Case Reports
A.P. Dayama, R. Kapoor, J.
Dass, G. Singh, M. Mahapatra and H.P. Pati
Published: November 10, 2011
Received: August 6, 2011
Accepted: September 6, 2011
Mediterr J Hematol Infect Dis 2011, 3(1): e20110, DOI 10.4084/MJHID.2011.051
This article is available from: http://www.mjhid.org/article/view/8987
Abstract
A middle aged man presented
with abdominal pain and fever, with
progressive dyspnea for the past one week. He had generalized
lymphadenopathy with hepatosplenomegaly and a left sided pleural
effusion on admission. Further evaluation revealed that he had
lymphocytosis on peripheral blood. He then developed increasing
abdominal pain and fall in hemoglobin which was confirmed on imaging to
be due to a splenic rupture and he underwent a splenectomy. The
diagnosis on lymph node biopsy and peripheral blood immunophenotyping
was grade 1 follicular lymphoma. He has completed his 6 cycles of
chemotherapy (R-CVP) and is on maintenance rituximab and doing well.
The case highlights the fact that splenic rupture can even be caused by
indolent lymphomas.
Introduction
Follicular lymphoma (FL) is the most common indolent non Hodgkin’s
lymphoma (NHL).[1]
It presents primarily with widespread disease which may be asymptomatic
and involves the bone marrow in around 40% of patients.[2]
Although the disease is widespread at presentation the incidence of
complications such as splenic rupture which are usually seen with other
aggressive lymphomas is rare.
Case Report
A 48 year old male presented to the emergency with complaints of
increasing abdominal distension and pain. He also had a history of
fever and breathlessness for the past 1 week. There was no history of
weight loss, skin rash, bleeding tendencies, bone/joint pains or
altered bowel/urinary habits. On examination he had generalized
lymphadenopathy (bilateral cervical, axillary, inguinal),
hepatosplenomegaly and decreased breath sounds over left hemithorax.
Rest of the examination was essentially normal. Investigations revealed
hemoglobin 11.7g/dL, total leucocyte count - 62,820/ ÁL, platelet
count- 169000/ÁL. The blood smear showed few smudge cells with mature
lymphocytosis (N6 L93, M1) with no malarial parasite and a reticulocyte
count of 2%. An ultrasound of the abdomen and chest showed
hepatosplenomegaly and small left sided pleural effusion. He developed
worsening of his symptoms with increased breathlessness and pain in
abdomen after admission. Chest X ray showed increasing pleural effusion
on the left side. However in view of progressive worsening of abdominal
pain in the next day, a repeat chest and abdominal CT was done, which
showed left pleural effusion with hepatosplenomegaly and multiple lymph
nodes in neck, mediastinum, bilateral axillae, retroperitoneal region.
There was a hypodense lesion in spleen suggestive of splenic rupture (Figure 1A).
He also developed fall in his hemoglobin from 10.4 to 6.3 g/dL in 3
days with severe abdominal pain for which he underwent emergency
splenectomy. The bone marrow aspirate showed near total replacement by
lymphocytes whereas the biopsy revealed diffuse infiltration by mature
lymphocytes. The immunophenotyping on peripheral blood was positive for
CD20, CD22, CD23, CD19, FMC7, CD79b and lambda restriction. It was
negative for CD5/23 co-exp, CD5, CD10, CD38, Zap 70, CD2, CD3, CD34,
CD25, CD11c, CD103. The LDH level was 385 U/dL and the serology for
HIV-1 & 2, HBsAg, Anti-HCV was negative. An axillary lymph node
biopsy was reported as grade 1 Follicular Lymphoma (Figure 1B and 1C).
Immunohistochemistry of lymphnode biopsy showed positive for CD 20,
CD10 and BCL-2, negative for Cyclin D1. The splenectomy specimen also
showed involvement by follicular lymphoma. The patient then received
chemotherapy (R-CVP) and was discharged in a stable condition with Hb
11.1 gm/dL, TLC 9490/ÁL, Plt 835000/ÁL. The patient has finished 6
cycles of R-CVP and is on 3 monthly maintenance Rituximab therapy and
is doing well.
Follicular lymphoma frequently involves spleen but incidence of
spontaneous splenic rupture is very rare. A variety of other causes
including acute leukemias, chronic leukemias, Hodgkin’s disease and NHL
have been reported to cause spontaneous splenic rupture.[3]
Pathologic rupture of spleen may be caused by the infiltration of the
splenic capsule by malignant cells leading to its congestion, splenic
infarction and possibly co-existent coagulation abnormalities leading
to subcapsular hematomas and capsular rupture.[4]
After searching the MEDLINE database, we came across only 1 series by
Howard et al who have described a total of 16 cases of FL involving the
spleen among which 3 underwent splenectomy for splenic rupture. In
their series, 12/16 patients were diagnosed as FL on the splenectomy
specimen including the 3 cases presenting with splenic rupture while in
the rest 4 cases, the diagnosis was established before splenectomy.[5] Splenic rupture has been seen in cases of mantle cell
lymphoma[6] and only rarely in other low grade
lymphomas such as Waldenstrom macroglobulinemia.[7]
This highlights the fact that even though rare the possibility of
indolent lymphomas such as FL should be kept in mind in a patient who
has rupture of the spleen.
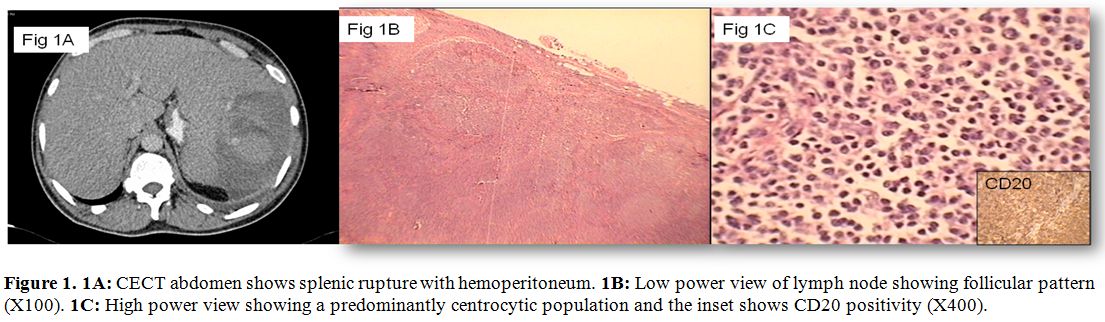
Figure 1. 1A: CECT abdomen shows splenic rupture with hemoperitoneum. 1B: Low power view of lymph node showing follicular pattern (X100). 1C: High power view showing a predominantly centrocytic population and the inset shows CD20 positivity (X400).
References
- Jaffe ES, Harris NL, Stein H, Vardiman JW. Pathology and genetics of tumours of haematopoietic and lymphoid tissues. In: Kleihues P, Sobin LH, editors. (World Health Organization Classification of Tumours). International Agency for Research on Cancer Press; 2001.
- Armitage JO, Weisenburger DD. New approach
to classifying non-Hodgkin’s lymphomas: clinical features of the major
histologic subtypes. Non-Hodgkin’s Lymphoma Classification Project. J
Clin Oncol 1998;16:2780–95. PMid:9704731

- Giagounidis AA, Burk M, Meckenstock G, Koch
AJ, Schneider W. Pathologic rupture of the spleen in hematologic
malignancies: two additional cases. Ann Hematol 1996;73:297-302. http://dx.doi.org/10.1007/s002770050245
PMid:9003161

- Ioannidis O, Papaemmanouil S, Paraskevas G,
Chatzopoulos S, Kotronis A, Papadimitriou N et al. Pathologic rupture
of the spleen as the presenting symptom of primary splenic Non-Hodgkin
Lymphoma. J Gastrointest Cancer. http://dx.doi.org/10.1007/s12029-011-9280-2.

- Howard MT, Dufresne S, Swerdlow SH, Cook
JR. Follicular lymphoma of the spleen: multiparameter analysis of 16
cases. Am J Clin Pathol 2009;131:656-62. http://dx.doi.org/10.1309/AJCPF9V8XRDYWTIR
PMid:19369624

- Strickland AH, Marsden KA, McArdle J,
Lowenthal RM. Pathologic Splenic Rupture as the Presentation of Mantle
Cell Lymphoma. Leuk Lymphoma. 2001;41:197-201. http://dx.doi.org/10.3109/10428190109057971

- Charakidis M, Russell DJ. Spontaneous
splenic rupture in Waldenstrom’s macroglobulinemia: a case report.
Journal of Medical Case Reports 2010, 4:300. http://dx.doi.org/10.1186/1752-1947-4-300
PMid:20825629 PMCid:2944189
