 |
Table
1. Main relevant data of anemic patients. |
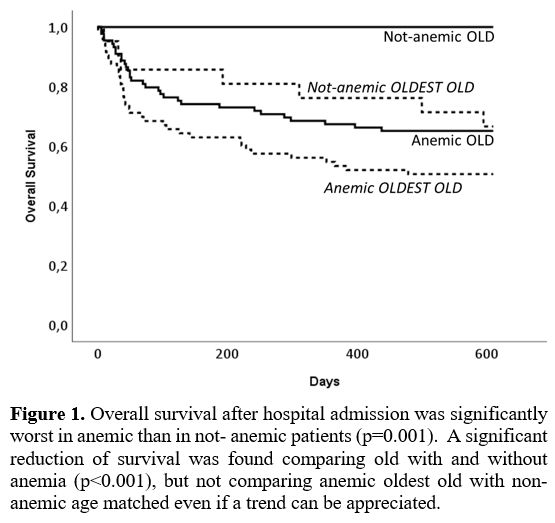
Comparing all patients together, those with anemia had shorter overall survival (p=0.001), as anemic old patients compared to those with normal hemoglobin levels (Figure 1). However, the rate of deaths in old and oldest-old anemic patients is not different.
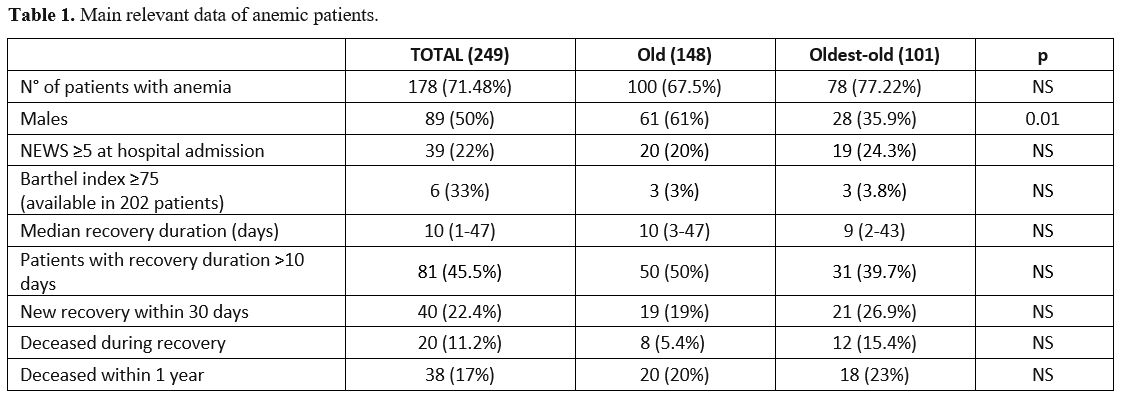
The median hemoglobin levels were not different in the two age groups, and a similar prevalence of mild and severe anemia but not of moderate anemia (p=0.01) was observed (Table 2). The most common cause of anemia was a chronic disease (38%), with no difference between old and oldest-old. In this group, 4 patients had ferritin > 100, TIBC < 20%, and sTRF > 1.76 and all had CKD. Multifactorial anemia was significantly prevalent in oldest-old (p=0.045) and hematologic neoplasms in old patients (p=0.03).
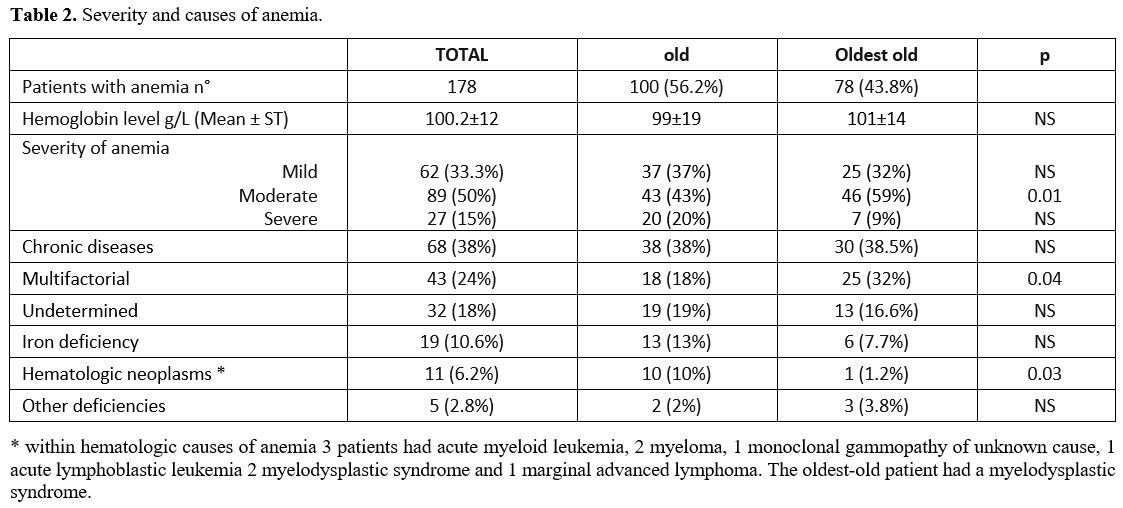 |
Table 2. Severity and causes of anemia. |
Taking together all the patients, the undetermined etiology of anemia was significantly less common in severe than in moderate (p=0.02) or mild (p=0.039) forms (Figure 2).
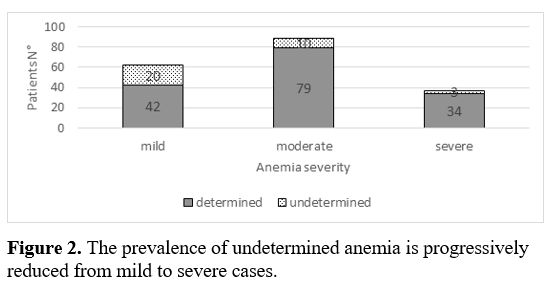 |
Figure 2. The prevalence of undetermined anemia is progressively reduced from mild to severe cases. |
When we stratified our patients on the basis of anemia severity, the prevalence of different causes of anemia were similar in the two groups of patients, excepting for multifactorial anemia (p=0.03) that was more frequent in moderate oldest-old patients compared to old (Figure 3), ferritin level of our patients did not differ comparing old and oldest-old patients. An average serum ferritin level 17.4% had clearly reduced ferritin (< 45 ug/L) and (45-250 ug/L) was found in 18.5% of patients, while 32% had ferritin higher than 250 ug/L.
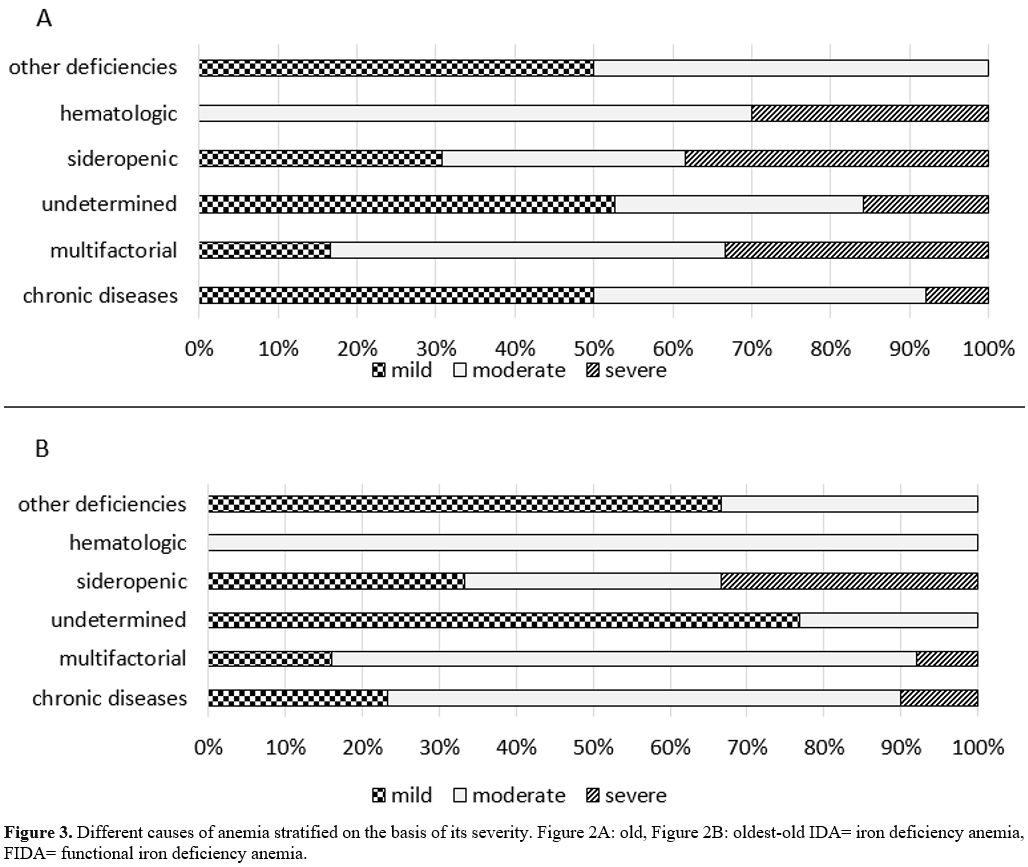 |
Figure 3. Different causes
of anemia stratified on the basis of its severity. Figure 2A: old,
Figure 2B: oldest-old IDA= iron deficiency anemia, FIDA= functional
iron deficiency anemia. |
Only thirty-five old (39.3%) and 22 oldest-old (36%) patients received treatment for anemia, in 10 cases combined (erythropoietin in 3, iron mainly i.v. in 30, vitamin B12 and folic acid in 14, blood transfusion in 22), with no difference among the old and oldest-old group.
The most common cause of admission in our cohort of patients was heart failure (30%): comparing the 28 old and the 27 oldest-old patients with heart failure, one vs. 1 had IDA, 2 vs. 1 had vitamin deficit, 8 vs. 6 had a chronic disease, 4 vs. 12 had multifactorial anemia, 6 vs. 0 a hematologic disease while in 7 vs. 8 patients had undefined anemia. We failed to observed different severity or different causes of anemia in this setting
Anemia was described in the discharging letter of 19 old (21.3%) and in 14 (22.9%) oldest-old.