Major Artery Occlusion: a Rare Complication of Sickle Cell Disease
Adnan Agha, Mohammad Al-Hakami and Ghulam Shabbir
Department of Internal Medicine, King Fahad Hospital, Armed Forces Hospital Program Southern Region, Khamis Mushyt, P.O. Box 101, Kingdom of Saudi Arabia.
Correspondence to: Adnan Agha,
Department of Internal Medicine, King Fahad Hospital, Armed Forces
Hospital Program Southern Region, Khamis Mushyt, P.O. Box 101, Kingdom
of Saudi Arabia. E-mail: adnanagha@hotmail.com
Published: May 4, 2010
Received: April 20, 2010
Accepted: April 27, 2010
Medit J Hemat Infect Dis 2010, 2(1): e2010007, DOI 10.4084/MJHID.2010.007
This article is available from: http://www.mjhid.org/article/view/5892
This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited
Abstract
Sickle
cell disease is hereditary hemoglobinopathy which causes haemolytic
anemia, vaso-occlusive crisis, ischemic injuries and many other
morbidities like cerebral infarction. In this report, we describe
a case of a young patient with sickle cell disease presenting with
right-sided weakness and slurring of speech with examination confirming
right-sided hemiparesis with motor aphasia. On further investigation,
she was found to have frontotemporal infarction. On magnetic
resonance imaging with angiography, she was found to have absent
circulation in left internal carotid artery probably secondary to
sickle cell disease. Major vessel occlusion is rare complication
of sickle cell disease that one must bear in mind.
Introduction
Case Report
Discussion
Conclusions
Sickle
cell disease is the most common genetic hemoglobinopathy diseases
characterized by hemolytic anemia and morbidities like painful
vaso-occlusive crisis and ischemic injury. It also predisposes to
cerebral infarcts in relatively younger age. Even rarely sickle cell
disease may result in vessel occlusion. In this case report we attempt
to describe a rare case of major vessel occlusion in a young patient
with known sickle disease.
Case Report
A
22-year-old Saudi female presented to Emergency Department with a 2-day
history of right-sided weakness and slurring of speech which was sudden
in onset. Her past medical history was significant for ischemic
stroke in the left frontal region 2 years back and for having sickle
cell disease with frequent visits to hospital for vaso-occlusive
crisis. She was on regular frequent blood transfusions with last
transfusion over three months ago. Since her ischemic stroke, the
patient had been on aspirin 81 mg daily. She was vaccinated
against Streptococcus pneumoniae, Haemophilus influenzae type B,
Neisseria meningitidis, with no indications of iron overload, taking
hydroxyurea 500 mg daily and was being regularly followed up in our
sickle cell clinic. She had no history of smoking or illicit drug use.
The patient was married with one kid but she was not taking any oral
contraceptives.
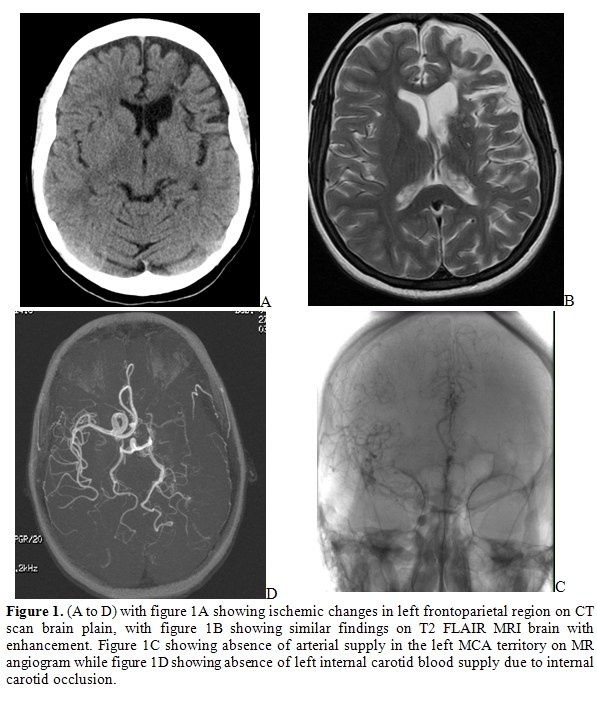
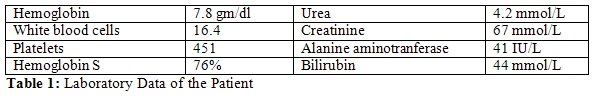
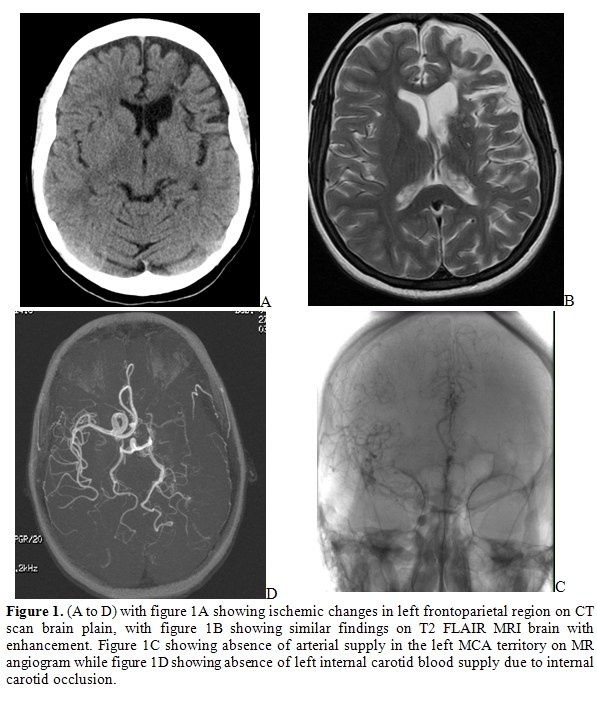
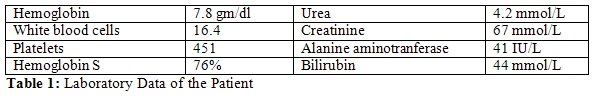
Examination revealed right-sided hemiparesis with motor aphasia. Her laboratory data is as shown in the table. CT scan showed frontotemporal ischemic changes suggestive of infarction. Suspicion for cortical venous thrombosis in light of sickle cell disease and predisposing thrombophilic tendency lead to performing an MRI Brain with angiography that revealed near absent circulation in left internal carotid artery.
Examination revealed right-sided hemiparesis with motor aphasia. Her laboratory data is as shown in the table. CT scan showed frontotemporal ischemic changes suggestive of infarction. Suspicion for cortical venous thrombosis in light of sickle cell disease and predisposing thrombophilic tendency lead to performing an MRI Brain with angiography that revealed near absent circulation in left internal carotid artery.
Discussion
Occlusion
of a major vessel like carotid artery is a rare complication of sickle
cell disease which has been reported before.[1]
Twenty-four percent of SCA patients suffer a stroke by the age of 45
which carries significant morbidity and mortality.[2]
In Saudi sickle cell population the presence of the Mediterranean G6PD
mutation (S188F) predisposes more to cerebral stroke.[3]
Sickle cell disease is an inherited disorder of hemoglobin that is among the most common genetic diseases in the world. It is characterized by lifelong hemolytic anemia and many other significant morbidities largely related to painful and debilitating vaso-occlusive phenomenon.[4] Sickle cell disease (SCD) was first described in 1910, in a dental student who presented with pulmonary symptoms.[5] Herrick coined the term “sickle-shaped” to describe the peculiar appearance of the red blood cell of this patient. However, given the patient’s symptoms, he was not sure at the time whether the blood condition was a disease sui generis or a manifestation of another disease.[6] Ingram and colleagues demonstrated shortly thereafter that the mutant sickle hemoglobin (Hb S) differed from normal hemoglobin A by a single amino acid.[7] This was followed by studies that analyzed the structure and physical properties of Hb S, which formed intracellular polymers upon deoxygenation.[8] The clinical manifestations of sickle cell anemia (SCA) result primarily from hemolytic anemia and the effects of repeated intravascular sickling, causing vasoocclusion and ischemic injury while lower levels of fetal hemoglobin (Hb F) and higher white blood cell (WBC) counts are associated with an increased incidence of SCA-related events, organ damage, and mortality.[9]
The chronic organ damage in SCA is an insidious process that may affect almost every organ system and can lead to considerable morbidity and mortality at an early age including loss of splenic function,[10] sickle nephropathy (proteinuria and renal insufficiency),[11] pulmonary hypertension,[12] and brain ischemic lesions,[13] are examples of long-term end-organ damage observed in SCA. The Stroke Prevention Trial in Sickle Cell Anemia (STOP) trial has demonstrated that the risk of stroke due to SCD is 10% per year in children not undergoing transfusion and 1% per year in children undergoing regular blood transfusion.[14,15]
Sickle cell disease is an inherited disorder of hemoglobin that is among the most common genetic diseases in the world. It is characterized by lifelong hemolytic anemia and many other significant morbidities largely related to painful and debilitating vaso-occlusive phenomenon.[4] Sickle cell disease (SCD) was first described in 1910, in a dental student who presented with pulmonary symptoms.[5] Herrick coined the term “sickle-shaped” to describe the peculiar appearance of the red blood cell of this patient. However, given the patient’s symptoms, he was not sure at the time whether the blood condition was a disease sui generis or a manifestation of another disease.[6] Ingram and colleagues demonstrated shortly thereafter that the mutant sickle hemoglobin (Hb S) differed from normal hemoglobin A by a single amino acid.[7] This was followed by studies that analyzed the structure and physical properties of Hb S, which formed intracellular polymers upon deoxygenation.[8] The clinical manifestations of sickle cell anemia (SCA) result primarily from hemolytic anemia and the effects of repeated intravascular sickling, causing vasoocclusion and ischemic injury while lower levels of fetal hemoglobin (Hb F) and higher white blood cell (WBC) counts are associated with an increased incidence of SCA-related events, organ damage, and mortality.[9]
The chronic organ damage in SCA is an insidious process that may affect almost every organ system and can lead to considerable morbidity and mortality at an early age including loss of splenic function,[10] sickle nephropathy (proteinuria and renal insufficiency),[11] pulmonary hypertension,[12] and brain ischemic lesions,[13] are examples of long-term end-organ damage observed in SCA. The Stroke Prevention Trial in Sickle Cell Anemia (STOP) trial has demonstrated that the risk of stroke due to SCD is 10% per year in children not undergoing transfusion and 1% per year in children undergoing regular blood transfusion.[14,15]
Conclusions
The idea behind this manuscript
is to highlight that major vessel occlusion causing stroke in patients
with sickle cell disease is a possibility which should be kept in mind
by emergency physicians.
References
- Tuohy AM, McKie V, Manci EA, Adams RJ.
Internal carotid artery occlusion in a child with sickle cell disease:
case report and immunohistochemical study. J Pediatr Hematol Oncol.
1997;19 :455-8

- Verduzco LA, Nathan DG. Sickle cell disease
and stroke. Blood. 2009; 114: 5117

- Hellani A, Al-Akoum S, Abu-Amero KK. G6PD
Mediterranean S188F codon mutation is common among Saudi sickle cell
patients and increases the risk of stroke. Genet Test Mol Biomarkers.
2009;13: 449-52

- Mentzer WC, Kan YW, 2001. Prospects for
research in hematologic disorders: sickle cell disease and thalassemia.
JAMA 285: 640–2.

- Herrick J.B. Peculiar elongated and
sickle-shaped red blood corpuscules in a case of severe anemia. Yale J
Biol Med. 2001 May-Jun;74(3):179-84.

- Herrick J.B. Abstract of discussion. JAMA. 1924;83:16.
- Ingram V.M. Abnormal human hemoglobins. I.
The comparison of normal human and sickle-cell haemoglobins by
fingerprinting. Biochim. Biophys. Acta. 1958;28:539-45.

- Ferrone F.A. Polymerization and sickle cell
disease: a molecular view. Microcirculation. 2004;11:115-28.

- Platt OS, Brambilla DJ, Rosse WF, et al.
Mortality in sickle cell disease. Life expectancy and risk factors for
early death. N Engl J Med. 1994;330: 1639-1644.

- Pearson HA, Spencer RP, Cornelius EA.
Functional asplenia in sickle-cell anemia. N Engl J Med. 1969;281:923-6.

- Wigfall DR, Ware RE, Burchinal MR, Kinney
TR, Foreman JW. Prevalence and clinical correlates of glomerulopathy in
children with sickle cell disease. J Pediatr. 2000;136:749-53.

- Powars D, Weidman JA, Odom-Maryon T,
Niland JC, Johnson C. Sickle cell chronic lung disease: prior morbidity
and the risk of pulmonary failure. Medicine (Baltimore). 1988;67:66-76.

- Pegelow CH, Macklin EA, Moser FG, et al.
Longitudinal changes in brain magnetic resonance imaging findings in
children with sickle cell disease. Blood. 2002;99:3014-18.

- Adams RJ. Lessons From the Stroke
Prevention Trial in Sickle Cell Anemia (STOP) Study. J Child Neurol
2000;15:344-9

- Adams RJ. Big Strokes in Small
Persons. Arch Neurol 2007;64:1567-74
