Background:
A novel coronavirus that is identified as the cause of pandemic
situation in February 2020 and affects adults and children with
variable presentation and outcome.
Objective:
We studied the typical and atypical clinical and laboratory
presentation of COVID-19 during the peak of the first wave in two main
referral hospitals, upper Egypt El-Minya governorate.
Methods:
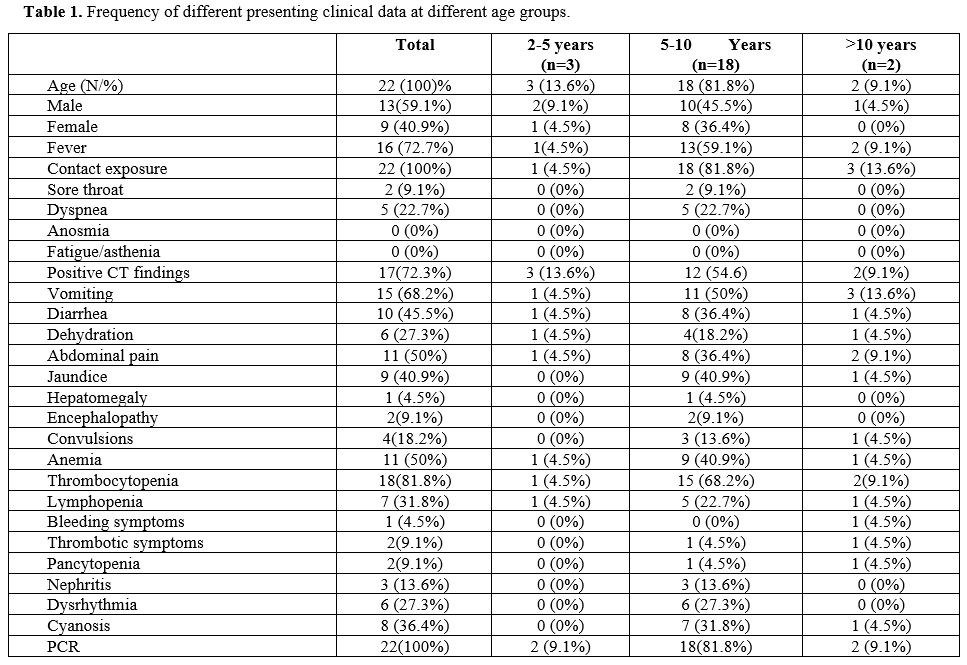
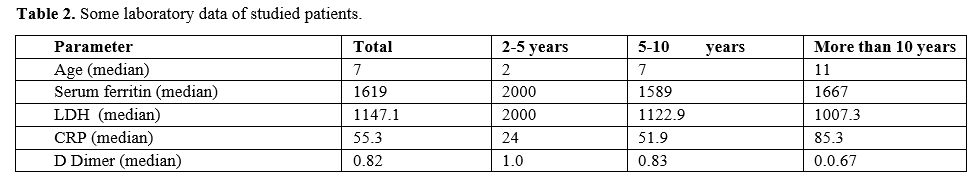
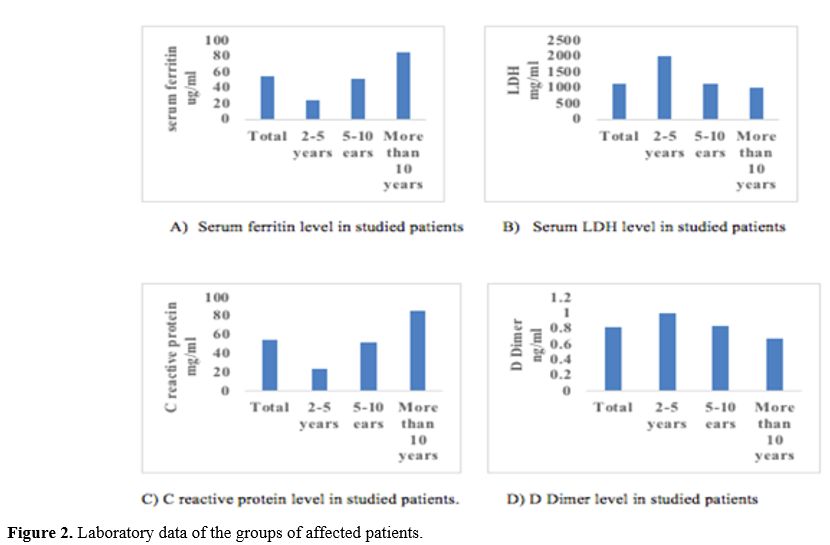
Among 88 children with suspected cases tested for COVID-19, only 22
proved to be positive. Studied patients were classified into three
groups based on age. The first group was 2–5 years, the second was 5–10
years, and the third included those aged more than 10 years. All
patients met diagnostic guidelines established by the Egyptian Ministry
of Health.
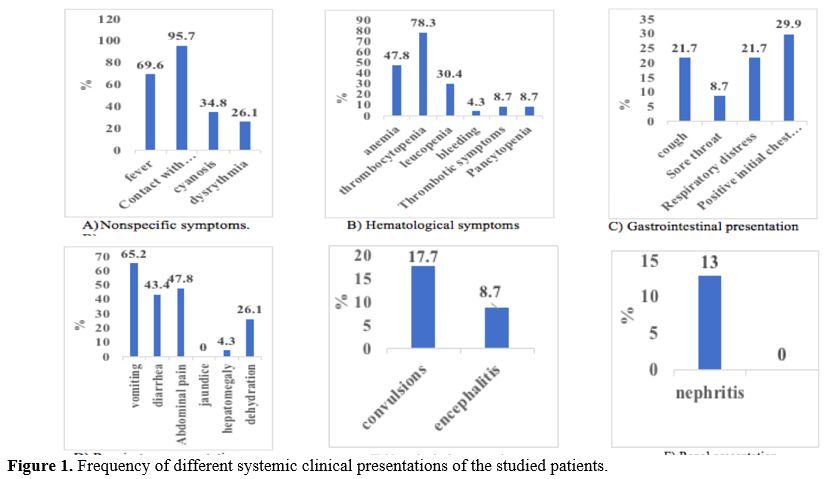
Results: out
of the positive 22 (25%) patients, 13 (59.1%) of them were male, while
9 (40.9%) were females. All enrolled patients have a history of near
contact exposure (100%). Thrombocytopenia was the highest presenting
symptom in all enrolled patients18 (81.8%), while other hematological
findings were anemia in 11 (50%), thrombotic symptoms in 2 (9.1%),
pancytopenia in 2(9.1%) while bleeding was found in 1 patient (4.5%).
Fever, present in 16 (72.7%), the most common constitutional symptom in
COVID-19, was not reported in all enrolled patients, while sore
throat was reported in only 2 patients (9.1%). The respiratory
presentation was only dominant in positive chest C.T. finding 17
(72.3%), rather than clinical symptoms; GUT symptoms were the dominant
presenting features as vomiting was found in 15 (68.2%), diarrhea in 10
(45.5%), abdominal pain in 11 (50%), jaundice in 9 (40.9%) and
dehydration in 6 (27.3%). Neurological symptoms were convulsions in 4
(18.2%), while encephalopathy was 2 (9.1%). Nephritis was the only
renal presentation in the enrolled patients, 3 (13.6%). Cardiac
presentations were only cyanosis 8 (36.4%) and arrhythmias 6 (27.3%)
Conclusion:
COVID-19 has many clinical classic presentations in children; however
other non-typical presentations like hematological, CNS, and renal
presentations have been reported.