84:103-104.
- Giordano PC & Harteveld CL. Hemoglobinopathies in The Netherlands: The role of the GP in carrier diagnostics and prevention (in Dutch). Huisarts & Wetenschap. 1998; 6:290-295.
- Elion-Gerritzen WE, Giordano PC, Haak HL. Anemia in the midwife practice. Standard issued by the Royal Dutch Organisation of Midwives: a risk of not recognizing iron deficiency and hemoglobinopathy. Ned Tijdschr Geneeskd. (2002) 146(10):457-459.
- Giordano PC, Harteveld CL, Dihal A, Bernini LF. Prevention of hemoglobino-pathies in the Netherlands: An individual approach based on information and prospective diagnostiscs. The Hematology Journal. 2000; 1:31.P120.
- Giordano PC, Harteveld CL. Information and carrier diagnostiscs as a basis for hemoglobinopathies prevention in The Netherlands: A task for the first line healthcare. Eur Jour Hum Genet. 2000; 8(1);54 P128.
- Giordano PC, Harteveld CL and Bernini LF. Prevention of hemoglobinopathies in the immigrant populations of northern Europe: The Netherlands. The 8th International Conference on Thalassemia and the Hemoglobinopathies 2001; abstract nr P09.