Demographical, Viro-Immunological, Clinical and Therapeutical
Characteristics of HIV-Infected Patients in an “Epidemiologically
Unexplored” Region of Italy (Calabria Region): the CalabrHIV Cohort
Maria Concetta Postorino1,
Filippo Luciani2, Carmelo Mangano3,
Maria Stella Carpentieri3, Paolo Scerbo4,
Armando Priamo4, Giuseppina Berardelli5,
Roberto Marino6, Alfredo Vallone6,
Nicola Serrao7, Vincenzo Pisani1,
Chiara Costa1, Albano Terremoto2,
Giuseppe Foti3, Lucio Cosco4,
Massimo Calderazzo5, Domenico Corigliano5,
Preziosa Scordo1, Alessio Strazzulla1,
Carlo Torti1 and the CalabrHIV Study Group
1Infectious
Diseases Unit, “Magna Graecia” University, Catanzaro
2Infectious Diseases Unit, “Annunziata”
Hospital, Cosenza
3Infectious Diseases Unit,
“Bianchi-Melacrino-Morelli” Hospital, Reggio Calabria
4Infectious Diseases Unit, “Pugliese-Ciaccio”
Hospital, Catanzaro
5Infectious Diseases Unit, “Giovanni Paolo II”
Hospital, LameziaTerme, Catanzaro
6Infectious Diseases Unit, “Jazzolino” Hospital,
Vibo Valentia
7Infectious Diseases Unit, “San Giovanni di Dio”
Hospital, Crotone
Corresponding author: Maria Concetta Postorino,
Infectious Diseases Unit, “Magna Graecia” University, Catanzaro. Tel:
+39 0961 3647203; Fax: +39 0961 3647544; viale Europa, loc. Germaneto
88100 Catanzaro, Italy. E-mail:
cettypostorino@gmail.com
Published: October 8, 2015
Received: March 21, 2015
Accepted: September 13, 2015
Mediterr J Hematol Infect Dis 2015, 7(1): e2015054, DOI
10.4084/MJHID.2015.054
This article is available on PDF format at:

This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background
and Objectives: HIV
epidemics may differ among epidemiological contexts. We aimed at
constructing an HIV clinical cohort whose main epidemiological,
clinical and therapeutical characteristics are described (the CalabrHIV
cohort, Calabria Region, Southern Italy).
Methods:
The CalabrHIV Cohort includes all HIV patients on active follow-up in
all infectious disease centers in the Calabria Region as at October
2014. All information was recorded in a common electronic database.
Not-infectious co-morbidities (such as cardiovascular diseases, bone
fractures, diabetes, renal failure and hypertension) were also studied.
Results:
548 patients (68% males; 59% aged <50 years) were included in
the
CalabrHIV cohort. Major risk factors were: sexual transmission (49%)
and intravenous drug use (34%). 39% patients had HCV and/or HBV
co-infection. Amongst 404 patients who had a complete clinical history,
34% were AIDS presenters and 49.3% had CD4 count ≤350/mm3
at HIV diagnosis. 83% patients on HAART had undetectable HIV-RNA.
Hypertension was the most frequent co-morbidity (21.5%). Multimorbidity
was more frequent in >50 years old patients than in <50
years old
ones (30% vs. 6%; p<0.0001). Co-morbidity was more frequent in
HCV
and/or HBV co-infected than in HIV mono-infected patients (46.6% vs.
31.7%: p=0.0006).
Conclusion:
This cohort presentation study sheds light, for the first time, on HIV
patients’ characteristics in the Calabria Region. We showed that
HIV-infected patients with chronic hepatitis were affected by
concomitant not-infectious co-morbidities more than the HIV
mono-infected individuals. New HCV treatments are therefore to be
implemented in the co-infected population.
|
Introduction
HIV infection may give diverse clinical manifestations, due to
virus-related factors, but also to host-related conditions and
psycho-social peculiarities. Therefore, epidemiological and clinical
features of HIV-infected patients may be different across different
countries and regions of the same country, so detailed regional
analyzes are very important to identify health priorities of HIV
patients.
Percentages of patients with HIV infection and/or with
AIDS have been underrated in the Calabria Region. Major causes may be
hypothesized: stigma and marginalization due to HIV diagnosis,[1]
the psycho-social fragility of HIV population, under-reporting of new
HIV diagnoses. Moreover, in the Calabria Region, incidence, prevalence
and characteristics of diseases (including HIV) are affected by a
massive “health migration”. Indeed, for a matter of reasons, many
patients living in the Calabria Region choose to be followed in
Hospitals located in the North and Centre of Italy.
In HIV patients also drug prescription can diverge from national
guidelines on regional clinical practice.[2]
Moreover, there are no available data regarding premature aging and
not-infective co-morbidities in HIV-infected patients from the Calabria
region.[3]
So, the aim of this study was to
describe baseline characteristics of HIV population in active follow-up
in the Calabria Region, in order to identify health priorities of
patients and create a large regional prospective cohort including all
HIV-infected patients (the CalabrHIV Cohort). Main epidemiological,
clinical and therapeutical characteristics have been assessed for the
first time in our region. Moreover, we wanted to explore in
HIV-infected patients whether or not HCV or HBV co-infection was
associated with higher percentages of not-infectious co- morbidities
than HIV mono-infection.
Both HIV and HCV are associated with a wide range of co-morbidities.[4-7]
In particular, HIV-infected patients suffer from premature aging,
putting them at risk of not-infectious co-morbidities at younger ages
than the general population.[3,4]
Indeed, high levels
of predictive biomarkers of inflammation typical of the great elderly
people were found in young people with HIV infection.[3]
Previous cohort studies showed a greater risk of diabetes mellitus,
acute myocardial infarction and cerebrovascular events in HIV-infected
patients than in HIV-negative ones.[8-12]
It is
currently not demonstrated whether HCV or HBV co-infection may
accelerate premature aging in HIV-infected patients, increasing rates
of cardiovascular, metabolic and renal diseases in these subjects. In
conclusion, the reasons leading to the study were:
1. To present a cohort profile of the
CalabrHIV study group.
2. To focus on clinical characteristics
of the enrolled patients, mainly the risk of comorbidities.
Materials and methods
All the infectious
diseases centers in the Calabria Region (Catanzaro, Vibo Valentia,
Reggio Calabria, Cosenza, and Crotone) have merged their data to create
a regional observational prospective cohort, so called CalabrHIV
Cohort. Patients’ characteristics were collected in a common electronic
database containing all epidemiological, demographic, virological,
immunological, clinical and therapeutic information. Latest follow-up
was available in October 2014.
Not-infectious comorbidities
diagnosed until October 2014 were also recorded: cardiovascular
diseases (defined as acute myocardial infarction, stroke, transient
ischemic attack, angina pectoris, coronary bypass, angioplasty, chronic
occlusive arterial disease), hypertension (defined as blood pressure
≥140/90 mmHg or antihypertensive therapy), diabetes (fasting serum
glucose ≥126 mg/dl or anti-diabetes therapy), renal failure (eGFR
≤60ml/min measured with CKD-EPI formula)[13]
and bone
fractures. Multimorbidity was defined as ≥2 not-infectious
co-morbidities occurring in the same patient. For the analysis of
not-infectious co-morbidities, patients were divided into four age
groups: aged ≤40, between 41 and 50 years, between 51 and 60 years and
>60 years.
Data were analyzed using common statistical descriptive procedures
(with statistical significance: p≤0.05).
Results
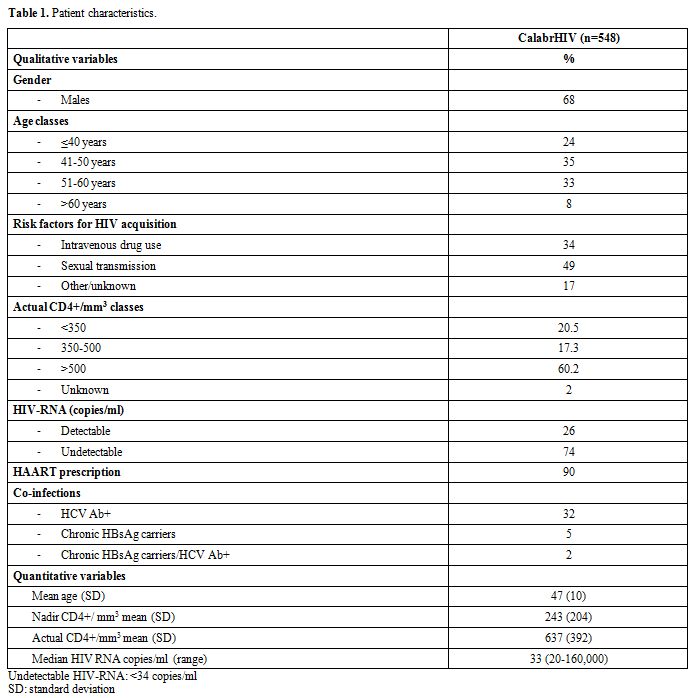
Five hundred forty-eight patients (68% males; 59% aged
<50 years)
on active follow-up as at October 2014 were included in the CalabrHIV
Cohort. Table 1
reports the
main patients’ demographic, epidemiological and clinical
characteristics. Major risk factors for HIV acquisition were sexual
transmission (49%) and intravenous drug use (34%). About 40% patients
had HCV and/or HBV co-infection.
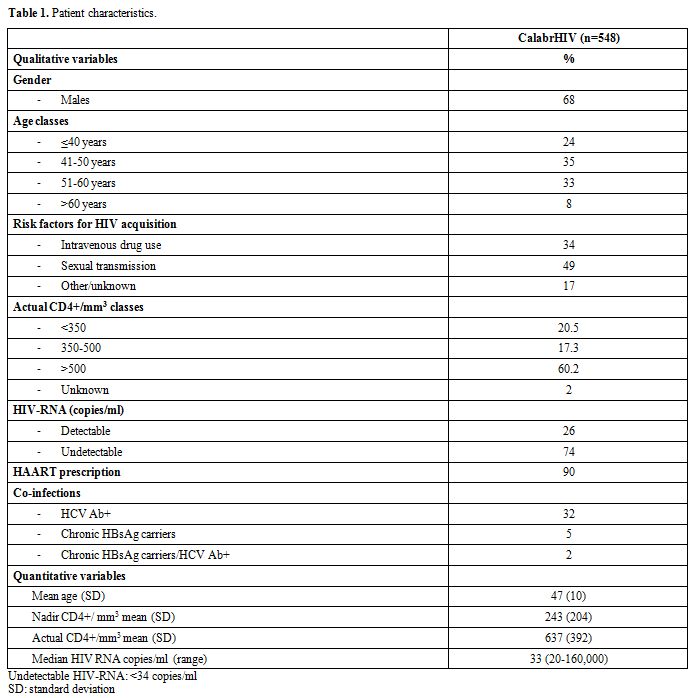 |
Table 1.
Patient’ characteristics. |
AIDS
and late presentation:
Although a good virological response was ongoing (73% had undetectable
HIV-RNA), the immunological status of patients, with a CD4 nadir
<200/mm3,
was still compromised. Only 42% of these patients had actual CD4 count
>500/mm3).
404/548 patients had available data about AIDS at HIV diagnosis, of
these 34% were AIDS presenters, and 49.3% had CD4 count ≤350/mm3.
HAART
prescription: 90% patients were on HAART and, among these, 83% had
undetectable HIV-RNA. A huge diversity in HAART prescription was
noticed: 92% first-line HAART included ≥3 different drugs. Only 5%
first line prescriptions included <3 antiretroviral drugs but,
amongst the currently ongoing regimens, 15% included <3 drugs as
simplification regimens. 49% patients actually in mono-/ dual- therapy
vs. 40% patients actually in HAART had a nadir CD4 <200/mm3.
Actual HIV RNA was <50 copies/ml in 81% patients receiving
mono-/
dual- therapy and in 83% of patients on HAART. The actual CD4 T cell
count was >500/mm3
in 60% patients receiving mono-/ dual- therapy and in 62% patients on
HAART.
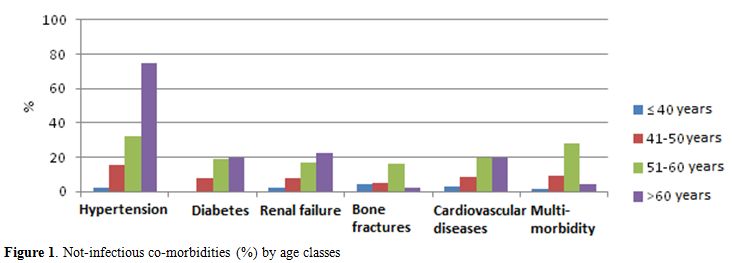
Study
of not infectious co-morbidities:
Median value of not infectious comorbidities per patient was 0.58
(range 0-4). 21.5% patients had at least one co-morbidity. None of the
patients had five, not infectious comorbidities. Hypertension was the
most frequent disease (21.5% patients) followed by cardiovascular
diseases (11.5%), renal failure (10%) and diabetes (10%) (Figure 1).
Multimorbidity was more frequently found higher in >50 years old
patients than in <50 years old (30% vs. 6%; p<0.0001) (Figure 2).
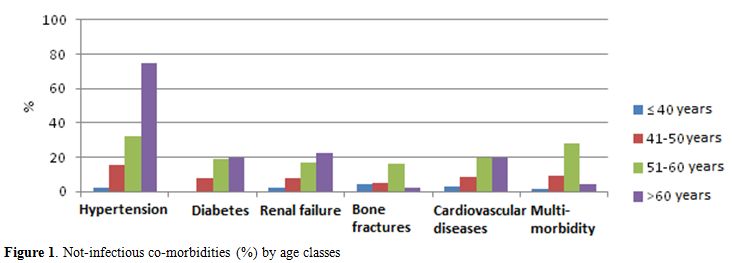 |
Figure
1. Not-infectious co-morbidities (%) by age classes |
|
|
Figure
2. Multi-morbidity (% by age classes) in CalabrHIV cohort. |
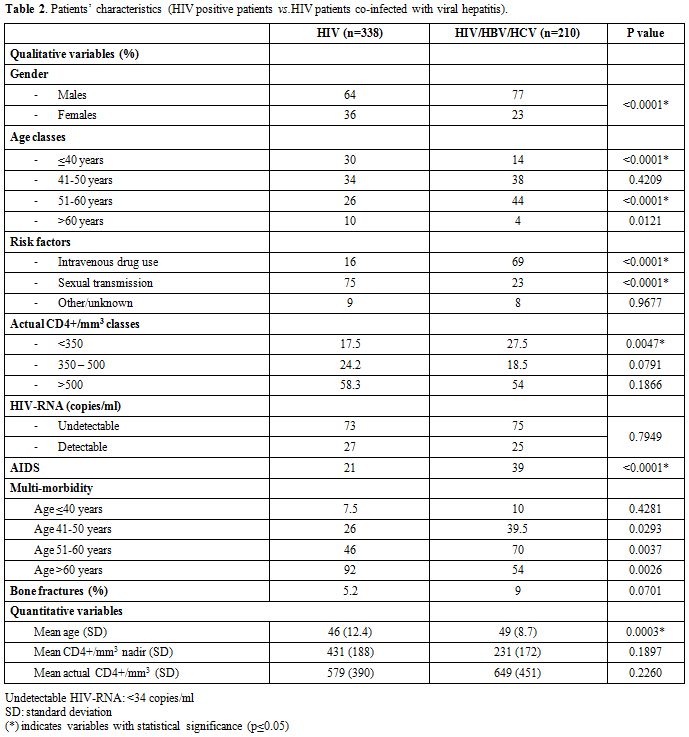
Patients
were ranked into two groups: HIV mono-infected patients
(61%) and HIV patients co-infected with HCV and/or HBV (39%).
Table 2
shows main epidemiological, clinical and demographic characteristics of
HIV mono-infected patients and HIV patients coinfected with HCV and/or
HBV. Co-infected patients were significantly older [mean age 49 years
(SD 8.7) vs. 46 years (SD 12.7); p=0.0003] and more frequently had AIDS
than mono-infected ones (39% vs. 21%; p<0.0001). Although not
statistically significant, nadir and actual CD4 T cell values were
lower in co-infected patients than in mono-infected ones.
Multimorbidity
rate was higher in patients aged ≥50 years with HCV and/or HBV
co-infection than in HIV-mono-infected (70% vs. 46%; p=0.0037). An
increased significance in the difference due to multimorbidity was
found in age groups starting from 40 years (39.5% vs. 26%; p=0.0293),
although difference was even inverse at >60 years of age (54%
vs.
92%; p=0.026) (Figure 3a-b).
There was a difference in bone fractures rates between HIV
mono-infected patients and patients with HCV and/or HBV co-infection at
a borderline significance value (5.2% vs. 9%; p=0.07).
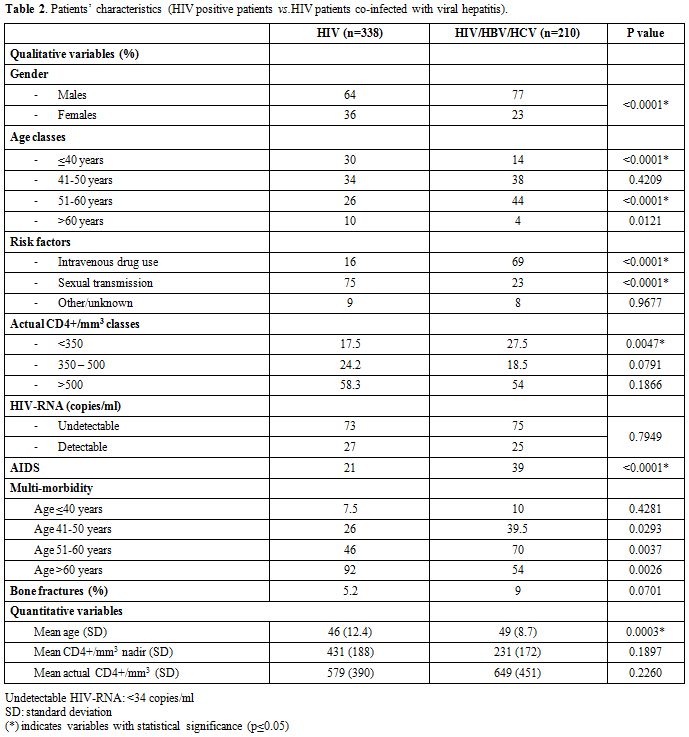 |
Table 2.
Patients’ characteristics (HIV positive patients vs.HIV patients
co-infected with viral hepatitis). |
|
|
Figure
3. a) % Multi-morbidity in HIV mono infected patients; b) %
Multi-morbidity in HIV patients co-infected with viral hepatitis |
Discussion
This
paper describes, for the first time, the main epidemiological and
clinical features of HIV patients in the Calabria Region. This large
number of patients with HIV infection, included in our study, suggests
that the HIV/AIDS epidemic in the Calabria Region is more important
than currently believed. More than 500 patients were on
active
follow-up, notwithstanding that the last estimates of National
Institute of Health reported the lowest incidence of new HIV diagnoses
among Italian regions in Calabria (0.2/100,000 inhabitants in 2012,
1.4/100,000 in 2013).[14] As
previously suggested,
underreporting, under-testing due to the fear of stigma and
marginalization, and the health migration phenomenon to areas of the
North/Centre of Italy may be some causes of this bias.[1]
Main
demographic and clinical characteristics of CalabrHIV Cohort may be
compared with other national cohorts. In particular, patients of
CalabrHIV Cohort are older (patients age was mainly up to 40 years old)
than patients belonging to the Italian MASTER Cohort (mean age 38.5
years old).[15]
This
datum may be due to selection bias since patients of older age may be
those less prone to migration. Alternatively, it may reflect a later
diagnosis (i.e., HIV infection is discovered later in life). However,
our data are consistent with national estimates; that reported a
progressive increase in mean age of patients diagnosed with HIV/AIDS in
Italy.[14]
Percentages
of late presenters in the CalabrHIV Cohort were similar to those
reported recently in Europe and Italy.[16-19]
About one third HIV patients in Europe were late presenters.[19]
Data from the Italian AIDS Registry from 1982 to 2011 showed a
progressively increased proportion of AIDS diagnoses in patients aged
>49 years in the latest years.[18]
Older patients
with AIDS were more frequently males, late testers and diagnosed with
AIDS in more recent years than younger patients.[18]
Rates of late presentation may vary by country, by nationality and by
transmission patterns. As reported in a recent international study,
rates of AIDS diagnosis within three months from HIV diagnosis in Italy
was 14.5%.[17] In Italy people,
presenting late
acquired infection more frequently by heterosexual contact, whereas, in
other countries, greater rates of late presenters were reported among
intravenous drug users.[17] Late
presentation was
associated with a higher rates of AIDS and mortality, in particular
during the first year after HIV diagnosis.[19]
Moreover, patients presented late showed a greater risk of HAART
not-adherence, drug toxicity, disease progression and death with
respect to patients who presented earlier.[20]
National
guidelines may be interpreted and applied differently in different
regional contexts. National HIV/AIDS guidelines do not recommend mono-/
dual-therapy as standard regimens.[21]
At present, a
valuable percentage of patients in the CalabrHIV cohort is treated with
<3 drugs (15%) and their viro-immunological profiles are similar
to
that of patients on HAART. Viro-immunological results in our patients
are consistent with those recently published.[22]
HIV
infection accelerates the normal process of aging.[3]
Previous studies showed a higher prevalence of not infectious
comorbidities (such as diabetes mellitus) and a greater relative risk
of acute myocardial infarction in HIV-infected patients compared with
HIV-negative ones.[8-10] Also, risk
of cerebrovascular diseases was higher in patients with HIV infection.[12]
At the same time, previous cohort studies do not explain the possible
current association between HIV infection and other risk factors of not
infectious co-morbidities (such as smoking, obesity, or family related
risk).[11,12,23]
Prevalence
of not-infectious comorbidities and multimorbidity rate in CalabrHIV
cohort were similar to those reported by Guaraldi et al.[4]
However, in that study, patients already diagnosed with lipodystrophy
and/or metabolic diseases were included, whereas, in the CalabrHIV
Cohort, HIV population may be more similar to the general.
It
is important to highlight that comorbidities rate was significantly
greater in HIV patients coinfected with HCV and/or HBV than in HIV
mono-infected patients (46.6% vs. 31.7%: p=0.0006); this datum was not
published yet. Also multimorbidity rate was higher in co-infected
patients than in HIV-mono-infected ones. This effect was not driven by
the oldest subjects since an increasing significance was found with the
increase in age starting from 40 years. Hepatitis viruses co-infection
may modify the natural history of HIV infections, further accelerating
premature aging.[24-26]
Interestingly, difference in
co-morbidity rates was even inverse (54% vs. 92%; p=0.026) at
>60
years of age in our cohort, probably because of age-related risk
diluted the impact of HCV and/or HBV co-infection in the elderly. In
conclusion, our results suggest that a greater attention should be
given to HIV co-infected patients, particularly to those of younger
age. Since eradication of HCV was associated not only with prevention
of liver-related morbidity and mortality[27]
but also with prevention of not infectious events, treatment of HCV
with the new drugs[28,29] should
be implemented.
Aims
of CalabrHIV Study Group are to continue prospective follow-up and
patients’ recruitment. Prevention and early detection of not infectious
comorbidities are important, in particular in the younger ones.
Treatment of HCV should be extended to patients infected with HIV with
the aim of improving both liver and general conditions of patients.
Acknowledgments
In addition to the authors of this paper, CalabrHIV Cohort
thanks all patients, doctors, nurses and colla+
\borators
of all participating centers: Infectious Diseases Unit, “Magna Graecia”
University, Catanzaro; Infectious Diseases Unit, “Annunziata” Hospital,
Cosenza; Infectious Diseases Unit, “Bianchi-Melacrino-Morelli”
Hospital, Reggio Calabria; Infectious Diseases Unit, “Pugliese-Ciaccio”
Hospital, Catanzaro, Infectious Diseases Unit, “Giovanni Paolo II”
Hospital, LameziaTerme, Catanzaro, Infectious Diseases Unit,
“Jazzolino” Hospital, Vibo Valentia, Infectious Diseases Unit, “San
Giovanni di Dio” Hospital, Crotone.
References
- Mahajan,
A.P., et al., Stigma in the HIV/AIDS epidemic: a review of the
literature and recommendations for the way forward. AIDS, 2008. 22
Suppl 2: p. S67-79. http://dx.doi.org/10.1097/01.aids.0000327438.13291.62
PMid:18641472 PMCid:PMC2835402

- Palella,
F.J., et al., Mortality in the highly active antiretroviral therapy
era: changing causes of death and disease in the HIV outpatient study.
J Acquir Immune DeficSyndr, 2006. 43(1): p. 27-34. http://dx.doi.org/10.1097/01.qai.0000233310.90484.16
PMid:16878047

- Deeks, S.G., HIV
infection, inflammation, immunosenescence, and aging. Annu Rev Med,
2011. 62: p. 141-55. http://dx.doi.org/10.1146/annurev-med-042909-093756
PMid:21090961 PMCid:PMC3759035

- Guaraldi,
G., et al., Premature age-related comorbidities among HIV-infected
persons compared with the general population. Clin Infect Dis, 2011.
53(11): p. 1120-6. http://dx.doi.org/10.1093/cid/cir627
PMid:21998278

- Hasse,
B., et al., Strong Impact of Smoking on Multimorbidity and
Cardiovascular Risk Among Human Immunodeficiency Virus-Infected
Individuals in Comparison With the General Population. Open Forum
Infect Dis, 2015. 2(3): p. ofv108. http://dx.doi.org/10.1093/ofid/ofv108
PMid:26284258 PMCid:PMC4536331

- Lombo,
B., et al., Prevalence of Metabolic Syndrome in Patients with HIV in
the Era of Highly Active Antiretroviral Therapy. Conn Med, 2015. 79(5):
p. 277-81. PMid:26245015

- Soriano,
V. and J. Berenguer, Extrahepatic comorbidities associated with
hepatitis C virus in HIV-infected patients. CurrOpin HIV AIDS, 2015.
10(5): p. 309-15. http://dx.doi.org/10.1097/COH.0000000000000175
PMid:26132342

- Brown,
T.T., et al., Antiretroviral therapy and the prevalence and incidence
of diabetes mellitus in the multicenter AIDS cohort study. Arch Intern
Med, 2005. 165(10): p. 1179-84. http://dx.doi.org/10.1001/archinte.165.10.1179
PMid:15911733

- Worm,
S.W., et al., Risk of myocardial infarction in patients with HIV
infection exposed to specific individual antiretroviral drugs from the
3 major drug classes: the data collection on adverse events of anti-HIV
drugs (D:A:D) study. J Infect Dis, 2010. 201(3): p. 318-30. http://dx.doi.org/10.1086/649897
PMid:20039804

- Triant,
V.A., et al., Increased acute myocardial infarction rates and
cardiovascular risk factors among patients with human immunodeficiency
virus disease. J ClinEndocrinolMetab, 2007. 92(7): p. 2506-12. http://dx.doi.org/10.1210/jc.2006-2190
PMid:17456578 PMCid:PMC2763385

- Rasmussen,
L.D., et al., Myocardial infarction among Danish HIV-infected
individuals: population-attributable fractions associated with smoking.
Clin Infect Dis, 2015. 60(9): p. 1415-23. http://dx.doi.org/10.1093/cid/civ013

- Rasmussen,
L.D., et al., Risk of cerebrovascular events in persons with and
without HIV: a Danish nationwide population-based cohort study. AIDS,
2011. 25(13): p. 1637-46. http://dx.doi.org/10.1097/QAD.0b013e3283493fb0
PMid:21646903

- Levey, A.S., et al., A
new equation to estimate glomerular filtration rate. Ann Intern Med,
2009. 150(9): p. 604-12. http://dx.doi.org/10.7326/0003-4819-150-9-200905050-00006
PMid:19414839 PMCid:PMC2763564

- Istituto Superiore di
Sanità, Dati HIV ed AIDS. Novembre 2014: Notiziario ISS. p.
3-47 .
- Torti
C.et al., L'infezione da HIV in Italia dall'origine dell'epidemia ad
oggi: lo studio di coorte MASTER, in Congresso SIMIT. Genova 26-29
ottobre 2014.
- Camoni,
L., et al., Late presenters among persons with a new HIV diagnosis in
Italy, 2010-2011. BMC Public Health, 2013. 13: p. 281. http://dx.doi.org/10.1186/1471-2458-13-281
PMid:23537210 PMCid:PMC3616982

- Hall,
H.I., et al., Late diagnosis and entry to care after diagnosis of human
immunodeficiency virus infection: a country comparison. PLoS One, 2013.
8(11): p. e77763. http://dx.doi.org/10.1371/journal.pone.0077763
PMid:24223724 PMCid:PMC3818378

- Camoni,
L., et al., The continued ageing of people with AIDS in Italy: recent
trend from the national AIDS Registry. Ann Ist Super Sanita, 2014.
50(3): p. 291-7.
PMid:25292277

- Mocroft,
A., et al., Risk factors and outcomes for late presentation for
HIV-positive persons in Europe: results from the Collaboration of
Observational HIV Epidemiological Research Europe Study (COHERE). PLoS
Med, 2013. 10(9): p. e1001510. http://dx.doi.org/10.1371/journal.pmed.1001510
PMid:24137103 PMCid:PMC3796947

- Celesia,
B.M., et al., Late presentation of HIV infection: predictors of delayed
diagnosis and survival in Eastern Sicily. Eur Rev Med PharmacolSci,
2013. 17(16): p. 2218-24.
PMid:23893189

- Antinori,
A., et al., Italian guidelines for the use of antiretroviral agents and
the diagnostic-clinical management of HIV-1 infected persons. Update
2011. New Microbiol, 2012. 35(2): p. 113-59.
PMid:22707127

- Di
Giambenedetto, S., et al., Safety and feasibility of treatment
simplification to atazanavir/ritonavir + lamivudine in HIV-infected
patients on stable treatment with two nucleos(t)ide reverse
transcriptase inhibitors + atazanavir/ritonavir with virological
suppression (Atazanavir and Lamivudine for treatment Simplification,
AtLaS pilot study). J Antimicrob Chemother, 2013. 68(6): p. 1364-72. http://dx.doi.org/10.1093/jac/dkt007
PMid:23372058

- Rasmussen,
L.D., et al., Risk of diabetes mellitus in persons with and without
HIV: a Danish nationwide population-based cohort study. PLoS One, 2012.
7(9): p. e44575. http://dx.doi.org/10.1371/journal.pone.0044575
PMid:22984529 PMCid:PMC3440341

- Konerman,
M.A., et al., Fibrosis progression in human immunodeficiency
virus/hepatitis C virus coinfected adults: prospective analysis of 435
liver biopsy pairs. Hepatology, 2014. 59(3): p. 767-75. http://dx.doi.org/10.1002/hep.26741
PMid:24436062 PMCid:PMC3943751

- Rockstroh,
J.K., et al., Does hepatitis C viremia or genotype predict the risk of
mortality in individuals co-infected with HIV? J Hepatol, 2013. 59(2):
p. 213-20. http://dx.doi.org/10.1016/j.jhep.2013.04.005
PMid:23583272

- Sanmartín,
R., et al., Progression of liver fibrosis in HIV/hepatitis C
virus-coinfected individuals on antiretroviral therapy with early
stages of liver fibrosis at baseline. HIV Med, 2014. 15(4): p. 203-12. http://dx.doi.org/10.1111/hiv.12105
PMid:24245909

- Berenguer,
J., et al., Sustained virological response to interferon plus ribavirin
reduces non-liver-related mortality in patients coinfected with HIV and
Hepatitis C virus. Clin Infect Dis, 2012. 55(5): p. 728-36. http://dx.doi.org/10.1093/cid/cis500
PMid:22610932

- Afdhal,
N., et al., Ledipasvir and sofosbuvir for previously treated HCV
genotype 1 infection. N Engl J Med, 2014. 370(16): p. 1483-93. http://dx.doi.org/10.1056/NEJMoa1316366
PMid:24725238

- Afdhal, N.,
et al., Ledipasvir and sofosbuvir for untreated HCV genotype 1
infection. N Engl J Med, 2014. 370(20): p. 1889-98. http://dx.doi.org/10.1056/NEJMoa1402454
PMid:24725239

[TOP]