Epidemiology of Activated Protein C Resistance and Factor V Leiden Mutation in the Mediterranean Region
Mehrez M. Jadaon
Published: September 8, 2011
Received: July 11, 2011
Accepted: August 17, 2011
Mediterr J Hematol Infect Dis 2011, 3: e2011037, DOI 10.4084/MJHID.2011.037
This article is available from: http://www.mjhid.org/article/view/8811
Thrombophilia is the term given to abnormal blood coagulation condition leading to increased tendency towards coagulation (hypercoagulability status). People with hypercoagulability are at risk of developing thrombosis, especially venous thromboembolic disorders (VTE) including deep vein thrombosis (DVT) and pulmonary embolism (PE). VTE is a significant cause of morbidity and mortality in many countries with an annual incidence of 1/1000.[1-4] Many genetic and acquired risk factors for the development of VTE were identified. In fact, the WHO expert group (1996) defined thrombophilia as a tendency to develop VTE that may be genetically determined, acquired or both.[5] Genetic factors include activated protein C resistance (APC-R) associated with Factor V Leiden mutation (FVL), Prothrombin G20210A mutation associated with high levels of prothrombin, genetic deficiencies of proteins C, S and antithrombin, and others. Acquired risk factors include lupus anticoagulants, pregnancy, use of contraceptives, major surgeries, cancer, inflammations, and others. This review article focuses on the epidemiology of APC-R/FVL in the Mediterranean area. For a better understanding of the pathophysiology involved in causing hypercoagulability by APC-R/FVL, it may be helpful to start by a quick revision of the process of coagulation and its associated natural anticoagulants.
Blood Coagulation
Normally, blood loss through injured vessels is prevented by a normal physiological process called “Hemostasis”. Normal human hemostasis is a balanced system which, on one hand, prevents excessive bleeding from any injured site, while on the other hand maintains blood circulation inside intact blood vessels by inhibiting intravascular coagulation. An efficient hemostatic process possesses intrinsic well-balanced regulatory systems, involving a number of dynamic mechanisms and chemical and physical reactions. It usually includes platelets, blood vessels and the coagulation system. In blood coagulation, a prominent response to an injury is recruited in the form of series of stepwise (cascade) chemical interactions leading to fibrin formation. This complex system involves certain proteins called the plasma clotting factors (enzymes). These enzymes circulate in the blood in an inactive form, and get activated in case of vessel injury. In summary, when a blood vessel is injured, the coagulation cascade is initiated by the release of tissue factor (thromboplastin) and the exposure of intravascular collagen, which activates clotting factors VII and XII, respectively. These clotting factors activate other clotting factors in a stepwise procedure ending up with the formation of a fibrin clot. A fibrin clot, in association with platelets, form a plug that blocks the injured blood vessel, preventing bleeding and allowing for wound healing. After healing, the fibrin clot is dissolved by the enzyme plasmin in a process called fibrinolysis. The whole process is under careful supervision by three main proteins that circulate normally in the blood; namely protein C (and its active form activated protein C; APC), protein S (PS) and antithrombin (AT). These so-called “natural anticoagulants” monitor the processes of coagulation and fibrinolysis in order to prevent excessive clotting.[6-8] Abnormalities in clotting factors may lead to bleeding problems (hemophilia), while abnormalities in the natural anticoagulants may lead to hypercoagulability and thrombosis, with certain exceptions in both. Figure 1 gives an illustrative drawing of the process of coagulation and its associated fibrinolysis process and natural anticoagulants.
Activated Protein C Resistance and Factor V Leiden Mutation
In 1993, a Swedish research team led by B. Dahlbäck recognized an unusual phenomenon affecting the coagulation system. They were studying the effect of addition of external APC to plasma of patients with VTE. Normally, APC should inactivate clotting Factor V (FV) (Figure 1) and therefore slow down the coagulation process. However, in certain patients studied by Dahlbäck and his team, this slowing down did not occur. They called this phenomenon “APC resistance”, and they originally though this could be due a deficiency in a yet unknown protein that co-helps APC in inactivating FV.[9] One year later, another group of researchers from Holland, led by R. M. Bertina, discovered a missense point mutation in the FV gene, where adenine (A) replaced guanine (G) at nucleotide position 1691 of exon 10 of the FV gene, only eleven nucleotides upstream of the beginning of intron 10. They called this mutation as FV Leiden mutation (FVL) after the Dutch city where they made their discovery in.[10] This nucleotide replacement happened to be in the codon for the amino acid residue arginine 506 (CGA) normally present in the factor V molecule, creating a new codon (CAA) which is translated as glutamine. In order to inactivate FV, APC needs to recognize arginine at position 506 of the FV molecule (Figure 2). Because of the amino acid change in FVL, APC can no longer inactivate FV efficiently, but FV retains its coagulation capabilities and therefore carriers of FVL develop hypercoagulability which may clinically manifest as VTE episodes. Later studies showed that people with FVL were at higher risk of developing VTE (10-fold in heterozygous carriers and 30 to 140-fold in homozygous carriers).[9-16] In addition, most homozygotes for FVL were reported to get at least one VTE event in their life time.[17,18] This explains the great clinical and scientific consideration this mutation had appealed and the hundreds of studies conducted on its prevalence and risk for developing VTE in almost every part of the world.
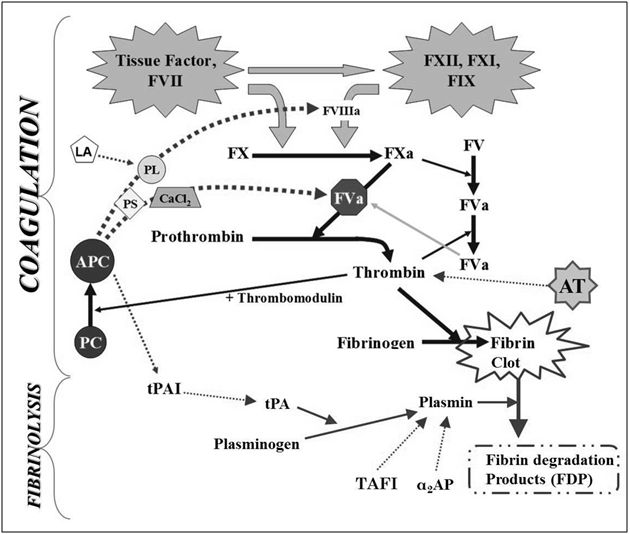
Figure 1. The processes of coagulation and fibrinolysis as a series of chemical reactions leading to the formation of a clot to stop bleeding from the site of injury, and then removing the clot afterwards. Solid lines indicate activation process, while dashed lines indicate inactivation process. Abbreviations: antithrombin (AT), protein C (PC), activated protein C (APC), protein S (PS), phospholipids (PL), lupus anticoagulants (LA), tissue plasminogen activator (tPA), tPA inhibitor (tPAI), α2 antiplasmin (α2AP), thrombin activatable fibrinolysis inhibitor (TAFI).
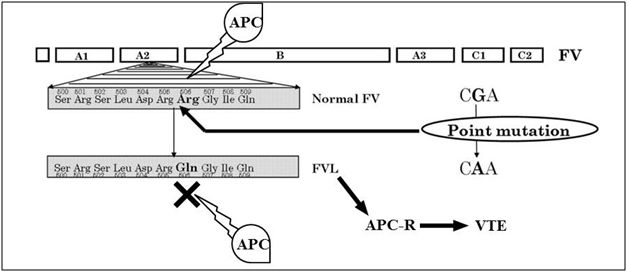
Figure 2. FV molecule showing arginine 506 as a main point of action for APC which is negatively affected by FVL.
World Distribution of Factor V Leiden
Since its discovery, several studies were conducted to determine the prevalence of FVL mutation in normal subjects and in patients with VTE, as well as to measure the risk value of this mutation in developing VTE. First reports appeared in Europe, which concentrated on populations of Caucasian origin. They found FVL to be present in a quite high percentage of patients with VTE (15-65%) and healthy subjects (1-15%). Similar results were obtained when Caucasians where studied in non-European countries like USA, Australia and Israel. Table 1 gives examples of studies on FVL in European and non-European Caucasians.[2,3,10,12,14-16,19-64] However, when studies where extended to other ethnic groups, FVL was surprisingly found to be very rare in Africans, South-East Asians, Chinese, Japanese, American Indians, Greenland Eskimos and Aboriginals of Australia (Table 2).[21,58,61,65-78] These findings suggested that FVL might have occurred as a single event sometime in the distant past in a common European Caucasian ancestor, whose offspring are the present time Caucasian carriers of this mutation living in Europe and other countries. This assumption was later strengthened by molecular studies that reported FVL to be always associated with one haplotype of single nucleotides polymorphisms (SNPs), as will be discussed later. Later on, studies were conducted on Arabs and populations living in the Middle East and North Africa (The MENA region), as summarized in Table 3.[31,63,79-133] These studies showed a high prevalence of FVL in these populations, who are not usually classified as Caucasians. However, the MENA region is geographically very close to Europe and had witnessed a lot of human movement from and to Europe, and hence such populations are expected to have some Caucasian genes in their DNA. Therefore, the presence of FVL in Arabs and North African populations should not be a surprising upshot.
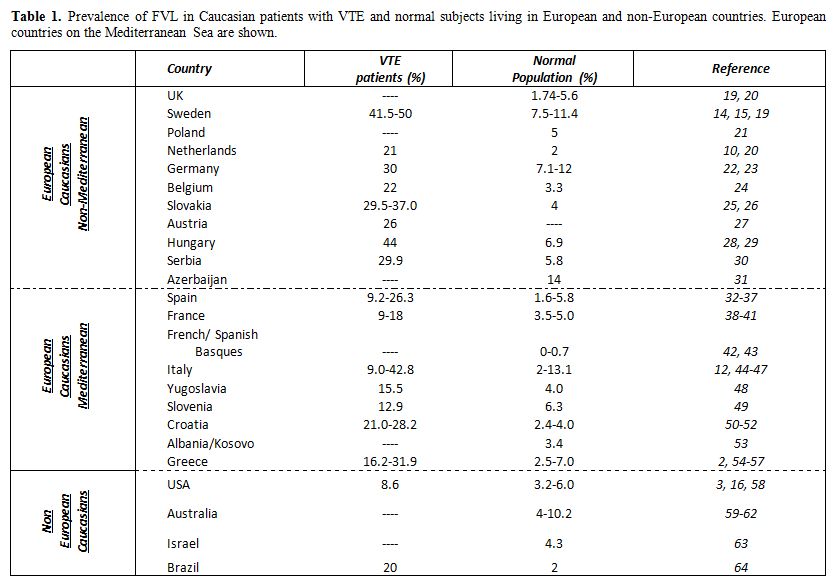
Table 1. Prevalence of FVL in Caucasian patients with VTE and normal subjects living in European and non-European countries. European countries on the Mediterranean Sea are shown.
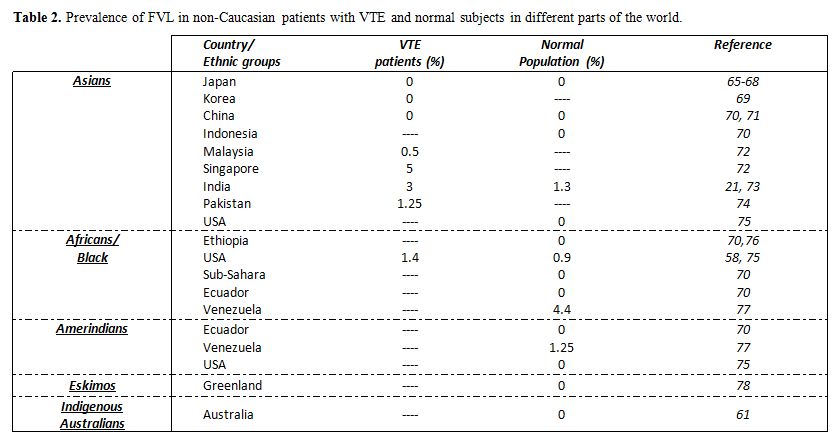
Table 2. Prevalence of FVL in non-Caucasian patients with VTE and normal subjects in different parts of the world.
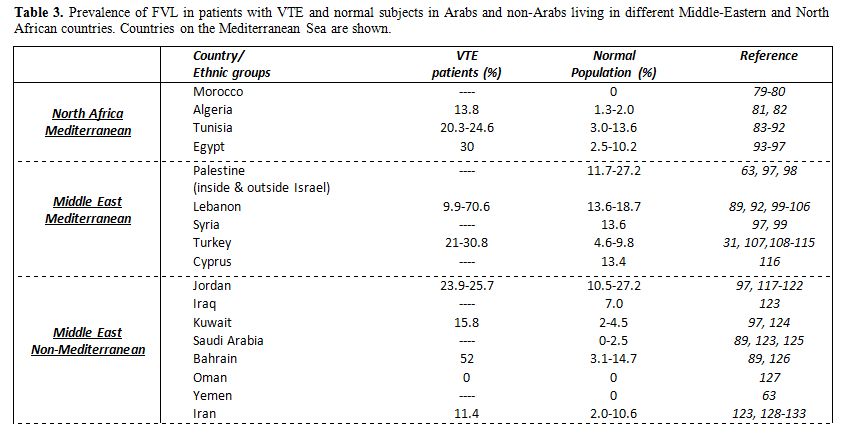
Table 3. Prevalence of FVL in patients with VTE and normal subjects in Arabs and non-Arabs living in different Middle-Eastern and North African countries. Countries on the Mediterranean Sea are shown.
Factor V Leiden in the Mediterranean Region
Currently, there are 20 countries that have seacoasts on the Mediterranean Sea and therefore are called the Mediterranean countries; 5 are in North Africa, 4 in West Asia and 11 in South Europe. Figure 3 gives a map of the Mediterranean Sea and its countries, showing the prevalence of FVL in these countries which are based on the studies listed in tables 1 and 3. No data could be retrieved from the literature on prevalence of FVL in Libya, Malta, Bosnia or Montenegro. However, one study reported FVL in Yugoslav people which included patients and healthy subjects from all over the former Yugoslavia, and possibly some of their subjects were from Bosnia and Montenegro.[48] There were no reports from Albania itself, but one study was conducted in Kosovo, the people of which are considered as Albanians.[53] In table 1, the prevalence of FVL in the people of the Basques was put separately, although not being a separate country, because of the unique rarity of FVL in these people.[42,43] This has an important issue which will be discussed later. In Israel, the population consists of a mixture of Palestinian Arabs and other immigrants from different parts of the world, largely being of European Caucasian origin. Therefore, the results there were split between tables 1 and 3 according to the origin of the studied populations.
One may notice that the prevalence of FVL is present in its maximum peak in this part of the World. In addition, there is generally an Eas-to-West decline in prevalence of FVL in these countries. This observation was also noticed by Lucotte et al (2001) who also observed a South-to-North decline of these values in Europe, only when southwestern populations were excluded.[134] These observations raised discussions in the literature on the exact place where FVL has first appeared.
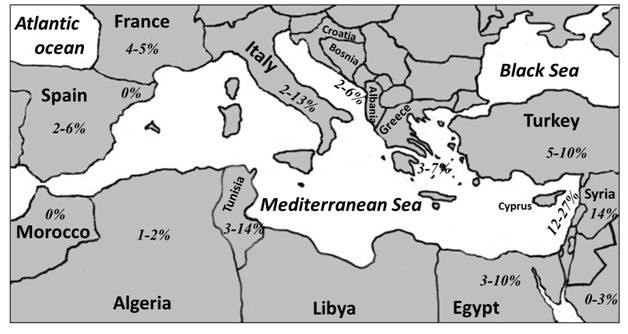
Figure 3. Map of the Mediterranean Sea and its countries showing the prevalence of FVL in healthy populations living there.
Has Factor V Leiden originated in the Eastern Mediterranean?
As was mentioned before, the first reports on the prevalence of FVL found high prevalence of FVL in European Caucasians, while the prevalence was almost zero in other ethnic groups. In addition, studies showed an association of FVL with one haplotype in all carriers of the mutation. Therefore, scientists got a perception that FVL has occurred once in the past time in one European Caucasian person. Anthropology proposes that Caucasoid populations who settled in Europe were diverted from Mongoloid populations (who moved to East Asia) around 32 thousands of years ago; therefore FVL should have appeared sometime earlier than 32,000 years ago.[2,4,11,135-137] It was suggested that the mutation occurred in Europe first, and then spread to other parts of the world. However, the observed highest prevalence of FVL in Eastern Mediterranean countries have raised speculations that FVL might have occurred somewhere there and then spread to Europe.[43,99,100,134,138,139] The author of this paper has found FVL to be associated with one haplotype in 67 Arabs from Eastern Mediterranean region, which was the same haplotype found in European carriers of the mutation, giving another confirmation that FVL occurred as a single event in the past even in Arabs. [140] Castoldi et al (1997) suggested that FVL probably occurred outside Europe.[138] The rarity of FVL in the French and Spanish Basque populations, which are thought to be the oldest ethnic groups in Europe of Paleolithic origin, has also suggested FVL to occur outside Europe first.[42,43] Lucotte et al (2001) proposed that FVL expanded in Europe during the Neolithic period, from a probable Anatolian center of origin in Turkey, which has occurred around 10,000 years ago.[134] This may explain the highest prevalence of FVL in East Mediterranean countries, and that the prevalence decreases when radiating away from this region towards Europe or other parts of the world. Still, more genetic and molecular studies may be needed to detect certain genetic loci or markers that may help in following the movement of carriers of FVL in the Mediterranean region to definitely determine the exact location where FVL might have occurred first.
Conclusions
Molecular and epidemiological studies provide evidences that FVL should have occurred as a single event in the past. The Mediterranean region has the highest prevalence of FVL in the world. This suggests it as the area where this mutation has arisen, possibly 10,000 years ago, and then it was spread to other parts of the world.
References
- Dahlbäck B. Resistance to activated protein
C, the Arg506 to Gln mutation in the factor V gene, and venous
thrombosis. Functional tests and DNA-based assays. Pros and Cons.
Thromb Haemost 73(5): 739-742, 1995. PMid:7482395

- Rees DC, Cox M and Clegg JB. World
distribution of factor V Leiden. Lancet 346(8983): 1133-1134,
1995.
http://dx.doi.org/10.1016/S0140-6736(95)91803-5

- Ridker PM, Miletich JP, Hennekens CH,
Buring JE. Ethnic distribution of Factor V Leiden in 4047 men and
women. Implications for venous thrmoboembolism screening. JAMA.
1997;277:1305-1307 http://dx.doi.org/10.1001/jama.277.16.1305

- Zivelin A, Griffin JH, Xu X, Pabinger I,
Samama M, Conard J, Brenner B, Eldor A and Seligsohn U. A single
genetic origin for a common Caucasian risk factor for venous
thrombosis. Blood 89(2): 397-402, 1997. PMid:9002940

- Lane DA, Mannucci PM, Bauer KA, Bertina RM,
Bochkov NP, Boulyjenkov V, Chandy M, Dahlbäck B, Ginter EK, Miletich
JP, Rosendaal FR, Seligsohn U. Inherited thrombophilia: Part 1. Thromb
Haemost. 76(5):651-662, 1996. PMid:8950768

- Davie EW. Biochemical and molecular aspects
of the coagulation cascade. Thromb Haemost 74(4): 1-6, 1995.PMid:8578439

- Kane WH and Davie EW. Blood coagulation
factor V and VIII: structural and functional similarities and their
relationship to haemorrhegic and thrombotic disorders. Blood 71(3):
539-555, 1988. PMid:3125864

- Kalafatis M, Rand MD, Mann KG. The
mechanism of inactivation of human factor V and human factor Va by
activated protein C. J Biol Chem. 1994;269:31869-31880. PMid:7989361

- Dahlbäck B, Carlsson M, Svensson PJ.
Familial thrombophilia due to a previously unrecognized mechanism
characterized by poor anticoagulant response to ctivated protein C:
Prediction of a cofactor to activated protein C. Proc Natl Acad Sci
USA. 1993;90:1004-1008. http://dx.doi.org/10.1073/pnas.90.3.1004

- Bertina RM, Koeleman BPC, Koster T,
Rosendaal FR, Dirven RJ, de Ronde HD, van der Velden PA and Reitsma PH.
Mutation in blood coagulation factor V associated with resistance to
activated protein C. Nature 369(6475): 64-67, 1994. http://dx.doi.org/10.1038/369064a0
PMid:8164741

- Dahlbäck B. Resistance to activated
protein C caused by the factor V R506Q mutation is a common risk factor
for venous thrombosis. Thromb Haemost. 1997;78:483-488. PMid:9198201

- Faioni EM, Razzari C, Martinelli I,
Panzeri D, Franchi F, Mannucci PM. Resistance to activated protein C in
unselected patients with arterial and venous thrombosis. Am J Hematol.
1997;55:59-64 http://dx.doi.org/10.1002/(SICI)1096-8652(199706)55:2<59::AID-AJH2>3.0.CO;2-1

- Hoagland LE, Triplett DA, Peng F, et al.
APC-resistnace as measured by a Textarin time assay: comparison to the
APTT-based method. Thromb Res. 1996;83:363-373. http://dx.doi.org/10.1016/0049-3848(96)00146-6

- Zöller B, Svensson PJ, He X, Dahlbäck B.
Identification of the same factor V gene mutation in 47 out of 50
thrombosis-prone families with inherited resistance to activated
protein C. J Clin Invest. 1994;94:2521-2524. http://dx.doi.org/10.1172/JCI117623
PMid:7989612 PMCid:330087

- Alderborn A, Siegbahn A, Wadelius C.
Venous thrombosis: factor V G1691A genetypeing related to APC
resistance measured by 2 methods. Eur J Haematol. 1997;58:229-232. http://dx.doi.org/10.1111/j.1600-0609.1997.tb01659.x

- Bontempo FA, Hassett AC, Faruki H, et al.
The factor V Leiden mutation: spectrum of thrombotic events and
laboratory evaluation. J Vasc Surg. 1997;25(2):271-275. http://dx.doi.org/10.1016/S0741-5214(97)70348-3

- Florell SR, Rodgers GM. Inherited
thrombotic disorders: An update. Am J Hematol. 1997;54:53-60. http://dx.doi.org/10.1002/(SICI)1096-8652(199701)54:1<53::AID-AJH8>3.0.CO;2-3

- Samama MM, Simon D, Horellou MH, et al.
Diagnosis and clinical characteristics of inherited activated protein C
resistance. Haemostasis. 1996;26:315-330. PMid:8979137

- Bengtsson A, Zöller B, de Frutos PG,
Dahlbäck B and Sturfelt G. Factor V:Q506 mutation and anticardiolipin
antibodies in systemic lupus erythematosus. Lupus 5(6): 598-601, 1996. http://dx.doi.org/10.1177/096120339600500607
PMid:9116703

- Beauchamp NJ, Daly ME, Hampton KK, Cooper
PC, Preston FE and Peake IR. High prevalence of a mutation in the
factor V gene within the U.K. population: relationship to activated
protein C resistance and familial thrombosis. Br J Haematol 88(1):
219-222, 1994. http://dx.doi.org/10.1111/j.1365-2141.1994.tb05005.x
PMid:7803250

- Herrmann FH, Koesling M, Schroder W,
Altman R, Jimenez Bonilla R, Lopaciuk S, Perez-Requejo JL and Singh JR.
Prevalence of factor V Leiden mutation in various populations. Genet
Epidemiol 14(4):403-11, 1997.
http://dx.doi.org/10.1002/(SICI)1098-2272(1997)14:4<403::AID-GEPI5>3.0.CO;2-3

- Aschka I, Aumann V, Bergmann F, Budde U,
Ebert W, Eckhof-Donovan S, Krey S, Nowak-Gottl U, Schobess R, Sutor AH,
Wendisch J and Schneppenheim R. Prevalence of factor V Leiden in
children with thrombo-embolism. Eur J Pediatr 155(12): 1009-1014, 1996.
http://dx.doi.org/10.1007/BF02532520
PMid:8956934

- Schröder W, Koesling M, Wulff K, Wehnert
M, Herrmann FH. Large-scale screening for factor V Leiden mutation in a
north-eastern German population. Haemostasis. 1996;26:233-6.

- Hainaut P, Azerad MA, Lehmann E, Schlit
AF, Zech F, Heusterspreute M, Philippe M, Col C, Lavenne E and Mariau
M. Prevalence of activated protein C resistance and analysis of
clinical profile in thromboembolic patients. A Belgian prospective
study. J intern Med 241(5): 427-433, 1997. http://dx.doi.org/10.1046/j.1365-2796.1997.139145000.x
PMid:9183312

- Simkova M, Batorova A, Dostalova K,
Pozgayova S, Simko F, Kovacs L. Factor V Leiden in patients with venous
thrombosis in Slovak population. Gen Physiol Biophys. 2004;23:435-442
PMid:15815078

- Hudecek J, Dobrotová M, Hybenová J,
Ivanková J, Melus V, Pullmann R, Kubisz P. Factor V Leiden and the
Slovak population. Vnitr Lek. 2003;49:845-850 PMid:14689680

- Melichart M, Kyrle PA, Eichnger S,
Rintelen C, Mannhalter C, Pabinger I. Thrombotic tendency in 75
symptomatic, unrelated patients with APC resistance. Wien Klin
Wochenschr. 1996;108:607-610 PMid:8921576

- Nagy A, Melegh B, Losonczy H. Study of the
Leiden mutation (factor VQ506), the most frequent cause of
thrombophilia, in 116 thrombosis patients. Orv Hetil.
1997;138:2797-2800 PMid:9411348

- Stankovics J, Melegh B, Nagy A, Kis A,
Molnar J, Losonczy H, Schuler A, Kosztolanyi G. Incidence of factor V
G1681A (Leiden) mutation in samplings from the Hungarian population.
Orv Hetil. 1998;139:1161-1163 PMid:9613165

- Djordjevic V, Rakicevic LJ, Mikovic D,
Kovac M, Miljic P, Radojkovic D, Savic A. Prevalence of factor V
leiden, factor V cambridge, factor II G20210A and
methylenetetrahydrofolate reductase C677T mutations in healthy and
thrombophilic Serbian populations. Acta Haematol. 2004;112:227-229. http://dx.doi.org/10.1159/000081280
PMid:15564739

- Gurgey A, Mesci L. The prevalence of
factor V Leiden (1691GA) mutation in Turkey. Turk J Pediatr.
1997;39:313-315 PMid:9339109

- Olave T, Cornudella R, Homs C, Azaceta G,
Tirado I, Gutierrez M. Incidence and clinical manifestations of
activated protein C resistance and factor V Leiden in young patients
with venous thromboembolic disease in Spain. Haematologica.
1998;83:378-80 PMid:9592991

- García-Hernández MC, Romero Casanova A,
Marco Vera P. Clinical comments on genetic marker prevalence (factor V
Leiden, prothrombin 20210A and homozygous methylenetetrahydrofolate
reductase form [Ho-MTHFR]): based on a study conducted in Health
Department No. 19 of the Valencian Community. Rev Clin Esp.
2007;207:26-28. PMid:17306151

- Aznar J, Vayá A, Estellés A, Mira Y, Seguí
R, Villa P, Ferrando F, Falcó C, Corella D, España F. Risk of venous
thrombosis in carriers of the prothrombin G20210A variant and factor V
Leiden and their interaction with oral contraceptives. Haematologica.
2000;85:1271-1276 PMid:11114134

- González Ordóñez AJ, Medina Rodriguez JM,
Martín L, Alvarez V, Coto E. The O blood group protects against venous
thromboembolism in individuals with the factor V Leiden but not the
prothrombin (factor II G20210A) mutation. Blood Coagul Fibrinolysis.
1999; 10: 303-307 http://dx.doi.org/10.1097/00001721-199907000-00013

- Vargas M, Soto I, Pinto CR, Urgelles MF,
Batalla A, Rodriguez-Reguero J, Cortina A, Alvarez V, Coto E. The
prothrombin 20210A allele and the factor V Leiden are associated with
venous thrombosis but not with early coronary artery disease. Blood
Coagul Fibrinolysis. 1999;10:39-41 http://dx.doi.org/10.1097/00001721-199901000-00006

- Ricart JM, Vayá A, Todolí J, Calvo J,
Villa P, Estellés A, España F, Santaolaria M, Corella D, Aznar J.
Thrombophilic risk factors and homocysteine levels in Behçet's disease
in eastern Spain and their association with thrombotic events. Thromb
Haemost. 2006;95(4):618-624 PMid:16601831

- Leroyer C, Mercier B, Escoffre M, Ferec C,
Mottier D. Factor V Leiden prevalence in venous thromboembolism
patients. Chest 1997;111: 1603-1606
http://dx.doi.org/10.1378/chest.111.6.1603 PMid:9187182

- Mansourati J, Da Costa A, Munier S,
Mercier B, Tardy B, Ferec C, Isaaz K, Blanc JJ. Prevalence of factor V
Leiden in patients with myocardial infarction and normal coronary
angiography. Thromb Haemost. 2000;83:822-825 PMid:10896232

- Meyer G, Emmerich J, Helley D, Arnaud E,
Nicaud V, Alhenc-Gelas M, Aiach M, Fischer A, Sors H, Fiessinger JN.
Factors V leiden and II 20210A in patients with symptomatic pulmonary
embolism and deep vein thrombosis. Am J Med. 2001;110:12-15 http://dx.doi.org/10.1016/S0002-9343(00)00653-7

- Mazoyer E, Ripoll L, Gueguen R, Tiret L,
Collet JP, dit Sollier CB, Roussi J, Drouet L; FITENAT Study Group.
Prevalence of factor V Leiden and prothrombin G20210A mutation in a
large French population selected for nonthrombotic history:
geographical and age distribution. Blood Coagul Fibrinolysis.
2009;20(7):503-510 http://dx.doi.org/10.1097/MBC.0b013e32832f5d7a

- Bauder F, Ducout L, Guerre C, Freyburger
G. Activated protein C (APC) resistance: does it exist in Basques? Br J
Haematol. 1997;99(3):712-713 PMid:9401095

- Zabalegui N, Montes R, Orbe J, Ayape ML,
Medarde A, Páramo JA, Rocha E. Prevalence of FVR506Q and prothrombin
20210A mutations in the Navarrese population. Thromb Haemost.
1998;80:522-523 PMid:9759640

- Simioni P, Prandoni P, Lensing AW,
Scudeller A, Sardella C, Prims MH, Villatta S, Dazzi F, Girolami A. The
risk of recurrent venous thromboembolism in patients with an Arg506G
mutation in the gene for factor V (factor V Leiden). N Engl J Med.
1997; 336:399-403 http://dx.doi.org/10.1056/NEJM199702063360602
PMid:9010145

- Sottilotta G, Mammì C, Furlò G, Oriana V,
Latella C, Trapani Lombardo V. High incidence of factor V Leiden and
prothrombin G20210A in healthy southern Italians. Clin Appl Thromb
Hemost. 2009;15:356-359

- Gessoni G, Valverde S, Canistro R, Manoni
F. Factor V Leiden in Chioggia: a prevalence study in patients with
venous thrombosis, their blood relatives and the general population.
Blood Transfus. 2010;8:193-195 PMid:20671880 PMCid:2906187

- Martinelli I, Battaglioli T, Bucciarelli
P, Passamonti SM, Mannucci PM. Risk factors and recurrence rate of
primary deep vein thrombosis of the upper extremities. Circulation.
2004;110:566-570 http://dx.doi.org/10.1161/01.CIR.0000137123.55051.9B
PMid:15262837

- Mikovic D, Rakicevic L, Kovac M,
Radojkovic D. Prevalence of factor V Leiden mutation in Yugoslav
thrombophilic patients and its relationship to the laboratory diagnosis
of APC resistance. Thromb Haemost. 2000;84:723-724 PMid:11057877

- Bedencic M, Bozic M, Peternel P, Stegnar
M. Major and potential prothrombotic genotypes in patients with venous
thrombosis and in healthy subjects from Slovenia. Pathophysiol Haemost
Thromb. 2008;36:58-63 PMid:19127083

- Cikes V, Abaza I, Krzelj V, Terzić IM,
Tafra R, Trlaja A, Marusić E, Terzić J. Prevalence of factor V Leiden
and G6PD 1311 silent mutations in Dalmatian population. Arch Med Res.
2004;35:546-548 http://dx.doi.org/10.1016/j.arcmed.2004.07.005
PMid:15631882

- Coen D, Zadro R, Honović L, Banfić L,
Stavljenić Rukavina A. Prevalence and association of the factor V
Leiden and prothrombin G20210A in healthy subjects and patients with
venous thromboembolism. Croat Med J. 2001;42:488-492 PMid:11471205

- Jukic I, Bingulac-Popovic J, Dogic V,
Babic I, Culej J, Tomicic M, Vuk T, Sarlija D, Balija M. ABO blood
groups and genetic risk factors for thrombosis in Croatian population.
Croat Med J. 2009;50:550-558 http://dx.doi.org/10.3325/cmj.2009.50.550
PMCid:2802088

- Mekaj Y, Zhubi B, Hoxha H, Belegu R, Mekaj
A, Miftari E, Belegu M. Prevalence of resistence to activated protein C
(APC-resistance) in blood donors in Kosovo. Bosn J Basic Med Sci.
2009;9:329-334 PMid:20002000

- Hatzaki A, Anagnostopoulou E,
Metaxa-Mariatou V, Melissinos C, Philalithis P, Iliadis K, Kontaxis A,
Liberatos K, Pangratis N, Nasioulas G. The impact of heterozygosity for
the factor V Leiden and factor II G20210A mutations on the risk of
thrombosis in Greek patients. Int Angiol. 2003;22:79-82 PMid:12771861

- Ioannou HV, Mitsis M, Eleftheriou A,
Matsagas M, Nousias V, Rigopoulos C, Vartholomatos G, Kappas AM. The
prevalence of factor V Leiden as a risk factor for venous
thromboembolism in the population of North-Western Greece. Int Angiol.
2000;19:314-318 PMid:11305729

- Antoniadi T, Hatzis T, Kroupis C,
Economou-Petersen E, Petersen MB. Prevalence of factor V Leiden,
prothrombin G20210A, and MTHFR C677T mutations in a Greek population of
blood donors. Am J Hematol. 1999;61:265-267 http://dx.doi.org/10.1002/(SICI)1096-8652(199908)61:4<265::AID-AJH8>3.0.CO;2-#

- Lambropoulos AF, Foka Z, Makris M, Daly M,
Kotsis A, Makris PE. Factor V Leiden in Greek thrombophilic patients:
relationship with activated protein C resistance test and levels of
thrombin-antithrombin complex and prothrombin fragment 1 + 2. Blood
Coagul Fibrinolysis. 1997;8:485-489 http://dx.doi.org/10.1097/00001721-199711000-00001

- Limdi NA, Beasley TM, Allison DB, Rivers
CA, Acton RT. Racial differences in the prevalence of Factor V Leiden
mutation among patients on chronic warfarin therapy. Blood Cells Mol
Dis. 2006;37:100-106 http://dx.doi.org/10.1016/j.bcmd.2006.06.003
PMid:16889993 PMCid:1829476

- Aboud MR, Ma DD. A comparrision between
two activated protein C resistance methods as routine diagnostic tests
for factor V Leiden mutation. Br J Haematol. 1997; 97:798-803 http://dx.doi.org/10.1046/j.1365-2141.1997.1432958.x
PMid:9217178

- Gibson CS, MacLennan AH, Rudzki Z, Hague
WM, Haan EA, Sharpe P, Priest K, Chan A, Dekker GA; South Australian
Cerebral Palsy Research Group. The prevalence of inherited
thrombophilias in a Caucasian Australian population. Pathology.
2005;37:160-163 http://dx.doi.org/10.1080/00313020500058250
PMid:16028846

- Bennett JA, Palmer LJ, Musk AW, Erber WN.
Prevalence of factor V Leiden and prothrombin 20210A mutations in
indigenous Australians. Thromb Haemost. 2001;86:1592-1593 PMid:11776339

- Gibson CS, MacLennan AH, Rudzki Z, Hague
WM, Haan EA, Sharpe P, Priest K, Chan A, Dekker GA; South Australian
Cerebral Palsy Research Group. The prevalence of inherited
thrombophilias in a Caucasian Australian population. Pathology.
2005;37:160-163 http://dx.doi.org/10.1080/00313020500058250
PMid:16028846

- Rosen E, Renbaum P, Heyd J, Levy-Lahad E.
High frequency of factor V Leiden in a population of Israeli Arabs.
Thromb Haemost. 1999;82:1768 PMid:10613668

- Arruda VR, Annichino-Bizzacchi JM, Costa
FF, Reitsma PH. Factor V Leiden (FVQ 506) is common in a Brazilian
population. Am J Hematol. 1995;49:242-243 http://dx.doi.org/10.1002/ajh.2830490312
PMid:7604818

- Zama T, Murata M, Ono F, Watanabe K,
Watanabe R, Moriki T, Yokoyama K, Tokuhira M, Ikeda Y. Low prevalence
of activated protein C resistance and coagulation factor V Arg506 to
Gln mutation among Japanese patients with various forms of thrombosis,
and normal individuals. Int J Hematol. 1996;65:71-78 http://dx.doi.org/10.1016/S0925-5710(96)00527-0

- Fujimura H, Kambayashi J, Monden M, Kato
H, Miyata T. Coagulation factor V Leiden mutation may have a racial
background. Thromb Haemost. 1995;74:1381-1382 PMid:8607128

- Kodaira H, Ishida F, Scimodaira S,
Takamiya O, Furihata K, Kitano K. Resistance to activated protein C and
Arg506Gln factor V mutation are uncommon in eastern Asian populations.
Acta Haematol. 1997; 98:22-25 http://dx.doi.org/10.1159/000203548
PMid:9210909

- Ro A, Hara M, Takada A. The Factor V
Leiden and the Prothrombin G20210A mutation was not found in Japanese
patients with pulmonary thromboembolism. Thromb Haemost. 1999;82:1769

- Kim TW, Kim WK, Lee JH, Kim SB, Kim SW,
Suh C, Lee KH, Lee JS, Seo EJ, Chi HS, Kim SH. Low prevalence of
activated protein C resistance and coagulation factor V Arg506 to Gln
mutation among Korean patients with deep vein thrombosis. J Korean Med
Sci. 1998;13:587-590 PMid:9886165 PMCid:3054550

- Pepe G, Rickards O, Vanegas OC, Brunelli
T, Gori AM, Giusti B, Attanasio M, Prisco D, Gensini GF, Abbate R.
Prevalence of factor V Leiden mutation in non-European populations.
Thromb Haemost. 1997;77:329-331 PMid:9157591

- Ho CH, Chau WK, Hsu HC, Gau JP, Chih CM. Prevalence of factor V Leiden in the Chinese population. Zhonghua Yi Xue Za Zhi. 1999;62:875-878
- Lim LC, Tan HH, Lee LH, Tien SL, Abdul
Ghafar A. Activated protein C resistance: a study among 60
thromboembolic patients in the Singapore population. Ann Acad Med
Singapore. 1999;28:252-255 PMid:10497677

- Ghosh K, Shetty S, Madkaikar M, Pawar A,
Nair S, Khare A, Pathare A, Jijina F, Mohanty D. Venous thromboembolism
in young patients from western India: a study. Clin Appl Thromb Hemost.
2001;7:158-165 http://dx.doi.org/10.1177/107602960100700214
PMid:11292195

- Nasiruddin, Zahur-ur-Rehman, Anwar M,
Ahmed S, Ayyub M, Ali W. Frequency of factor V leiden mutation. J Coll
Physicians Surg Pak. 2005;15:15-17 PMid:15670517

- Gregg JP, Yamane AJ, Grody WW. Prevalence
of the factor V-Leiden mutation in four distinct American ethnic
populations. Am J Med Genet. 1997;73:334-336 http://dx.doi.org/10.1002/(SICI)1096-8628(19971219)73:3<334::AID-AJMG20>3.0.CO;2-J

- Abdulkadir J, Feleke Y, Berg JP, Falch JA
and Odegaard OR. Absence of the factor V Leiden mutation in Ethiopians.
Thromb Res. 1997;86:431-432 PMid:9211636

- Vizcaino G, Torres E, Quintero J, Herrmann
F, Grimm R, Diez-Ewald M, Arteaga-Vizcaino M, Perez-Requejo JL,
Colina-Araujo J. Prevalence of the activated protein C resistance in
indigenous and Black populations of the western Venezuela. Invest Clin.
2000;41:29-36 PMid:10758697

- De Maat MPM, Kluft C, Jespersen J, Gram J.
World distribution of factor V Leiden mutation. Lancet. 1996;347:58 http://dx.doi.org/10.1016/S0140-6736(96)91590-1

- Mathonnet F, Nadifi S, Serazin-Leroy V,
Dakouane M, Giudicelli Y. Absence of factor V Leiden mutation and low
prothrombin G 20210 A mutation prevalence in a healthy Moroccan
population. Thromb Haemost. 2002;88:1073-1074 PMid:12529766

- They-They TP, Hamzi K, Moutawafik MT,
Bellayou H, El Messal M, Nadifi S. Prevalence of angiotensin-converting
enzyme, methylenetetrahydrofolate reductase, Factor V Leiden,
prothrombin and apolipoprotein E gene polymorphisms in Morocco. Ann Hum
Biol. 2010;37:767-777 http://dx.doi.org/10.3109/03014461003738850
PMid:20687780

- Chafa O, Reghis A, Aubert A, Fischer AM.
Prevalence of the FVQ506 (factor V Leiden) mutation in the normal and
thrombophilic Algerian population. Br J Haematol. 1997;97:688-689
PMid:9207426

- Bourouba R, Houcher B, Djabi F, Egin Y,
Akar N. The prevalence of methylenetetrahydrofolate reductase 677 C-T,
factor V 1691 G-A, and prothrombin 20210 G-A mutations in healthy
populations in Setif, Algeria. Clin Appl Thromb Hemost. 2009;15:529-534
http://dx.doi.org/10.1177/1076029608319944
PMid:18840629

- Frere C, Saut N, Boukef MK, Zili M, Toumi
NE. Factor V Leiden G1691A and prothrombin G20210A mutations are common
in Tunisia. J Thromb Haemost 2003;1:2451-2452 http://dx.doi.org/10.1046/j.1538-7836.2003.0468b.x
PMid:14629484

- Bouaziz L, Hezard N, Touhami M, Potron G,
N'siri B, Nguyen P. Allelic frequency of the factor V Leiden mutation
and of the pro-thrombin gene 20210A mutation in healthy Tunisian
population. Thromb Haemost. 2004;91:824-825 PMid:15045148

- Ajem A, Slama A, Slama FB, Mehjoub T.
Prevalence of factor V leiden mutation in patients with thrombosis in
Tunisia. East Mediterr Health J. 2009;15:1483-1488 PMid:20218141

- Maalej L, Hadjkacem B, Ben Amor I, Smaoui M, Gargouri A, Gargouri J. Prevalence of factor V Leiden in south Tunisian blood donors. J Thromb Thrombolysis. 2011 [Epub ahead of print]
- Zammiti W, Mtiraoui N, Mercier E, Abboud
N, Saidi S, Mahjoub T, Almawi WY, Gris JC. Association of factor V gene
polymorphisms (Leiden; Cambridge; Hong Kong and HR2 haplotype) with
recurrent idiopathic pregnancy loss in Tunisia. A case-control study.
Thromb Haemost. 2006;95:612-617. PMid:16601830

- Mtiraoui N, Borgi L, Hizem S, Nsiri B,
Finan RR, Gris JC, Almawi WY, Mahjoub T. Prevalence of antiphospholipid
antibodies, factor V G1691A (Leiden) and prothrombin G20210A mutations
in early and late recurrent pregnancy loss. Eur J Obstet Gynecol Reprod
Biol. 2005;119:164-170. http://dx.doi.org/10.1016/j.ejogrb.2004.07.003

- Almawi WY, Keleshian SH, Borgi L, Fawaz
NA, Abboud N, Mtiraoui N, Mahjoub T. Varied prevalence of factor V
G1691A (Leiden) and prothrombin G20210A single nucleotide polymorphisms
among Arabs. J Thromb Thrombolysis. 2005;20:163-168 http://dx.doi.org/10.1007/s11239-005-3550-4
PMid:16261289

- Klai S, Fekih-Mrissa N, Rachdi R, Gritli
N. The status of thrombophilic defects and non-O blood group as risk
factors for gestational vascular complications among Tunisian women.
Acta Haematol. 2011;125:115-120 http://dx.doi.org/10.1159/000321934
PMid:21109732

- Bouaziz-Borgi L, Nguyen P, Hezard N,
Musharrafieh U, Almawi WY, Mahjoub T. A case control study of deep
venous thrombosis in relation to factor V G1691A (Leiden) and A4070G
(HR2 Haplotype) polymorphisms. Exp Mol Pathol. 2007;83:480-483. http://dx.doi.org/10.1016/j.yexmp.2007.04.006
PMid:17555744

- Bouaziz-Borgi L, Almawi WY, Mtiraoui N,
Nsiri B, Keleshian SH, Kreidy R, Louzir B, Hezard N, Mahjoub T.
Distinct association of factor V-Leiden and prothrombin G20210A
mutations with deep venous thrombosis in Tunisia and Lebanon. Am J
Hematol. 2006;81:641-643. http://dx.doi.org/10.1002/ajh.20582
PMid:16823828

- El-Karaksy H, El-Koofy N, El-Hawary M,
Mostafa A, Aziz M, El-Shabrawi M, Mohsen NA, Kotb M, El-Raziky M,
El-Sonoon MA, A-Kader H. Prevalence of factor V Leiden mutation and
other hereditary thrombophilic factors in Egyptian children with portal
vein thrombosis: results of a single-center case-control study. Ann
Hematol. 2004;83:712-715 http://dx.doi.org/10.1007/s00277-004-0921-4
PMid:15309526

- Abu-Skeen IA, Mohamed AA, Moustafa NN,
Badawy ME. Factor V Leiden and prothrombin G20210A gene mutations in
women with a history of thrombosis during pregnancy. Relation to
pregnancy outcomes for mother and fetus. Saudi Med J. 2010;31:123-129
PMid:20174725

- Maher MM, Soloma SH. Assessment of
thrombophilic abnormalities during the active state of inflammatory
bowel disease. Saudi J Gastroenterol. 2008;14:192-197 http://dx.doi.org/10.4103/1319-3767.41743
PMid:19568537 PMCid:2702936

- Settin A, Dowaidar M, El-Baz R,
Abd-Al-Samad A, El-Sayed I, Nasr M. Frequency of factor V Leiden
mutation in Egyptian cases with myocardial infarction. Hematology.
2008;13:170-174. http://dx.doi.org/10.1179/102453308X316158
PMid:18702875

- Dashti AA, Jadaon MM, Lewis HL. Factor V
Leiden mutation in Arabs in Kuwait by real-time PCR: different values
for different Arabs. J Hum Genet. 2010;55:232-235 http://dx.doi.org/10.1038/jhg.2010.11
PMid:20224595

- Hussein AS, Darwish H, Shelbayeh K.
Association between factor V Leiden mutation and poor pregnancy
outcomes among Palestinian women. Thromb Res. 2010;126:e78-82. http://dx.doi.org/10.1016/j.thromres.2010.04.017
PMid:20605623

- Irani-Hakime N, Tamim H, Elias G, Finan
RR, Daccache JL, Almawi WY. High prevalence of factor V mutation
(Leiden) in the Eastern Mediterranean. Clin Chem. 2000;46:134-136
PMid:10620589

- Taher A, Khalil I, Shamseddine A,
El-Ahdab F, Bazarbachi A. High prevalence of Factor V Leiden mutation
among healthy individuals and patients with deep venous thrombosis in
Lebanon: is the eastern Mediterranean region the area of origin of this
mutation? Thromb Haemost. 2001;86:723-724 PMid:11522037

- Tamim H, Finan RR, Almawi WY. Prevalence
of two thrombophilia predisposing mutations: factor V G1691A (R506Q;
Leiden) and prothrombin G20210A, among healthy Lebanese. Thromb
Haemost. 2002;88:691-692 PMid:12362248

- Finan RR, Tamim H, Ameen G, Sharida HE,
Rashid M and Almawi WY. Prevalence of factor V G1691A (factor V-Leiden)
and prothrombin G20210A gene mutations in a recurrent miscarriage
population. Am J Hematol. 2002;71:300-305 http://dx.doi.org/10.1002/ajh.10223
PMid:12447960

- Isma'eel H, Arnaout MS, Shamseddeen W,
Mahfouz R, Zeineh N, Jradi O, Taher A. Screening for inherited
thrombophilia might be warranted among Eastern Mediterranean
sickle-beta-0 thalassemia patients. J Thromb Thrombolysis.
2006;22:121-123 http://dx.doi.org/10.1007/s11239-006-8953-3
PMid:17008978

- Zahed LF, Rayes RF, Mahfouz RA, Taher AT,
Maarouf HH, Nassar AH. Prevalence of factor V Leiden, prothrombin and
methylene tetrahydrofolate reductase mutations in women with adverse
pregnancy outcomes in Lebanon. Am J Obstet Gynecol.
2006;195:1114-1118 http://dx.doi.org/10.1016/j.ajog.2006.06.082
PMid:17000243

- Isma'eel H, El Accaoui R, Shamseddeen W,
Taher A, Alam S, Mahfouz R, Arnaout MS. Genetic thrombophilia in
patients with VTE in eastern Mediterranean located tertiary care
center; is it time to change the algorithm for thrombophilia work up
decision making? J Thromb Thrombolysis. 2006;21:267-270 http://dx.doi.org/10.1007/s11239-006-5537-1
PMid:16683219

- Irani-Hakime N, Tamim H, Elias G,
Choueiry S, Kreidy R, Daccache JL, Almawi WY. Factor V R506Q
mutation-Leiden: an independent risk factor for venous thrombosis but
not coronary artery disease. J Thromb Thrombolysis. 2001;11:111-1116 http://dx.doi.org/10.1023/A:1011268531377
PMid:11406725

- Irdem A, Devecioglu C, Batun S, Soker M,
Sucakli IA. Prevalence of factor V Leiden and prothrombin G20210A gene
mutation. Saudi Med J. 2005;26:580-583 PMid:15900364

- Diz-Kucukkaya R, Hancer VS, Artim-Esen B,
Pekcelen Y, Inanc M. The prevalence and clinical significance of
inherited thrombophilic risk factors in patients with antiphospholipid
syndrome. J Thromb Thrombolysis. 2010;29:303-309 http://dx.doi.org/10.1007/s11239-009-0356-9
PMid:19504051

- Celiker G, Can U, Verdi H, Yazici AC,
Ozbek N, Atac FB. Prevalence of thrombophilic mutations and ACE I/D
polymorphism in Turkish ischemic stroke patients. Clin Appl Thromb
Hemost. 2009;15:415-420 http://dx.doi.org/10.1177/1076029608315163
PMid:18387982

- Oguzulgen IK, Yilmaz E, Demirtas S,
Erkekol FO, Ekim N, Demir N, Numanoglu N, Ozel D, Ulu A, Akar N. The
role of plasminogen activator inhibitor-1 polymorphism,
factor-V-Leiden, and prothrombin-20210 mutations in pulmonary
thromboembolism. Clin Appl Thromb Hemost. 2009;15:73-77 http://dx.doi.org/10.1177/1076029607305110
PMid:18160588

- Kabukcu S, Keskin N, Keskin A, Atalay E.
The frequency of factor V Leiden and concomitance of factor V Leiden
with prothrombin G20210A mutation and methylene tetrahydrofolate
reductase C677T gene mutation in healthy population of Denizli, Aegean
region of Turkey. Clin Appl Thromb Hemost. 2007;13:166-171 http://dx.doi.org/10.1177/1076029606298990
PMid:17456626

- Kalkanli S, Ayyildiz O, Tiftik N, Batun
S, Isikdogan A, Ince H, Tekes S, Muftuoglu E. Factor V Leiden mutation
in venous thrombosis in southeast Turkey. Angiology. 2006;57:193-196 http://dx.doi.org/10.1177/000331970605700209
PMid:16518527

- Atasay B, Arsan S, Günlemez A, Kemahli S,
Akar N.Factor V Leiden and prothrombin gene 20210A variant in neonatal
thromboembolism and in healthy neonates and adults: a study in a single
center. Pediatr Hematol Oncol. 2003;20:627-634 PMid:14578033

- Gurgey A, Haznedaroglu IC, Egesel T,
Buyukasik Y, Ozcebe OI, Sayinalp N, Dundar SV, Bayraktar Y. Two common
genetic thrombotic risk factors: factor V Leiden and prothrombin
G20210A in adult Turkish patients with thrombosis. Am J Hematol.
2001;67:107-111 http://dx.doi.org/10.1002/ajh.1087
PMid:11343382

- Ozbek U, Tangün Y. Frequency of factor V
Leiden in Turkey. Int J Hematol. 1996;64:291-292 http://dx.doi.org/10.1016/0925-5710(96)00499-9

- Angelopoulou K, Nicolaides A,
Constantinou Deltas C. Prevalence of genetic mutations that predispose
to thrombophilia in a Greek Cypriot population. Clin Appl Thromb
Hemost. 2000;6:104-107 http://dx.doi.org/10.1177/107602960000600211
PMid:10775032

- Eid SS, Rihani G. Prevalence of factor V
Leiden, prothrombin G20210A, and MTHFR C677T mutations in 200 healthy
Jordanians. Clin Lab Sci. 2004; 17:200-202 PMid:15559724

- Eid SS, Shubeilat T. Prevalence of Factor
V Leiden, prothrombin G20210A, and MTHFR G677A among 594 thrombotic
Jordanian patients. Blood Coagul Fibrinolysis. 2005;16:417-421 http://dx.doi.org/10.1097/01.mbc.0000175478.46831.52

- Awidi A, Shannak M, Bseiso A, Kailani
MAM, Kailani MA, Omar N, Anshasi B, Sakarneh N. High Prevalence of
Factor V Leiden in Healthy Jordanian Arabs. Thromb Haemost.
1999;41:582-584

- Obeidat NM, Awidi A, Sulaiman NA,
Abu-Khader IB. Thrombophilia-related genetic variations in patients
with pulmonary embolism in the main teaching hospital in Jordan. Saudi
Med J. 2009;30:921-925 PMid:19618008

- Nusier MK, Radaideh AM, Ababneh NA,
Qaqish BM, Alzoubi R, Khader Y, Mersa JY, Irshaid NM, El-Khateeb M.
Prevalence of factor V G1691A (Leiden) and prothrombin G20210A
polymorphisms among apparently healthy Jordanians. Neuro Endocrinol
Lett. 2007;28:699-703 PMid:17984931

- Al-Sweedan SA, Jaradat S, Iraqi M,
Beshtawi M. The prevalence of factor V Leiden (G1691A), prothrombin
G20210A and methylenetetrahydrofolate reductase C677T mutations in
Jordanian patients with beta-thalassemia major. Blood Coagul
Fibrinolysis. 2009;20:675-678 http://dx.doi.org/10.1097/MBC.0b013e3283315b4f

- Dashti AA, Jadaon MM. Race differences in
the prevalence of the factor V Leiden mutation in Kuwaiti nationals.
Mol Biol Rep. 2010. http://dx.doi.org/10.1007/s11033-010-0474-7
PMid:21104134

- Jadaon MM, Dashti AA, Lewis HL. High
prevalence of activated protein C resistance and factor V Leiden
mutation in an Arab population and patients with venous thrombosis in
Kuwait. Diagn Mol Pathol. 2010;19:180-183 http://dx.doi.org/10.1097/00019606-201009000-00009
PMid:20736749

- Dzimiri N, Meyer B. World distribution of
factor V Leiden. Lancet. 1996;347:481-482 http://dx.doi.org/10.1016/S0140-6736(96)90064-1

- Almawi WY, Tamim H, Kreidy R, Timson G,
Rahal E, Nabulsi M, Finan RR, Irani-Hakime N. A case control study on
the contribution of factor V-Leiden, prothrombin G20210A, and MTHFR
C677T mutations to the genetic susceptibility of deep venous
thrombosis. J Thromb Thrombolysis. 2005;19:189-196 http://dx.doi.org/10.1007/s11239-005-1313-x
PMid:16082606

- Pathare A, Al Kindi S, Al Haddabi H,
Dennison D, Bayoumi R, Muralitharan S. Hereditary thrombophilia in
ethnic Omani patients. Am J Hematol. 2006;81:101-106 http://dx.doi.org/10.1002/ajh.20525
PMid:16432849

- Pawar AR, Shetty S, Ghosh K, Mohanty D.
How old is Factor V Leiden mutation? Thromb Haemost. 2001;86:1591-1592
PMid:11776338

- Zeinali S, Duca F, Zarbakhsh B, Tagliabue
L, Mannucci PM. Thrombophilic mutations in Iran. Thromb Haemost.
2000;83:351-352 PMid:10739401

- Mozafari H, Rahimi Z, Heidarpour A,
Fallahi M, Muniz A. The prevalence of factor V Leiden, prothrombin
G20210A and methylenetetrahydrofolate reductase polymorphism C677T
among G6PD deficient individuals from Western Iran. Mol Biol Rep.
2009;36:2361-3264 http://dx.doi.org/10.1007/s11033-009-9458-x
PMid:19219640

- Rahimi Z, Nomani H, Mozafari H,
Vaisi-Raygani A, Madani H, Malek-Khosravi S, Parsian A. Factor V
G1691A, prothrombin G20210A and methylenetetrahydrofolate reductase
polymorphism C677T are not associated with coronary artery disease and
type 2 diabetes mellitus in western Iran. Blood Coagul Fibrinolysis.
2009;20:252-256 http://dx.doi.org/10.1097/MBC.0b013e3283255487

- Rahimi Z, Ghaderi M, Nagel RL, Muniz A.
Prevalence of thrombotic risk factors among beta-thalassemia patients
from Western Iran. J Thromb Thrombolysis. 2008;26:229-233 http://dx.doi.org/10.1007/s11239-007-0163-0
PMid:17982733

- Rahimi Z, Mozafari H, Shahriari-Ahmadi A,
Alimogaddam K, Ghavamzadeh A, Aznab M, Mansouri K, Rezaei M, Parsian A.
Deep venous thrombosis and thrombophilic mutations in western Iran:
association with factor V Leiden. Blood Coagul Fibrinolysis.
2010;21:385-388 http://dx.doi.org/10.1097/MBC.0b013e328330e69a

- Lucotte G, Mercier G. Population genetics
of factor V Leiden in Europe. Blood Cells Mol Dis. 2001;27:362-367
http://dx.doi.org/10.1006/bcmd.2001.0388 PMid:11259157

- Cox MJ, Rees DC, Martinson JJ, Clegg JB.
Evidence of a single origin of factor V Leiden. Br J Haematol
92(4):1022-1025, 1996.
http://dx.doi.org/10.1046/j.1365-2141.1996.4961037.x PMid:8616062

- Rees DC, Cox M and Clegg JB. World
distribution of factor V Leiden. Lancet 346(8983): 1133-1134, 1995. http://dx.doi.org/10.1016/S0140-6736(95)91803-5

- Perry DJ and Pasi KJ. Resistance to activated protein C and factor V Leiden. Q J Med 90(6): 379-385, 1997
- Castoldi E, Lunghi B, Mingozzi F, Ioannou
P, Marchetti G, Bernardi F. New coagulation factor V gene polymorphisms
define a single and infrequent haplotype underlying the factor V Leiden
mutation in Mediterranean populations and Indians. Thromb Haemost.
1997;78:1037-1041 PMid:9308750

- Bauduer F, Lacombe D. Factor V Leiden,
prothrombin 20210A, methylenetetrahydrofolate reductase 677T, and
population genetics. Mol Genet Metab 2005;86:91-99 http://dx.doi.org/10.1016/j.ymgme.2005.04.002
PMid:16185908

- Jadaon MM, Dashti AA, Lewis HL. What is
the origin of factor V Leiden mutation in Arabs? The first molecular
proof. J Thromb Haemost. 2011;9: P-MO-155.
