Review Articles
Epidemiology of
Prothrombin G20210A Mutation in the Mediterranean RegionM.M. Jadaon
1Department of
Medical Laboratory Sciences, Faculty of Allied Health Sciences, Kuwait
University, Kuwait
Correspondence
to:
Mehrez M. Jadaon. Department of Medical Laboratory Sciences, Faculty of
Allied Health Sciences, Kuwait University, P.O. Box 31470 – Sulaibekaht
90805 – Kuwait. Tel.: (965) 6664 3485 Fax: (965) 2498 3835. Email: mehrez@hsc.edu.kw mehrezmls99@yahoo.com
Published: November 28, 2011
Received: October 1, 2011
Accepted: October 7, 2011
Mediterr J Hematol Infect Dis 2011, 3(1): e2011054, DOI 10.4084/MJHID.2011.054
This article is available from: http://www.mjhid.org/article/view/9310
This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License
(http://creativecommons.org/licenses/by/2.0),
which permits
unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited
Abstract
There are many genetic and acquired risk factors that are known to cause venous thromboembolic disorders (VTE). One of these is the Prothrombin G20210A mutation, which has been identified in 1996. Prothrombin G20210A mutation causes higher levels of the clotting factor prothrombin in the blood of carriers, which creates a higher tendency towards blood clotting (hypercoagulability), and therefore the carriers become at higher risk of developing VTE. High prevalence of Prothrombin G20210A mutation was reported in Caucasian populations, but the prevalence was almost absent in non-Caucasians. That was most obvious in countries of South Europe and the Mediterranean region. This review article discusses Prothrombin G20210A mutation, how it causes VTE, the origin of the mutation, and its distribution worldwide with special concentration on the Mediterranean area.
Introduction
Venous thromboembolic disorders (VTE) are serious disorders accounting for high morbidity and mortality rates with an annual incidence of 1/1000.[1-4] Many genetic and acquired risk factors were identified to cause VTE including Factor V Leiden mutation, genetic deficiencies of proteins C, S and antithrombin, lupus anticoagulants, pregnancy, use of contraceptives, major surgeries, cancer, inflammations, and Prothrombin G20210A mutation. This review article focuses on Prothrombin G20210A mutation, its pathophysiology, prevalence and origin, with a special concentration on this mutation in the Mediterranean region.
Role of Prothrombin in the Coagulation System
In case of blood vessel injury, blood coagulation is initiated through a cascade of chemical reactions to form a blood clot to block the injured blood vessel and prevent blood loss. Several enzymes and proteins, generally known as blood clotting factors, are involved in blood coagulation, a very important one is thrombin (clotting factor II). Thrombin is usually produced in the liver in an inactive form called prothrombin, which circulates in the blood until being activated in case of injury. Potrhombin gets activated into thrombin by another clotting factor called activated factor X. The main function of thrombin is to convert fibrinogen (clotting factor I) into a fibrin clot that blocks the injured blood vessel. In fact, thrombin is a very robust enzyme that plays a major role in the coagulation system by activating many clotting factors and other elements of the coagulation system like the blood platelets. Thrombin is usually under careful monitoring by an inhibitor called antithrombin (AT), which down-regulates thrombin after clot formation and prevents accidental formation of thrombin in sites away from injured vessels.[5,6] This is very crucial to prevent the formation of unnecessary clots inside intact blood vessels. The formation of such intravascular clots predisposes to the development of VTE.
Prothrombin G20210A Mutation
Because of the importance of thrombin in the coagulation system, genetic or acquired deficiency of prothrombin usually causes impaired clotting and therefore bleeding problems (hemophilia). On the contrary, if prothrombin is produced in higher quantities in the blood, this is expected to cause an increased tendency towards blood clotting, a condition known as “hypercoagulability”, which usually manifests clinically as VTE. It has been demonstrated that prothrombin levels more than 115% of the normal level have 2-fold increased risk of developing VTE.[7] Poort et al (1996) performed an extensive DNA sequencing on the prothrombin gene (on chromosome 11) for patients with unexplained VTE.[7] They found a single missense mutation (guanine to adenine; GA) at nucleotide position 20210, which is present in the 3′ untranslated region of the prothrombin gene. This Prothrombin G20210A mutation is present outside the coding region for prothrombin, and hence it does not affect the actual structure of the prothrombin molecule and it does not affect its function as a strong clotting factor when activated into thrombin. However, Prothrombin G20210A mutation was found to cause elevated levels of blood prothrombin (by one-third above normal; 133%), which is more than the extra 15% needed to develop VTE. Also, it has been proven that Prothrombin G20210A mutation leads to increased mRNA and protein expression for prothrombin.[8]
Moreover, increased prothrombin levels may lead to an increase in a protein called thrombin-activatable fibrinolysis inhibitor (TAFI), which is an inhibitor of the fibrinolysis process. Fibrinolysis is the process by which the blood removes clots. Therefore, an increase in TAFI may disturb the fibrinolysis process and therefore allow for accumulation of clots leading to VTE.[9,10] This is another possible pathophysiological pathway of causing VTE in cases having Prothrombin G20210A mutation with elevated TAFI. All these findings may explain why Prothrombin G20210A mutation may cause hypercoagulability and an increased risk of developing VTE. Such increased risk was reported to be 2 to 4-fold.[7,11-15]
Prevalence of Prothrombin G20210A mutation
The prevalence of Prothrombin G20210A mutation in European Caucasians was found to be roughly 3-17% in patients with VTE and 1-8% in healthy controls. That was also true in Caucasians living outside Europe like in the USA, Australia, Brazil and Israel (Table 1). It may be noticed here that the prevalence of Prothrombin G20210A mutation is higher in the Southern European countries than in the Northern countries, in spite of presence of overlapping between the North and South. On the other hand, Prothrombin G20210A mutation was found to be very rare or even absent in Asian and African populations, and in native populations of America (Amerindians) and Australia (Table 1). This was also true when these populations were studied in countries outside their origin like African Americans and Asians living in the USA. The only exception to the above observations is the high prevalence reported in Hispanics and Mexican Mestizos; the latter are descendants of mixed marriages between Europeans and Amerindians. The presence of European genes in such populations may explain the high prevalence of Prothrombin G20210A mutation in these.
High prevalence of Prothrombin G20210A mutation was also reported in populations living close to Europe, namely countries of the Middle East and North Africa. In fact, the prevalence in these countries was very comparable with the prevalence reported in Southern European countries. Therefore, the countries present on the coasts of the Mediterranean Sea, including Southern Europe, may be grouped together sharing the same prevalence of Prothrombin G20210A mutation (Table 2). These countries, 20 in total, have a prevalence of 3-24% in patients with VTE and 1-12% in the general population. No reports could be found in Malta, Syria, Bosnia, Albania and Macedonia. The highest prevalence was found by a study in Egypt in patients with VTE, but the highest among the general populations (healthy controls) was in Palestinians living in Israel (Israeli Arabs). Unfortunately, there were no reports on the prevalence in Palestinian patients with VTE, which kight be higher than the one reported in Egypt, noting that Egypt and Palestine are geographically neighbours.
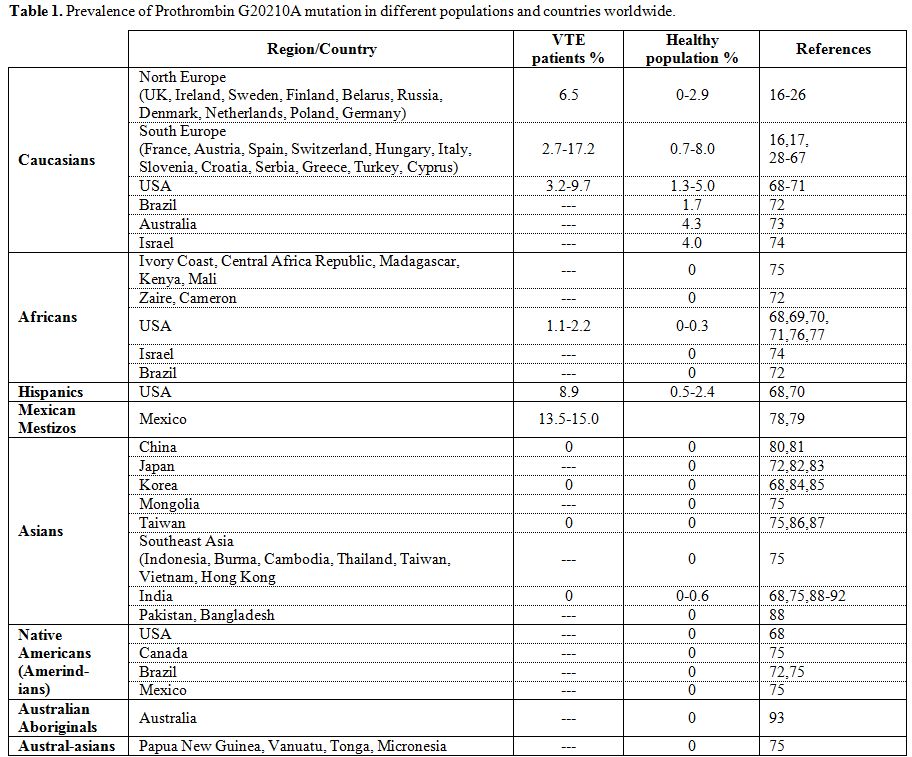
Table 1. Prevalence of Prothrombin G20210A mutation in different populations and countries worldwide.
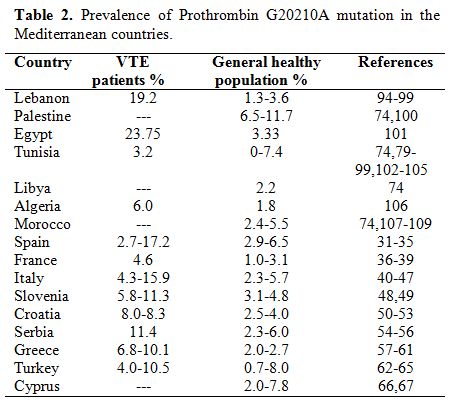
Table 2. Prevalence of Prothrombin G20210A mutation in the Mediterranean countries.
Origin of Prothrombin G20210A mutation
The highest prevalence of Prothrombin G20210A mutation in European Caucasians brought up speculations that Prothrombin G20210A mutation might have occurred as a single event in a single Caucasian ancestor and that the current Caucasian carriers of the mutation should have descended from that proposed grandparent. This assumption was supported by a molecular study that found a haplotype to be associated with more than two third of carriers of the mutation compared to one third of non-carriers. This suggests a founder effect, and the mutation was estimated to occur around 24 thousand years ago after the divergence of Africans from Non-Africans and Caucasoids from Mongoloids.[110] It is tempting to explore this founder haplotype in non-Caucasian carriers of the Prothrombin G20210A mutation in the Middle East and North Africa to see if this founder effect occurred there too. In addition, it may be interesting to study this mutation in the Basque population (in France and Spain), who is thought to be the oldest ethnic group living in Europe. Finding or not finding the mutation in this population may give a hint on the origin of the mutation and to know if it occurred inside or outside Europe. Also, if a future study can prove that Palestinian patients with VTE have the highest prevalence of Prothrombin G20210A mutation (like the general Palestinian population), then this region (Palestine/Israel) may be the place where the mutation has occurred and then spread to Europe and other parts of the Mediterranean region. This region has witnessed a lot of mankind movements since the old ages, since the Neolithic period, and then the Phoenicians who appeared in Lebanon and then cruised to many cities on the Mediterranean coast, followed by the Roman and Greek civilizations, and more recently the Crusaders and Ottomans. Therefore, it is encouraging to try to find certain genetic or chromosomal markers that can help in following the migratory history of manhood in the Mediterranean region which may give a final approach towards determining exactly where the mutation has occurred first and how it spread all over the Mediterranean region.
Conclusions
The prevalence of Prothrombin G20210A mutation differs in different countries and ethnic groups, being highest in Caucasians, especially those in the Southern Europe, and in the Mediterranean region. Further studies are needed to verify where exactly has the mutation occurred first and how it was carried to other parts of the world.
Venous thromboembolic disorders (VTE) are serious disorders accounting for high morbidity and mortality rates with an annual incidence of 1/1000.[1-4] Many genetic and acquired risk factors were identified to cause VTE including Factor V Leiden mutation, genetic deficiencies of proteins C, S and antithrombin, lupus anticoagulants, pregnancy, use of contraceptives, major surgeries, cancer, inflammations, and Prothrombin G20210A mutation. This review article focuses on Prothrombin G20210A mutation, its pathophysiology, prevalence and origin, with a special concentration on this mutation in the Mediterranean region.
Role of Prothrombin in the Coagulation System
In case of blood vessel injury, blood coagulation is initiated through a cascade of chemical reactions to form a blood clot to block the injured blood vessel and prevent blood loss. Several enzymes and proteins, generally known as blood clotting factors, are involved in blood coagulation, a very important one is thrombin (clotting factor II). Thrombin is usually produced in the liver in an inactive form called prothrombin, which circulates in the blood until being activated in case of injury. Potrhombin gets activated into thrombin by another clotting factor called activated factor X. The main function of thrombin is to convert fibrinogen (clotting factor I) into a fibrin clot that blocks the injured blood vessel. In fact, thrombin is a very robust enzyme that plays a major role in the coagulation system by activating many clotting factors and other elements of the coagulation system like the blood platelets. Thrombin is usually under careful monitoring by an inhibitor called antithrombin (AT), which down-regulates thrombin after clot formation and prevents accidental formation of thrombin in sites away from injured vessels.[5,6] This is very crucial to prevent the formation of unnecessary clots inside intact blood vessels. The formation of such intravascular clots predisposes to the development of VTE.
Prothrombin G20210A Mutation
Because of the importance of thrombin in the coagulation system, genetic or acquired deficiency of prothrombin usually causes impaired clotting and therefore bleeding problems (hemophilia). On the contrary, if prothrombin is produced in higher quantities in the blood, this is expected to cause an increased tendency towards blood clotting, a condition known as “hypercoagulability”, which usually manifests clinically as VTE. It has been demonstrated that prothrombin levels more than 115% of the normal level have 2-fold increased risk of developing VTE.[7] Poort et al (1996) performed an extensive DNA sequencing on the prothrombin gene (on chromosome 11) for patients with unexplained VTE.[7] They found a single missense mutation (guanine to adenine; GA) at nucleotide position 20210, which is present in the 3′ untranslated region of the prothrombin gene. This Prothrombin G20210A mutation is present outside the coding region for prothrombin, and hence it does not affect the actual structure of the prothrombin molecule and it does not affect its function as a strong clotting factor when activated into thrombin. However, Prothrombin G20210A mutation was found to cause elevated levels of blood prothrombin (by one-third above normal; 133%), which is more than the extra 15% needed to develop VTE. Also, it has been proven that Prothrombin G20210A mutation leads to increased mRNA and protein expression for prothrombin.[8]
Moreover, increased prothrombin levels may lead to an increase in a protein called thrombin-activatable fibrinolysis inhibitor (TAFI), which is an inhibitor of the fibrinolysis process. Fibrinolysis is the process by which the blood removes clots. Therefore, an increase in TAFI may disturb the fibrinolysis process and therefore allow for accumulation of clots leading to VTE.[9,10] This is another possible pathophysiological pathway of causing VTE in cases having Prothrombin G20210A mutation with elevated TAFI. All these findings may explain why Prothrombin G20210A mutation may cause hypercoagulability and an increased risk of developing VTE. Such increased risk was reported to be 2 to 4-fold.[7,11-15]
Prevalence of Prothrombin G20210A mutation
The prevalence of Prothrombin G20210A mutation in European Caucasians was found to be roughly 3-17% in patients with VTE and 1-8% in healthy controls. That was also true in Caucasians living outside Europe like in the USA, Australia, Brazil and Israel (Table 1). It may be noticed here that the prevalence of Prothrombin G20210A mutation is higher in the Southern European countries than in the Northern countries, in spite of presence of overlapping between the North and South. On the other hand, Prothrombin G20210A mutation was found to be very rare or even absent in Asian and African populations, and in native populations of America (Amerindians) and Australia (Table 1). This was also true when these populations were studied in countries outside their origin like African Americans and Asians living in the USA. The only exception to the above observations is the high prevalence reported in Hispanics and Mexican Mestizos; the latter are descendants of mixed marriages between Europeans and Amerindians. The presence of European genes in such populations may explain the high prevalence of Prothrombin G20210A mutation in these.
High prevalence of Prothrombin G20210A mutation was also reported in populations living close to Europe, namely countries of the Middle East and North Africa. In fact, the prevalence in these countries was very comparable with the prevalence reported in Southern European countries. Therefore, the countries present on the coasts of the Mediterranean Sea, including Southern Europe, may be grouped together sharing the same prevalence of Prothrombin G20210A mutation (Table 2). These countries, 20 in total, have a prevalence of 3-24% in patients with VTE and 1-12% in the general population. No reports could be found in Malta, Syria, Bosnia, Albania and Macedonia. The highest prevalence was found by a study in Egypt in patients with VTE, but the highest among the general populations (healthy controls) was in Palestinians living in Israel (Israeli Arabs). Unfortunately, there were no reports on the prevalence in Palestinian patients with VTE, which kight be higher than the one reported in Egypt, noting that Egypt and Palestine are geographically neighbours.
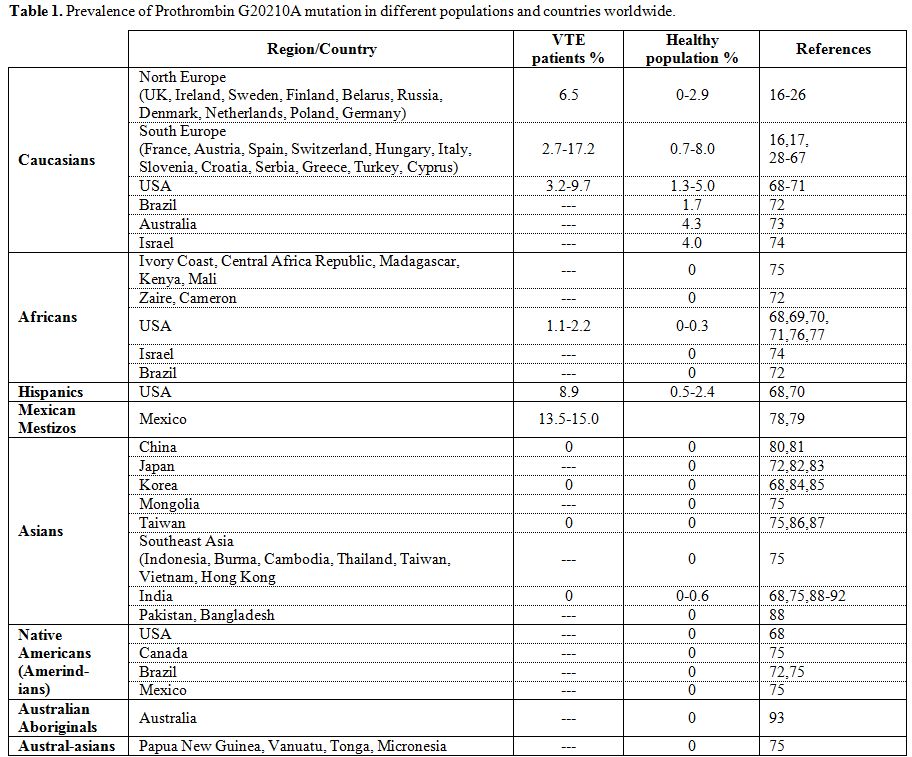
Table 1. Prevalence of Prothrombin G20210A mutation in different populations and countries worldwide.
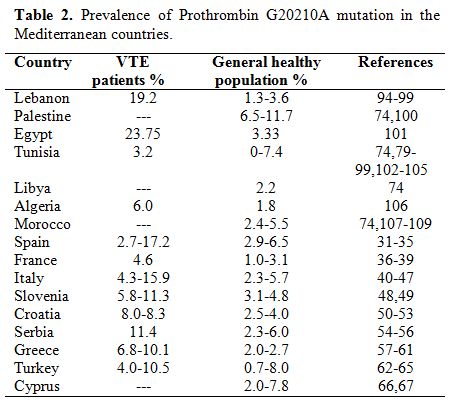
Table 2. Prevalence of Prothrombin G20210A mutation in the Mediterranean countries.
Origin of Prothrombin G20210A mutation
The highest prevalence of Prothrombin G20210A mutation in European Caucasians brought up speculations that Prothrombin G20210A mutation might have occurred as a single event in a single Caucasian ancestor and that the current Caucasian carriers of the mutation should have descended from that proposed grandparent. This assumption was supported by a molecular study that found a haplotype to be associated with more than two third of carriers of the mutation compared to one third of non-carriers. This suggests a founder effect, and the mutation was estimated to occur around 24 thousand years ago after the divergence of Africans from Non-Africans and Caucasoids from Mongoloids.[110] It is tempting to explore this founder haplotype in non-Caucasian carriers of the Prothrombin G20210A mutation in the Middle East and North Africa to see if this founder effect occurred there too. In addition, it may be interesting to study this mutation in the Basque population (in France and Spain), who is thought to be the oldest ethnic group living in Europe. Finding or not finding the mutation in this population may give a hint on the origin of the mutation and to know if it occurred inside or outside Europe. Also, if a future study can prove that Palestinian patients with VTE have the highest prevalence of Prothrombin G20210A mutation (like the general Palestinian population), then this region (Palestine/Israel) may be the place where the mutation has occurred and then spread to Europe and other parts of the Mediterranean region. This region has witnessed a lot of mankind movements since the old ages, since the Neolithic period, and then the Phoenicians who appeared in Lebanon and then cruised to many cities on the Mediterranean coast, followed by the Roman and Greek civilizations, and more recently the Crusaders and Ottomans. Therefore, it is encouraging to try to find certain genetic or chromosomal markers that can help in following the migratory history of manhood in the Mediterranean region which may give a final approach towards determining exactly where the mutation has occurred first and how it spread all over the Mediterranean region.
Conclusions
The prevalence of Prothrombin G20210A mutation differs in different countries and ethnic groups, being highest in Caucasians, especially those in the Southern Europe, and in the Mediterranean region. Further studies are needed to verify where exactly has the mutation occurred first and how it was carried to other parts of the world.
References
- Dahlbäck B. Resistance to activated protein
C, the Arg506 to Gln mutation in the factor V gene, and venous
thrombosis. Functional tests and DNA-based assays. Pros and Cons.
Thromb Haemost. 1995;73:739-742 PMid:7482395

- Rees DC, Cox M, Clegg JB. World
distribution of factor V Leiden. Lancet. 1995;346:1133-1134 http://dx.doi.org/10.1016/S0140-6736(95)91803-5

- Ridker PM, Miletich JP, Hennekens CH,
Buring JE. Ethnic distribution of Factor V Leiden in 4047 men and
women. Implications for venous thrmoboembolism screening. JAMA.
1997;277:1305-1307 http://dx.doi.org/10.1001/jama.277.16.1305

- Zivelin A, Griffin JH, Xu X, Pabinger I,
Samama M, Conard J, Brenner B, Eldor A, Seligsohn U. A single genetic
origin for a common Caucasian risk factor for venous thrombosis. Blood.
1997;89:397-402 PMid:9002940

- Lane DA, Mannucci PM, Bauer KA, Bertina RM,
Bochkov NP, Boulyjenkov V, Chandy M, Dahlbäck B, Ginter EK, Miletich
JP, Rosendaal FR, Seligsohn U. Inherited thrombophilia: Part 1. Thromb
Haemost. 1996;76:651-662 PMid:8950768

- Davie EW. Biochemical and molecular aspects
of the coagulation cascade. Thromb Haemost. 1995;74:1-6PMid:8578439

- Poort SR, Rosendaal FR, Reitsma PH, Bertina
RM. A common genetic variation in the 3'-untranslated region of the
prothrombin gene is associated with elevated plasma prothrombin levels
and an increase in venous thrombosis. Blood. 1996;88:3698-3703
PMid:8916933

- Ceelie H, Spaargaren-van Riel CC, Bertina
RM, Vos HL. G20210A is a functional mutation in the prothrombin gene;
effect on protein levels and 3'-end formation. J Thromb Haemost.
2004;2:119-127 http://dx.doi.org/10.1111/j.1538-
836.2003.00493.x
PMid:14717975

- Meltzer ME, Lisman T, de Groot PG, Meijers
JC, le Cessie S, Doggen CJ, Rosendaal FR. Venous thrombosis risk
associated with plasma hypofibrinolysis is explained by elevated plasma
levels of TAFI and PAI-1. Blood. 2010;116:113-121 http://dx.doi.org/10.1182/blood-2010-02-267740
PMid:20385790

- Miljić P, Heylen E, Willemse J, Djordjević
V, Radojković D, Colović M, Elezović I, Hendriks D. Thrombin
activatable fibrinolysis inhibitor (TAFI): a molecular link between
coagulation and fibrinolysis. Srp Arh Celok Lek. 2010;138:74-78
PMid:20229688

- Bertina, RM. Factor V Leiden and other
coagulation factor mutations affecting thrombotic risk. Cl Chem.
1997:43:1678–1683 PMid:9299960

- Koeleman BPC, Reitsma PH, Bertina RM.
Familial thrombophilia: a complex genetic disorder. Semin Hematol.
1997;34:256-264 PMid:9241710

- Hillarp A, Zöller B, Svensson PJ, Dahlbäck
B. The 20210A allele of the prothrombine gene is a common risk factor
among Swedish outpatients with verified deep venous thrombosis. Thromb
Haemost. 1997;78:990-992 PMid:9308741

- Alhenc-Gelas M, Le Cam-Duchez V, Emmerich J, Frebourg T, Fiessinger JN, Barg JY, Aiach M. The A20210 allele of the prothrombin gene is not frequently associated with the factor V Arg506 to Gln mutation in thrombophilic families. Blood. 1997;96:1711
- Dahlbäck B. Advances in understanding
pathogenic mechanisms of thrombophilic disorders. Blood. 2008;112:19-27
http://dx.doi.org/10.1182/blood-2008-01-077909
PMid:18574041

- Rosendaal FR, Doggen CJ, Zivelin A, Arruda
VR, Aiach M, Siscovick DS, Hillarp A, Watzke HH, Bernardi F, Cumming
AM, Preston FE, Reitsma PH. Geographic distribution of the 20210 G to A
prothrombin variant. Thromb Haemost. 1998;79:706-708 PMid:9569177

- Bykowska K, Vertun-Baranowska B, Windyga
J, Łopaciuk S. Prevalence of G20210A prothrombin gene mutation in
Poland. Pol Arch Med Wewn. 2000;104:729-733 PMid:11434083

- McColl
MD, Ellison J, Reid F, Tait RC,
Walker ID, Greer IA. Prothrombin 20210 ⋄A, MTHFR C677T mutations in
women with venous thromboembolism associated with pregnancy. BJOG.
2000;107:565-569 http://dx.doi.org/10.1111/j.1471-0528.2000.tb13281.x

- Wramsby ML, Sten-Linder M, Bremme K.
Primary habitual abortions are associated with high frequency of factor
V Leiden mutation. Fertil Steril. 2000;74:987-991 http://dx.doi.org/10.1016/S0015-0282(00)01545-4

- Vossen CY, Hoffmeister M, Chang-Claude JC,
Rosendaal FR, Brenner H. Clotting factor gene polymorphisms and
colorectal cancer risk. J Clin Oncol. 2011;29:1722-1727 http://dx.doi.org/10.1200/JCO.2010.31.8873
PMid:21422408

- Petäjä J, Hiltunen L, Fellman V. Increased
risk of intraventricular hemorrhage in preterm infants with
thrombophilia. Pediatr Res. 2001;49:643-646 http://dx.doi.org/10.1203/00006450-200105000-00006

- Avdonin PV, Kirienko AI, Kozhevnikova LM,
Shostak NA, Babadaeva NM, Leont'ev SG, Petukhov EB, Kubatiev AA,
Savel'ev VS. C677T mutation in methylentetrahydrofolatereductase gene
in patients with venous thromboses from the central region of Russia
correlates with a high risk of pulmonary artery thromboembolism. Ter
Arkh. 2006;78:70-76

- Lipay NV, Dmitriev VV, Borisenok MB.
Thrombotic complications during cancer treatment in children. Exp
Oncol. 2007;29:231-235 PMid:18004248

- Keenan C, Livingstone WJ, White B,
Mynett-Johnson L, Cusack S, Lawler M, Smith OP. Prevalence of the
prothrombin G20210A mutation in the Irish populations: use of a novel
polymerase chain reaction approach. Blood Coagul Fibrinolysis.
2000;11:669-672 PMid:7482395

- Pherwani AD, Winter PC, McNamee PT,
Patterson CC, Hill CM, Connolly JK, Maxwell AP. Is screening for factor
V Leiden and prothrombin G20210A mutations in renal transplantation
worthwhile? Results of a large single-center U.K. study.
Transplantation. 2003;76:603-605

- Jensen MK, de Nully Brown P, Thorsen S,
Hasselbalch HC. Frequent occurrence of anticardiolipin antibodies,
Factor V Leiden mutation, and perturbed endothelial function in chronic
myeloproliferative disorders. Am J Hematol. 2002;69:185-191

- Silingardi M, Salvarani C, Boiardi L,
Accardo P, Iorio A, Olivieri I, Cantini F, Salvi F, La Corte R, Triolo
G, Ciccia F, Ghirarduzzi A, Filippini D, Paolazzi G, Iori I. Factor V
Leiden and prothrombin gene G20210A mutations in Italian patients with
Behçet's disease and deep vein thrombosis. Arthritis Rheum.
2004;51:177-183 PMid:9002940

- Balogh I, Póka R, Losonczy G, Muszbek L.
High frequency of factor V Leiden mutation and prothrombin 20210A
variant in Romanies of Eastern Hungary. Thromb Haemost.
1999;82:1555-1556 PMid:8950768

- Laczkovics C, Grafenhofer H, Kaider A,
Quehenberger P, Simanek R, Mannhalter C, Lechner K, Pabinger I. Risk of
recurrence after a first venous thromboembolic event in young women.
Haematologica. 2007;92:1201-1207 PMid:8578439

- Lalouschek W, Schillinger M, Hsieh K,
Endler G, Tentschert S, Lang W, Cheng S, Mannhalter C. Matched
case-control study on factor V Leiden and the prothrombin G20210A
mutation in patients with ischemic stroke/transient ischemic attack up
to the age of 60 years. Stroke. 2005;36:1405-1409 PMid:8916933

- Francès F, Portolès O, Gabriel F, Corella
D, Sorlí JV, Sabater A, Alfonso JL, Guillén M. Factor V Leiden (G1691A)
and prothrombin-G20210A alleles among patients with deep venous
thrombosis and in the general population from Spain. Rev Med Chil.
2006;134:13-20 PMid:14717975

- González Ordóñez AJ, Medina Rodríguez JM,
Fernández Alvarez CR, Sánchez García J, Martín Sánchez L, Coto García
E, Alvarez Martínez MV. 20210A mutation of the prothrombin and venous
thromboembolism gene. Sangre (Barc). 1999;44:13-18 PMid:20385790

- Alvarez A, Barroso A, Robledo M, Arranz E,
Outeiriño J, Benítez J. Prevalence of Factor V Leiden and the G20210A
mutation of the prothrombin gene in a random group of patients with
thrombotic episodes. Sangre (Barc). 1999;44:7-12 PMid:20229688

- Souto JC, Coll I, Llobet D, del Río E,
Oliver A, Mateo J, Borrell M, Fontcuberta J. The prothrombin 20210A
allele is the most prevalent genetic risk factor for venous
thromboembolism in the Spanish population. Thromb Haemost.
1998;80:366-369 PMid:9299960

- Roldan V, Lecumberri R, Muñoz-Torrero JF,
Vicente V, Rocha E, Brenner B, Monreal M; RIETE Investigators.
Thrombophilia testing in patients with venous thromboembolism. Findings
from the RIETE registry. Thromb Res. 2009;124:174-177 PMid:9241710

- Leroyer C, Mercier B, Oger E, Chenu E,
Abgrall JF, Férec C, Mottier D. Prevalence of 20210 A allele of the
prothrombin gene in venous thromboembolism patients. Thromb Haemost.
1998;80:49-51 PMid:9308741

- Mazoyer E, Ripoll L, Gueguen R, Tiret L,
Collet JP, dit Sollier CB, Roussi J, Drouet L; FITENAT Study Group.
Prevalence of factor V Leiden and prothrombin G20210A mutation in a
large French population selected for nonthrombotic history:
geographical and age distribution. Blood Coagul Fibrinolysis.
2009;20:503-510

- Pasquier E, Bohec C, Mottier D, Jaffuel S,
Mercier B, Férec C, Collet M, De Saint Martin L. Inherited
thrombophilias and unexplained pregnancy loss: an incident case-control
study. J Thromb Haemost. 2009;7:306-311 PMid:18574041

- Reny JL, Alhenc-Gelas M, Fontana P,
Bissery A, Julia PL, Fiessinger JN, Aiach M, Emmerich J. The factor II
G20210A gene polymorphism, but not factor V Arg506Gln, is associated
with peripheral arterial disease: results of a case-control study. J
Thromb Haemost. 2004;2:1334-1340 PMid:9569177

- Martinelli I, Bucciarelli P, Margaglione
M, De Stefano V, Castaman G, Mannucci PM. The risk of venous
thromboembolism in family members with mutations in the genes of factor
V or prothrombin or both. Br J Haematol. 2000;111:1223-1239
PMid:11434083

- Martinelli I, Taioli E, Cetin I, Marinoni
A, Gerosa S, Villa MV, Bozzo M, Mannucci PM. Mutations in coagulation
factors in women with unexplained late fetal loss. N Engl J Med.
2000;343:1015-1018

- Margaglione M, Brancaccio V, De Lucia D,
Martinelli I, Ciampa A, Grandone E, Di Minno G. Inherited thrombophilic
risk factors and venous thromboembolism: distinct role in peripheral
deep venous thrombosis and pulmonary embolism. Chest.
2000;118:1405-411.

- de Moerloose P, Reber G, Perrier A,
Perneger T, Bounameaux H. Prevalence of factor V Leiden and prothrombin
G20210A mutations in unselected patients with venous thromboembolism.
Br J Haematol. 2000;110:125-129PMid:21422408

- Silingardi M, Salvarani C, Boiardi L,
Accardo P, Iorio A, Olivieri I, Cantini F, Salvi F, La Corte R, Triolo
G, Ciccia F, Ghirarduzzi A, Filippini D, Paolazzi G, Iori I. Factor V
Leiden and prothrombin gene G20210A mutations in Italian patients with
Behçet's disease and deep vein thrombosis. Arthritis Rheum.
2004;51:177-183

- Sottilotta G, Mammì C, Furlò G, Oriana V,
Latella C, Trapani Lombardo V. High incidence of factor V Leiden and
prothrombin G20210A in healthy southern Italians. Clin Appl Thromb
Hemost. 2009;15:356-359

- Tosetto A, Missiaglia E, Frezzato M,
Rodeghiero F. The VITA project: prothrombin G20210A mutation and venous
thromboembolism in the general population. Thromb Haemost.
1999;82:1395-1398 PMid:18004248

- Cattaneo M, Chantarangkul V, Taioli E,
Santos JH, Tagliabue L. The G20210A mutation of the prothrombin gene in
patients with previous first episodes of deep-vein thrombosis:
prevalence and association with factor V G1691A,
methylenetetrahydrofolate reductase C677T and plasma prothrombin
levels. Thromb Res. 1999;93:1-8

- Bedencic M, Bozic M, Peternel P, Stegnar
M. Major and potential prothrombotic genotypes in patients with venous
thrombosis and in healthy subjects from Slovenia. Pathophysiol Haemost
Thromb. 2008;36:58-63

- Zerjavic K, Zagradisnik B, Stangler
Herodez S, Lokar L, Glaser Krasevac M, Kokalj Vokac N. Is the JAK2
V617F mutation a hallmark for different forms of thrombosis? Acta
Haematol. 2010;124:49-56

- Jukic I, Bingulac-Popovic J, Dogic V,
Babic I, Culej J, Tomicic M, Vuk T, Sarlija D, Balija M. ABO blood
groups and genetic risk factors for thrombosis in Croatian population.
Croat Med J. 2009;50:550-558

- Herak DC, Antolic MR, Krleza JL, Pavic M,
Dodig S, Duranovic V, Brkic AB, Zadro R. Inherited prothrombotic risk
factors in children with stroke, transient ischemic attack, or
migraine. Pediatrics. 2009;123:e653-660

- Eterović D, Titlić M, Culić V, Zadro R,
Primorac D. Lower contribution of factor V Leiden or G202104 mutations
to ischemic stroke in patients with clinical risk factors: pair-matched
case-control study. Clin Appl Thromb Hemost. 2007;13:188-193

- Coen D, Zadro R, Honović L, Banfić L,
Stavljenić Rukavina A. Prevalence and association of the factor V
Leiden and prothrombin G20210A in healthy subjects and patients with
venous thromboembolism. Croat Med J. 2001;42:488-492

- Kovac M, Mitic G, Mikovic Z, Djordjevic V,
Savic O, Mandic V, Rakicevic LJ, Antonijevic N, Radojkovic D.
Thrombophilia in women with pregnancy-associated complications: fetal
loss and pregnancy-related venous thromboembolism. Gynecol Obstet
Invest. 2010;69:233-238

- Djordjevic V, Stankovic M,
Brankovic-Sreckovic V, Rakicevic L, Radojkovic D. Genetic risk factors
for arterial ischemic stroke in children: a possible MTHFR and eNOS
gene-gene interplay? J Child Neurol. 2009;24:823-827

- Djordjevic V, Rakicevic LJ, Mikovic D,
Kovac M, Miljic P, Radojkovic D, Savic A. Prevalence of factor V
leiden, factor V cambridge, factor II G20210A and
methylenetetrahydrofolate reductase C677T mutations in healthy and
thrombophilic Serbian populations. Acta Haematol. 2004;112:227-229

- Foka ZJ, Lambropoulos AF, Makris PE,
Constantinidis TC, Kotsis A. High frequency of factor V Leiden and
prothrombin G20210A mutations in Greek hemophiliacs. J Thromb Haemost.
2003;1:1116-1167

- Hatzaki A, Anagnostopoulou E,
Metaxa-Mariatou V, Melissinos C, Philalithis P, Iliadis K, Kontaxis A,
Liberatos K, Pangratis N, Nasioulas G. The impact of heterozygosity for
the factor V Leiden and factor II G20210A mutations on the risk of
thrombosis in Greek patients. Int Angiol. 2003;22:79-82 PMid:7482395

- Zalavras ChG, Giotopoulou S, Dokou E,
Mitsis M, Ioannou HV, Tsaousi C, Tzolou A, Kolaitis N, Vartholomatos G.
Prevalence of the G20210A prothrombin gene mutation in Northwestern
Greece and association with venous thromboembolism. Int Angiol.
2003;22:55-57

- Agorastos T, Karavida A, Lambropoulos A,
Constantinidis T, Tzitzimikas S, Chrisafi S, Saravelos H, Vavilis D,
Kotsis A, Bontis J. Factor V Leiden and prothrombin G20210A mutations
in pregnancies with adverse outcome. J Matern Fetal Neonatal Med.
2002;12:267-273

- Antoniadi T, Hatzis T, Kroupis C,
Economou-Petersen E, Petersen MB. Prevalence of factor V Leiden,
prothrombin G20210A, and MTHFR C677T mutations in a Greek population of
blood donors. Am J Hematol. 1999;61:265-267 PMid:9002940

- Tug E, Aydin H, Kaplan E, Dogruer D.
Frequency of genetic mutations associated with thromboembolism in the
Western Black Sea Region. Intern Med. 2011;50:17-21 PMid:8950768

- Altinisik J, Ates O, Ulutin T, Cengiz M,
Buyru N. Factor V Leiden, prothrombin G20210A, and protein C mutation
frequency in Turkish venous thrombosis patients. Clin Appl Thromb
Hemost. 2008;14:415-420 PMid:8578439

- Irdem A, Devecioglu C, Batun S, Soker M,
Sucakli IA. Prevalence of factor V Leiden and prothrombin G20210A gene
mutation. Saudi Med J. 2005;26:580-583 PMid:8916933

- Gurgey A, Haznedaroglu IC, Egesel T,
Buyukasik Y, Ozcebe OI, Sayinalp N, Dundar SV, Bayraktar Y. Two common
genetic thrombotic risk factors: factor V Leiden and prothrombin
G20210A in adult Turkish patients with thrombosis. Am J Hematol.
2001;67:107-111 PMid:14717975

- Xenophontos SL, Hadjivassiliou M, Ayrton
N, Karagrigoriou A, Pantzaris M, Nicolaides AN, Cariolou MA. Spectrum
and prevalence of prothrombotic single nucleotide polymorphism profiles
in the Greek Cypriot population. Int Angiol. 2002;21:322-329
PMid:20385790

- Angelopoulou K, Nicolaides A, Constantinou
Deltas C. Prevalence of genetic mutations that predispose to
thrombophilia in a Greek Cypriot population. Clin Appl Thromb Hemost.
2000;6:104-107 PMid:20229688

- Hessner MJ, Luhm RA, Pearson SL, Endean
DJ, Friedman KD, Montgomery RR. Prevalence of prothrombin G20210 A,
factor V G1691 A (Leiden), and methyltetrahydrofolate reductase (MTHFR)
C 677T in seven different populations determined by multiple
allele-specific PCR. Thromb Haemost. 1999;81:733-738 PMid:9299960

- Dowling NF, Austin H, Dilley A, Whitsett
C, Evatt BL, Hooper WC. The epidemiology of venous thromboembolism in
Caucasians and African-Americans: the GATE Study. J Thromb Haemost.
2003;1:80-87 PMid:9241710

- Tang Y, Sampson B, Pack S, Shah K, Yon Um
S, Wang D, Wang T, Prinz M. Ethnic differences in out-of-hospital fatal
pulmonary embolism. Circulation. 2011;123:2219-2225 PMid:9308741

- Zakai NA, McClure LA. Racial Differences
in Venous
Thromboembolism. J Thromb Haemost. 2011; http://dx.doi.org/10.
1111/j.1538-7836.2011.04443.x

- Franco RF, Santos SE, Elion J, Tavella MH,
Zago MA.
Prevalence of the G20210A polymorphism in the 3'-untranslated region of
the prothrombin gene in different human populations. Acta Haematol.
1998;100:9-12 PMid:18574041

- Gibson CS, MacLennan AH, Rudzki Z, Hague
WM, Haan EA,
Sharpe P, Priest K, Chan A, Dekker GA; South Australian Cerebral Palsy
Research Group. The prevalence of inherited thrombophilias in a
Caucasian Australian population. Pathology. 2005;37:160-163
PMid:9569177

- Zoossmann-Diskin A, Gazit E, Peleg L,
Shohat M, Turner D.
Thrombophilic polymorphisms in Israel. Blood Cells Mol Dis.
2008;41:230-233 PMid:11434083

- Rees DC, Chapman NH, Webster MT, Guerreiro
JF, Rochette J,
Clegg JB. Born to clot: the European burden. Br J Haematol.
1999;105:564-566

- Dilley A, Austin H, Hooper WC, El-Jamil M,
Whitsett C,
Wenger NK, Benson J, Evatt B. Prevalence of the prothrombin 20210
G-to-A variant in blacks: infants, patients with venous thrombosis,
patients with myocardial infarction, and control subjects. J Lab Clin
Med. 1998;132:452-455

- Mack R, Chowdary D, Streck D, Dermody J.
Inherited thrombophilia genes in minorities. Genet Test. 1999;3:371-373
PMid:21422408

- Ruiz-Argüelles GJ, Garcés-Eisele J,
Reyes-Núñez V,
Ramírez-Cisneros FJ. Primary thrombophilia in Mexico. II. Factor V
G1691A (Leiden), prothrombin G20210A, and methylenetetrahydrofolate
reductase C677T polymorphism in thrombophilic Mexican mestizos. Am J
Hematol. 2001;66:28-31

- Ruiz-Argüelles GJ, López-Martínez B,
Valdés-Tapia P,
Gómez-Rangel JD, Reyes-Núñez V, Garcés-Eisele J. Primary thrombophilia
in Mexico. V. A comprehensive prospective study indicates that most
cases are multifactorial. Am J Hematol. 2005;78:21-26

- Jun ZJ, Ping T, Lei Y, Li L, Ming SY, Jing
W. Prevalence of
factor V Leiden and prothrombin G20210A mutations in Chinese patients
with deep venous thrombosis and pulmonary embolism. Clin Lab Haematol.
2006;28:111-116 PMid:18004248

- Lu Y, Zhao Y, Liu G, Wang X, Liu Z, Chen
B, Hui R. Factor V
gene G1691A mutation, prothrombin gene G20210A mutation, and MTHFR gene
C677T mutation are not risk factors for pulmonary thromboembolism in
Chinese population. Thromb Res. 2002 1;106:7-12

- Sakuma M, Shirato K. The epidemiology of
acute pulmonary thromboembolism. Nihon Rinsho. 2003;61:1706-1712

- Miyata T, Kawasaki T, Fujimura H, Uchida
K, Tsushima M,
Kato H. The prothrombin gene G20210A mutation is not found among
Japanese patients with deep vein thrombosis and healthy individuals.
Blood Coagul Fibrinolysis. 1998;9:451-452

- Chang JD, Hur M, Lee SS, Yoo JH, Lee KM.
Genetic background
of nontraumatic osteonecrosis of the femoral head in the Korean
population. Clin Orthop Relat Res. 2008;466:1041-1046

- Kim YH, Kim JS. The 2007 John Charnley
Award. Factors
leading to low prevalence of DVT and pulmonary embolism after THA:
analysis of genetic and prothrombotic factors. Clin Orthop Relat Res.
2007;465:33-39

- Shen MC, Lin JS, Tsay W. Protein C and
protein S
deficiencies are the most important risk factors associated with
thrombosis in Chinese venous thrombophilic patients in Taiwan. Thromb
Res. 2000;99:447-452

- Lin JS, Shen MC, Tsay W. The mutation at
position 20210 in
the 3'-untranslated region of the prothrombin gene is extremely rare in
Taiwanese Chinese patients with venous thrombophilia. Thromb Haemost.
1998;80:343

- Newton LJ, Krishnan A, Parapia LA. Born to
clot: the European burden. Br J Haematol. 1999;107:213

- Kumar SI, Kumar A, Srivastava S, Saraswat
VA, Aggarwal R.
Low frequency of factor V Leiden and prothrombin G20210A mutations in
patients with hepatic venous outflow tract obstruction in northern
India: a case-control study. Indian J Gastroenterol. 2005;24:211-215
PMid:16361766

- Ghosh K, Shetty S, Madkaikar M, Pawar A,
Nair S, Khare A,
Pathare A, Jijina F, Mohanty D. Venous thromboembolism in young
patients from western India: a study. Clin Appl Thromb Hemost.
2001;7:158-165 http://dx.doi.org/10.1177/107602960100700214
PMid:11292195

- Angeline T, Bentley HA, Hawk AB, Manners
RJ, Mokashi HA,
Jeyaraj N, Tsongalis GJ. Prevalence of the Factor V G1691A and the
Factor II/prothrombin G20210A gene polymorphisms among Tamilians. Exp
Mol Pathol. 2005;79:9-13 http://dx.doi.org/10.1016/j.yexmp.2005.03.003
PMid:15896772

- Garewal G, Das R, Ahluwalia J, Mittal N,
Varma S.
Prothrombin G20210A is not prevalent in North India. J Thromb Haemost.
2003;1:2253-2254 http://dx.doi.org/10.1046/j.1538-7836.2003.00430.x
PMid:14521619

- Bennett JA, Palmer LJ, Musk AW, Erber WN.
Prevalence of
factor V Leiden and prothrombin 20210A mutations in indigenous
Australians. Thromb Haemost. 2001;86:1592-1593 PMid:11776339

- Tamim H, Finan RR, Almawi WY. Prevalence
of two
thrombophilia predisposing mutations: factor V G1691A (R506Q; Leiden)
and prothrombin G20210A, among healthy Lebanese. Thromb Haemost.
2002;.88:691-692

- Finan RR, Tamin H, Amen G, Sharide HE,
Rasid M, Alunen WY.
Factor V G1691A and factor II G20210A mutations. Am J Hematol.
2002;71:300-305http://dx.doi.org/10.1002/ajh.10223
PMid:12447960

- Sabbagh AS, Ibrahim G, Kanaan Z, Shammaa
DM, Khalek RA,
Ghasham M, Greige L, Mahfouz RA. Prevalence of the prothrombin G20210A
polymorphism in the Lebanese population: use of a reverse hybridization
strip assay approach. Mol Biol Rep. 2009;36:399-403 http://dx.doi.org/10.1007/s11033-007-9193-0
PMid:18066679

- Bouaziz-Borgi L, Almawi WY, Mtiraoui N,
Nsiri B, Keleshian
SH, Kreidy R, Louzir B, Hezard N, Mahjoub T. Distinct association of
factor V-Leiden and prothrombin G20210A mutations with deep venous
thrombosis in Tunisia and Lebanon. Am J Hematol. 2006;81:641-643 http://dx.doi.org/10.1002/ajh.20582
PMid:16823828

- Almawi WY, Keleshian SH, Borgi L, Fawaz
NA, Abboud N,
Mtiraoui N, Mahjoub T. Varied prevalence of factor V G1691A (Leiden)
and prothrombin G20210A single nucleotide polymorphisms among Arabs. J
Thromb Thrombolysis. 2005;20:163-168 http://dx.doi.org/10.1007/s11239-005-3550-4
PMid:16261289

- Ameen G, Irani-Hakime N, Fawaz NA, Mahjoub
T, Almawi WY. An
Arab selective gradient in the distribution of factor V G1691A
(Leiden), prothrombin G20210A, and methylenetetrahydrofolate reductase
(MTHFR) C677T. J Thromb Haemost. 2005;3:2126-2127 http://dx.doi.org/10.1111/j.1538-7836.2005.01546.x
PMid:16102131

- Dagan E, Brik R, Broza Y, Gershoni-Baruch
R.
Henoch-Schonlein purpura: polymorphisms in thrombophilia genes. Pediatr
Nephrol. 2006;21:1117-1121 http://dx.doi.org/10.1007/s00467-006-0155-x
PMid:16791607

- Attia FM, Mikhailidis DP, Reffat SA.
Prothrombin Gene
G20210A Mutation in Acute Deep Venous Thrombosis Patients with Poor
Response to Warfarin Therapy. Open Cardiovasc Med J. 2009;3:147-151 http://dx.doi.org/10.2174/1874192400903010147
PMid:19920886
PMCid:2778014

- Mahjoub T, Mtiraoui N, Tamim H, Hizem S,
Finan RR, Nsiri B,
Almawi WY. Association between adverse pregnancy outcomes and maternal
factor V G1691A (Leiden) and prothrombin G20210A genotypes in women
with a history of recurrent idiopathic miscarriages. Am J Hematol.
2005;80:12-19 http://dx.doi.org/10.1002/ajh.20419
PMid:16138341

- Mtiraoui N, Borgi L, Hizem S, Nsiri B,
Finan RR, Gris JC,
Almawi WY, Mahjoub T. Prevalence of antiphospholipid antibodies, factor
V G1691A (Leiden) and prothrombin G20210A mutations in early and late
recurrent pregnancy loss. Eur J Obstet Gynecol Reprod Biol.
2005;119:164-170 http://dx.doi.org/10.1016/j.ejogrb.2004.07.003

- Frere C, Saut N, Boukef MK, Zili M, Toumi
NE. Factor V
Leiden G1691A and prothrombin G20210A mutations are common in Tunisia.
J Thromb Haemost. 2003;1:2451-2452 http://dx.doi.org/10.1046/j.1538-7836.2003.0468b.x
PMid:14629484

- Klai S, Fekih-Mrissa N, Rachdi R, Gritli
N. The status of
thrombophilic defects and non-O blood group as risk factors for
gestational vascular complications among Tunisian women. Acta Haematol.
2011;125:115-120 http://dx.doi.org/10.1159/000321934
PMid:21109732

- Helley D, Chafa O, Yaker NL, Reghis A,
Fischer AM.
Prevalence of the prothrombin gene 20210A mutation in thrombophilic and
healthy Algerian subjects. Thromb Haemost. 1999;82:1554-1555
PMid:10595654

- Mathonnet F, Nadifi S, Serazin-Leroy V,
Dakouane M,
Giudicelli Y. Absence of factor V Leiden mutation and low prothrombin G
20210 A mutation prevalence in a healthy Moroccan population. Thromb
Haemost. 2002;88:1073-1074 PMid:12529766

- They-They TP, Hamzi K, Moutawafik MT,
Bellayou H, El Messal
M, Nadifi S. Prevalence of angiotensin-converting enzyme,
methylenetetrahydrofolate reductase, Factor V Leiden, prothrombin and
apolipoprotein E gene polymorphisms in Morocco. Ann Hum Biol.
2010;37:767-777 http://dx.doi.org/10.3109/03014461003738850
PMid:20687780

- They-They TP, Battas O, Slassi I, Rafai
MA, Katumbay DT,
Nadifi S. Prothrombin G20210A and Factor V Leiden Polymorphisms in
Stroke. J Mol Neurosci. 2011 [accepted for publication] http://dx.doi.org/10.1007/s12031-011-9580-9
PMid:21701789

- Zivelin A, Rosenberg N, Faier S, Kornbrot
N, Peretz H,
Mannhalter C, Horellou MH, Seligsohn U. A single genetic origin for the
common prothrombotic G20210A polymorphism in the prothrombin gene.
Blood. 1998, 92(4):1119-24. PMid:9694698
