Introduction:
According to the World Health Organization (WHO), COVID-19 has become a
Public Health Emergency of International Concern (PHEIC). Understanding
patients' hematologic findings in SARS-CoV-2 infection is essential to
doing their prognosis, so adjusting care and improving outcomes.
Objective:
In this review, we aim at summarizing changes in the hematopoietic
system and hemostasis that occur in SARS-CoV-2 infected patients.
Findings:
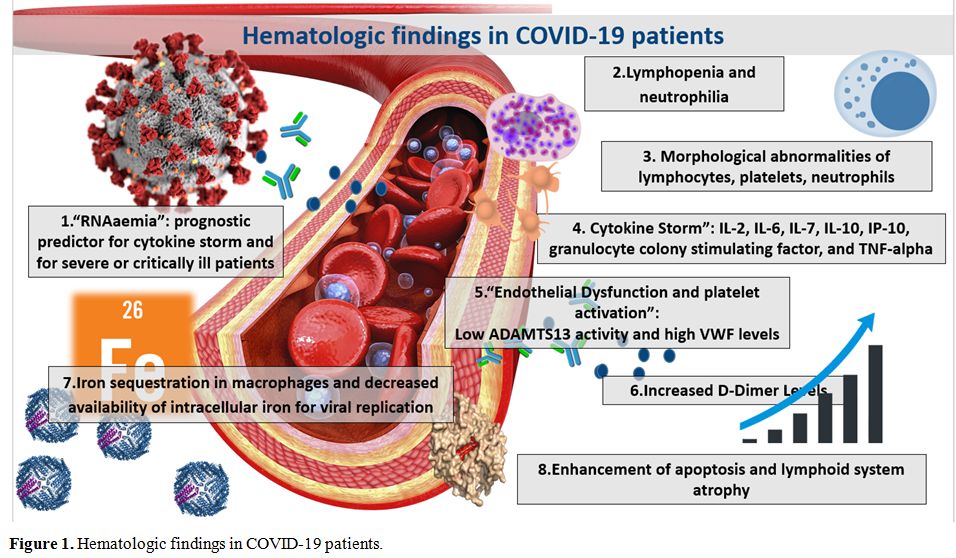
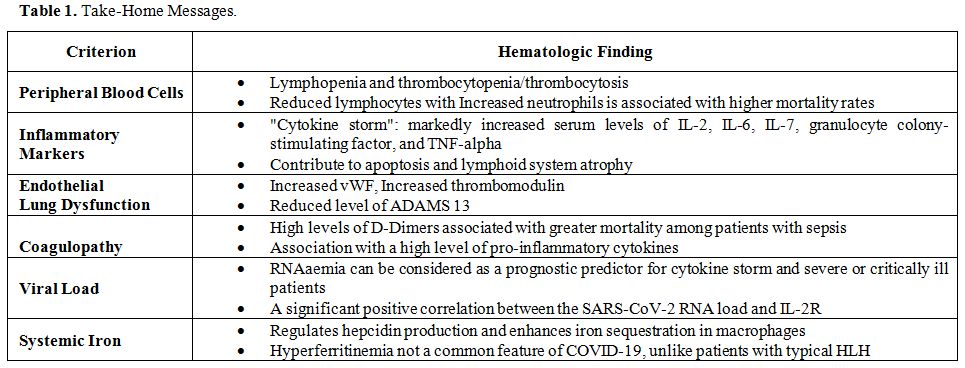
COVID-19 infection is often associated with laboratory hematologic
features that can have important clinical implications. Careful
revision of baseline hematologic data at diagnosis can predict the
severity of illness and help clinicians tailoring the approach and
management of patients whose condition can be guarded or
critical. The levels of hematologic markers like D-dimer,
procalcitonin, C-reactive protein, viral load, inflammatory cytokines,
differential blood cell count, and peripheral smear are fundamental for
the prognosis. Studies have also shown an association between some of
these markers and severe COVID-19 infection requiring admission to the
intensive care unit or complicated by acute respiratory distress
syndrome (ARDS). Since, so far, a vaccine is not available,
prevention of the infection is based on the avoiding people affected
and the spreading of the virus; the treatment, in the absence of an
effective antiviral agent, is symptomatic, and, in addition to oxygen
support, finds in the anti-inflammatory drugs and anticoagulation
fundamental therapeutic lines. According to the American Society of
Hematology (ASH), all hospitalized patients with COVID-19 should
receive pharmacologic thromboprophylaxis with LMWH.