Skin Manifestations Associated With Mantle Cell Lymphoma: a Case Report
Avinash Kumar Singh1, Gaurav Dixit1, Sanjeev Sharma1, Suman Kumar1, Rajni Yadav2, Narendra Agrawal1, Pravas Mishra1, Tulika Seth1, C.Sarkar2, M.Mahapatra1 and Renu Saxena1
1
Department of Hematology, All India Institute of Medical Sciences, New
Delhi
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi
Correspondence
to: Avinash Kumar Singh, Department of Hematology, All
India Institute of Medical Science, New Delhi, India. E-mail: avinash.pmch@gmail.com
Published: February, 25 2013
Received: December 18, 2012
Accepted: February 20, 2013
Meditter J Hematol Infect Dis 2013, 5(1): e2013020, DOI 10.4084/MJHID.2013.020
This article is available on PDF format at:

This is an Open
Access article
distributed under the terms of the
Creative Commons Attribution License
(http://creativecommons.org/licenses/by/2.0),
which permits
unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited
Abstract
Mantle
cell lymphoma (MCL) is a distinct non-Hodgkin’s lymphoma type that
commonly affects extra nodal sites. The most often affected sites are
bone marrow, gastrointestinal tract and Waldeyer’s ring, being the skin
rarely involved. We report a case of 56 year-old man with MCL,
exhibiting multiple large maculopapular skin rashes and skin ulcers.
Histopathological examination had not shown direct infiltration by any
atypical cells. He had significant improvement of skin lesions with
combination chemotherapy and debridement. Awareness of skin
manifestations of MCL is crucial for dermatologists and haematologists
to establish the early diagnosis and timely administration of
appropriate treatment.
Case Report
A 56 years old indo-aryan black gentleman, farmer by occupation, occasional smoker and alcoholic for more than 20 years, presented to Haematology OPD with complains of weakness and easy fatigability for one month, he also had glandular swellings involving the neck, axilla and inguinal region. He noticed erythematous maculopapular rashes over both upper limbs, 2 days back. There was no history of fever, cough, bleeding, skeletal pain or jaundice. There was no involvement of the oral mucosa by the skin lesions. The past and family history was not significant. On examination, he had generalised lymphadenopathy and massive hepatosplenomegaly. The skin rashes (Figure 1) were maculopapular erythematous, size varying from 4x5 cm to 10x8 cm without any initial itching, pain or secretion. Over 4 to 5 days, the rashes developed blackish discolouration, followed by bullae formation that eventually ruptured.

Figure 1. Skin lesion with central necrosis over right arm.
The blood exam revealed anemia, thrombocytopenia and leucocytosis (WBC = 18000/mm3) with presence of atypical lymphoid cells on peripheral smear. The bone marrow examination showed 45% immature lymphoid cells, negative for MPO, SB, AP, NSE & PAS on cytochemistry. The bone marrow biopsy showed infiltration by atypical lymphoid cells. Immunophenotyping by flow cytometry of bone marrow showed positivity for co-expression of CD19/5, CD19, FMC7, Kappa clonality, CD25, HLADR, CD22, CD20, CD79b, SIgM and negative for co-expression of CD23/5, CD10, CD23, CD11C, CD103, CD2, CD3, CD34, SIgG, TdT. The axillary lymph node biopsy was suggestive of blastoid variant of mantle cell lymphoma, which showed immunopositivity for CD 20, CD43, Cyclin D1, BCL-2, BCL-6 and immunonegative for CD5, CD3, CD10, CD23. The skin biopsy from the left arm maculopapular lesion (including both healthy and affected area) showed congested vessels along with extravasations of RBC in the dermis without any atypical lymphoid cells (Figure 2a and 2b). He received R-CHOP chemotherapy and has undergone debridement (Figure 3) for the skin lesions. Gradually, after 5 cycles of chemotherapy, he has attained complete remission of skin lesions along with disappearance of lymphadenopathy, organomegaly and normalisation of the hemogram.
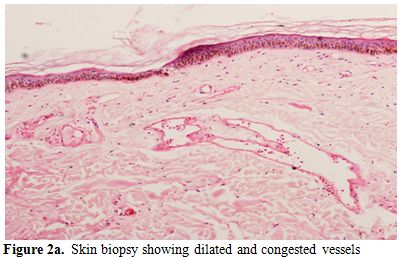
Figure 2a. Skin biopsy showing dilated and congested vessels.

Figure 2b. Skin biopsy showing extravasation RBC in the dermis.

Figure 3. Skin lesion after 4 months.
Discussion
Mantle cell lymphoma (MCL) is a malignant tumor derived from B cells in the mantle zone of lymphoid follicles characterized by specific pathologic, immunophenotypic and molecular genetics features, and usually takes an aggressive clinical course, defined in the World Health Organization (WHO) classification.[1-3] Histologically, it shows a diffuse or nodular monotonous proliferation of small lymphoid cells with scant cytoplasm and irregular nuclear contours in lymphnodes.
Immunophenotypically, the tumor cells are positive for B-cell markers CD79a, CD19, CD20 and CD22 as well as CD5, and are usually negative for CD10 and CD23.[5,6] The majority of MCL have an associated cytogenetic abnormality t(11,14) (q13;q32) translocation, which causes a juxtaposition of the CCND-1 gene on chromosome 11 with the immunoglobulin heavy chain gene on chromosome 14, resulting in an over expression of cyclin D1 protein, that leads to a positive signal for transition to the S phase.[7-9] Cyclin D1 over expression is considered to be an important diagnostic marker for MCL.[10]
MCL frequently involves extra nodal organs, particularly the bone marrow, gastrointestinal tract and Waldeyer’s ring; thus it has been considered in the past as an extracutaneous lymphoma. However, MCL rarely affects the skin. In two large series of 121 and 59 cases of MCL, only 3 and 2 patients respectively had skin lesions, respectively.[3,4] To the best of our knowledge, only 18 cases of mantle cell lymphoma with skin manifestation have been reported in English literature (Table 1).[11,12] The commonly reported sites of skin involvement in MCL are trunk (60%), face (30%) followed by arm (20%), thigh, leg & scalp.[11,12] Skin lesions manifested as nodular lesions in 6 patients (34%), macular or maculopapular lesions, as in our case, in 6 (34%), tumoral or infiltrated plaques in 4 (21%), and subcutaneous nodules in 2 (11%).[11,12]
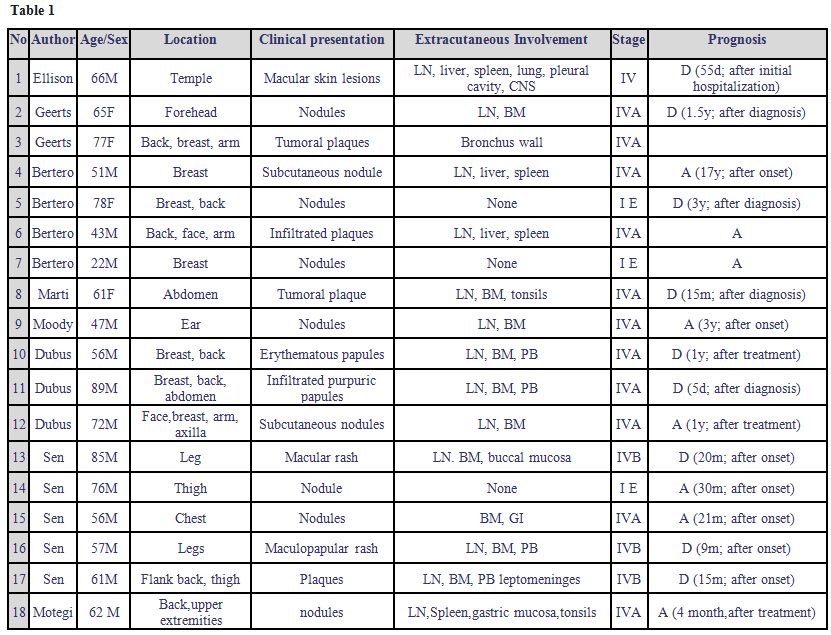
Table 1
In most of the reported cases of skin manifestations of MCL, skin lesion has shown infiltration by atypical lymphoid cells, while a reactive cutaneous eruption, simulating insect bites, has been only incidentally described in association with MCL.[11,13-15] The skin involvement, even if rare, has been most frequently reported in the blastoid variant of MCL as in our case; when present the skin localizations are disseminated and associated with a poor prognosis.[11,12,16] Although, large reactive skin lesions have not been reported previously, the absence of atypical lymphoid cells and the complete remission with chemotherapy suggest that the skin lesions should be considered in the present case as reactive to mantle cell lymphoma; however, the presence of hidden malignant cells in the lesion cannot be excluded. The prognosis of MCL with skin localizations is particularly poor; aggressive chemotherapy may improve the survival rate.[12] As cutaneous lesions can be the first manifestation of MCL, awareness of MCL is crucial for dermatologists and haematologists to establish an early diagnosis and perform an appropriate treatment.
A 56 years old indo-aryan black gentleman, farmer by occupation, occasional smoker and alcoholic for more than 20 years, presented to Haematology OPD with complains of weakness and easy fatigability for one month, he also had glandular swellings involving the neck, axilla and inguinal region. He noticed erythematous maculopapular rashes over both upper limbs, 2 days back. There was no history of fever, cough, bleeding, skeletal pain or jaundice. There was no involvement of the oral mucosa by the skin lesions. The past and family history was not significant. On examination, he had generalised lymphadenopathy and massive hepatosplenomegaly. The skin rashes (Figure 1) were maculopapular erythematous, size varying from 4x5 cm to 10x8 cm without any initial itching, pain or secretion. Over 4 to 5 days, the rashes developed blackish discolouration, followed by bullae formation that eventually ruptured.

Figure 1. Skin lesion with central necrosis over right arm.
The blood exam revealed anemia, thrombocytopenia and leucocytosis (WBC = 18000/mm3) with presence of atypical lymphoid cells on peripheral smear. The bone marrow examination showed 45% immature lymphoid cells, negative for MPO, SB, AP, NSE & PAS on cytochemistry. The bone marrow biopsy showed infiltration by atypical lymphoid cells. Immunophenotyping by flow cytometry of bone marrow showed positivity for co-expression of CD19/5, CD19, FMC7, Kappa clonality, CD25, HLADR, CD22, CD20, CD79b, SIgM and negative for co-expression of CD23/5, CD10, CD23, CD11C, CD103, CD2, CD3, CD34, SIgG, TdT. The axillary lymph node biopsy was suggestive of blastoid variant of mantle cell lymphoma, which showed immunopositivity for CD 20, CD43, Cyclin D1, BCL-2, BCL-6 and immunonegative for CD5, CD3, CD10, CD23. The skin biopsy from the left arm maculopapular lesion (including both healthy and affected area) showed congested vessels along with extravasations of RBC in the dermis without any atypical lymphoid cells (Figure 2a and 2b). He received R-CHOP chemotherapy and has undergone debridement (Figure 3) for the skin lesions. Gradually, after 5 cycles of chemotherapy, he has attained complete remission of skin lesions along with disappearance of lymphadenopathy, organomegaly and normalisation of the hemogram.
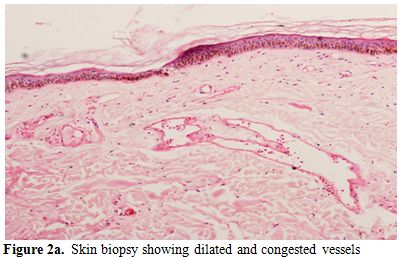
Figure 2a. Skin biopsy showing dilated and congested vessels.

Figure 2b. Skin biopsy showing extravasation RBC in the dermis.

Figure 3. Skin lesion after 4 months.
Discussion
Mantle cell lymphoma (MCL) is a malignant tumor derived from B cells in the mantle zone of lymphoid follicles characterized by specific pathologic, immunophenotypic and molecular genetics features, and usually takes an aggressive clinical course, defined in the World Health Organization (WHO) classification.[1-3] Histologically, it shows a diffuse or nodular monotonous proliferation of small lymphoid cells with scant cytoplasm and irregular nuclear contours in lymphnodes.
Immunophenotypically, the tumor cells are positive for B-cell markers CD79a, CD19, CD20 and CD22 as well as CD5, and are usually negative for CD10 and CD23.[5,6] The majority of MCL have an associated cytogenetic abnormality t(11,14) (q13;q32) translocation, which causes a juxtaposition of the CCND-1 gene on chromosome 11 with the immunoglobulin heavy chain gene on chromosome 14, resulting in an over expression of cyclin D1 protein, that leads to a positive signal for transition to the S phase.[7-9] Cyclin D1 over expression is considered to be an important diagnostic marker for MCL.[10]
MCL frequently involves extra nodal organs, particularly the bone marrow, gastrointestinal tract and Waldeyer’s ring; thus it has been considered in the past as an extracutaneous lymphoma. However, MCL rarely affects the skin. In two large series of 121 and 59 cases of MCL, only 3 and 2 patients respectively had skin lesions, respectively.[3,4] To the best of our knowledge, only 18 cases of mantle cell lymphoma with skin manifestation have been reported in English literature (Table 1).[11,12] The commonly reported sites of skin involvement in MCL are trunk (60%), face (30%) followed by arm (20%), thigh, leg & scalp.[11,12] Skin lesions manifested as nodular lesions in 6 patients (34%), macular or maculopapular lesions, as in our case, in 6 (34%), tumoral or infiltrated plaques in 4 (21%), and subcutaneous nodules in 2 (11%).[11,12]
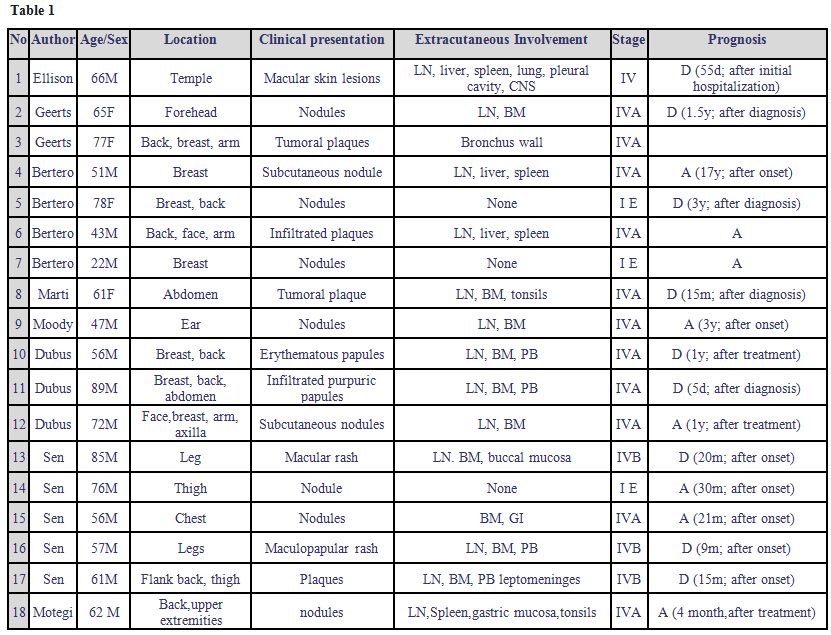
Table 1
In most of the reported cases of skin manifestations of MCL, skin lesion has shown infiltration by atypical lymphoid cells, while a reactive cutaneous eruption, simulating insect bites, has been only incidentally described in association with MCL.[11,13-15] The skin involvement, even if rare, has been most frequently reported in the blastoid variant of MCL as in our case; when present the skin localizations are disseminated and associated with a poor prognosis.[11,12,16] Although, large reactive skin lesions have not been reported previously, the absence of atypical lymphoid cells and the complete remission with chemotherapy suggest that the skin lesions should be considered in the present case as reactive to mantle cell lymphoma; however, the presence of hidden malignant cells in the lesion cannot be excluded. The prognosis of MCL with skin localizations is particularly poor; aggressive chemotherapy may improve the survival rate.[12] As cutaneous lesions can be the first manifestation of MCL, awareness of MCL is crucial for dermatologists and haematologists to establish an early diagnosis and perform an appropriate treatment.
References
- Burg G, Jaffe ES,
Kempf W, Berti E, Cerroni
L, Chimenti S, et al., WHO/EORTC. Classification of cutaneous
lymphomas. In: Weedon D, LeBoit P, Burg G, Sarasin A, eds. Pathology
and Genetics of Skin Tumors: WHO Classification of Tumors. Lyon:
IARC,2005: 166.
- Swerdlow SH,
Kurrer M, Bernengo M, Buchner
S. Cutaneous involvement in primary extracutaneous B-cell lymphoma. In:
Weedon D, LeBoit P, Burg G, Sarasin A, eds. Pathology and Genetics of
Tumors of the Skin: WHO Classification of Tumors. Lyon: IARC, 2005:
204-6.
- Swerdlow SH,
Nathwani BN, Berger F, Piris
MA, Isaacson PI, Harris NL, et al. Mantle cell lymphoma. In: Jaffe E,
Harris N, Stein H, Vardiman J, eds. Pathology and Genetics of Tumors of
Haematopoietic and Lymphoid Tissue:WHO Classification of tumors. Lyon:
IARC, 2001: 168-70.
- Samaha H, Dumontet
C, Ketterer N, Moullet
I, Thieblemont C, Bouafia F, et al. Mantle cell lymphoma: a
retrospective study of 121 cases. Leukemia 1998; 12: 1281-7. http://dx.doi.org/10.1038/sj.leu.2401121
PMid:9697885

- Banks PM, Chan J,
Cleary ML, Delsol G, De
Wolf-Peeters C, Gatter K, et al. Mantle cell lymphoma. A proposal for
unification of morphologic, immunologic, and molecular data. Am J Surg
Pathol 1992; 16: 637-40. http://dx.doi.org/10.1097/00000478-199207000-00001
PMid:1530105

- Pittaluga S,
Wlodarska I, Stul MS, Thomas
J, Verhoef G, Cassiman JJ, et al. Mantle cell lymphoma: a
clinicopathological study of 55 cases. Histopathology 1995; 26: 17-24. http://dx.doi.org/10.1111/j.1365-2559.1995.tb00615.x
PMid:7713480

- Seto M, Yamamoto
K, Iida S, Akao Y, Utsumi
KR, Kubonishi I, et al. Gene rearrangement and overexpression of PRAD1
in lymphoid malignancy with t(11;14)(q13;q32) translocation. Oncogene
1992; 7: 1401-6. PMid:1535701

- Yang WI, Zukerberg
LR, Motokura T, Arnold
A, Harris NL. Cyclin D1 (Bcl-1, PRAD1) protein expression in low-grade
B-cell lymphomas and reactive hyperplasia. Am J Pathol 1994; 145:
86-96. PMid:7518196 PMCid:1887308

- Dubus P, Young P,
Beylot-Barry M,
Belaud-Rotureau MA, Courville P, Vergier B, et al. Value of interphase
FISH for the diagnosis of t(11:14)(q13;q32) on skin lesions of mantle
cell lymphoma. Am J Clin Pathol 2002; 118: 832-41. http://dx.doi.org/10.1309/508R-YBWW-Y0AC-82GA
PMid:12472275

- Yatabe Y, Suzuki
R, Tobinai K, Matsuno Y,
Ichinohasama R, Okamoto M et al. Significance of cyclin D1
overexpression for the diagnosis of mantle cell lymphoma: a
clinicopathologic comparison of cyclin D1-positive MCL and cyclin
D1-negative MCL-like B-cell lymphoma. Blood 2000; 1: 2253-61.

- Motegi S, Okada
E, Nagai Y, Tamura A,
Ishikawa O. Skin manifestation of mantle cell lymphoma. Eur J Dermatol
2006; 16 (4): 435-8 PMid: 6935806

- Canpolat F, Taş
E, Albayrak Sönmez A,
Oktay M, Eskioğlu F, Alper M. Cutaneous Presentation of Mantle Cell
Lymphoma. Acta Derm Venereol 90, 2010;548-550 PMID: 20814647

- Barzilai A,
Shpiro D, Goldberg I,
Yacob-Hirsch Y, Diaz- Cascajo C, Meytes D, et al. Insect bite-like
reaction in patients with hematologic malignant neoplasms. Arch
Dermatol 1999; 135: 1503-7. http://dx.doi.org/10.1001/archderm.135.12.1503
PMid:10606056

- Dodiuk-Gad RP,
Dann EJ, Bergman R. Insect
bite-like reaction associated with mantle cell lymphoma: a report of
two cases and review of the literature. Int J Dermatol 2004; 43: 754-8.
http://dx.doi.org/10.1111/j.1365-4632.2004.02145.x
PMid:15485536

- Khamaysi Z,
Dodiuk-Gad RP, Weltfriend S,
Ben-Arieh Y, Dann EJ, Sahar D, et al. Insect bite-like reaction
associated with mantle cell lymphoma: clinicopathological,
immunopathological, and molecular studies. Am J Dermatopathol
2005;27:290-5. http://dx.doi.org/10.1097/01.dad.0000164607.41402.40
PMid:16121047

- Senff NJ,
Noordijk EM, Kim YH, Bagot M,
Berti E, Cerroni L, et al. European Organization for Research and
Treatment of Cancer and International Society for Cutaneous
Lymphomaconsensus recommendations for the management of cutaneous
B-cell lymphomas. Blood 2008; 112: 1600–1609. http://dx.doi.org/10.1182/blood-2008-04-152850
PMid:18567836
