PATHOPHISIOLOGY OF SICKLE CELL DISEASE AND NEW DRUGS FOR THE TREATMENT
Main Article Content
Keywords
Abstract
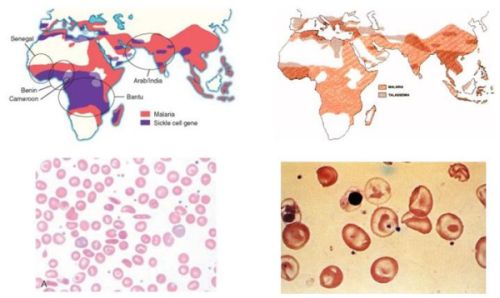
A homozygous mutation in the gene for b globin, a subunit of adult hemoglobin A (HbA), is the proximate cause of sickle cell disease (SCD). Sickle hemoglobin (HbS) shows peculiar biochemical properties, which lead to polymerizing when deoxygenated. HbS polymerization is associated with a reduction in cell ion and water content (cell dehydration), increased red cell density which further accelerate HbS polymerization. Dense, dehydrated erythrocytes are likely to undergo instant polymerization in conditions of mild hypoxia due to their high HbS concentration, and HbS polymers may be formed under normal oxygen pressure.
Pathophysiological studies have shown that the dense, dehydrated red cells may play a central role in acute and chronic clinical manifestations of sickle cell disease, in which intravascular sickling in capillaries and small vessels leads to vaso-occlusion and impaired blood flow in a variety of organs and tissue. The persistent membrane damage associated with HbS polymerization also favors the generation of distorted rigid cells and further contributes to vaso-occlusive crisis (VOCs) and cell destruction in the peripheral circulation. These damaged, dense sickle red cells also show a loss of phospholipid asymmetry with externalization of phosphatidylserine (PS), which is believed to play a significant role in promoting macrophage recognition with removal of erythrocytes (erythrophagocytosis). Vaso-occlusive events in the microcirculation result from a complex scenario involving the interactions between different cell types, including dense, dehydrated sickle cells, reticulocytes, abnormally activated endothelial cells, leukocytes, platelets and plasma factors such as cytokine and oxidized pro-inflammatory lipids.
Hydroxycarbamide (hydroxyurea) is currently the only drug approved for chronic administration in adult patients with sickle cell disease to prevent acute painful crises and reduce the incidence of transfusion and acute chest crises.
Here, we will focus on consolidated and experimental therapeutic strategies for the treatment of sickle cell disease, including:
a) agents which reduce or prevent sickle cell dehydration
b) agents which reduce sickle cell-endothelial adhesive events
c) nitric oxide (NO) or NO-related compounds
d) anti-oxidant agents
Correction of the abnormalities ranging from membrane cation transport pathways to red cell-endothelial adhesive events, might constitute new pharmacological targets for treating sickle cell disease.
Downloads
Abstract 821
PDF Downloads 595
HTML Downloads 10925