Changes of von Willebrand Factor during Pregnancy in Women with and without von Willebrand Disease
Giancarlo Castaman
Hemophilia and Thrombosis Center, Department of Cell Therapy and Hematology, San Bortolo Hospital, Vicenza, Italy.
Correspondence
to:
Giancarlo Castaman, M.D., Department of Cell Therapy and Hematology,
Hemophilia and Thrombosis Center, San Bortolo Hospital, 36100 Vicenza,
Italy. Tel: +39444753679; Fax: +39444753922. E-mail: castaman@hemato.ven.it
Published: July 16, 2013
Received: May 25, 2013
Accepted: June 10, 2013
Meditter J Hematol Infect Dis 2013, 5(1): e2013052, DOI 10.4084/MJHID.2013.052
This article is available on PDF format at:

This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License
(http://creativecommons.org/licenses/by/2.0),
which permits
unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited
Abstract
Delivery
in von Willebrand disease (VWD) represents a significant hemostatic
challenge because of the variable pattern of changes observed during
pregnancy of von Willebrand factor (VWF) and factor VIII (FVIII), the
protein carried by VWF. Since a wide heterogeneity of phenotypes and of
the underlying pathophysiological mechanisms is associated with this
disorder, a prompt and careful evaluation of pregnant women with VWD is
requested in order to plan the most appropriate treatment at time of
parturition. VWF and FVIII increase significantly during pregnancy in
normal women, already within the first trimester, reaching levels by
far >100 U/dL by the time of parturition. Women with VWD, levels at
baseline of VWF and FVIII >30 U/dL have us a high likelihood to
achieve normal levels at the end of pregnancy; thus specific
anti-hemorrhagic prophylaxis is seldom required. Women with basal level
<20 U/dL usually have a poor increase since most of these women
carry mutations associated with increased VWF clearance or are compound
heterozygous for different VWF mutations; that prevent the achievement
of satisfactory hemostatic levels. While women with mutations
associated with increased clearance show a full, albeit transitory
correction of their hemostatic deficiency after desmopressin
administration, compound heterozygous need replacement therapy because
they do not respond well to this agent. Patients with abnormal
VWF:RCo/VWF:Ag ratio at baseline (e.g. <0.6), typically associated
with type 2 VWD, maintain the abnormality throughout pregnancy and
VWF:RCo usually does not attain safe levels ≥50 U/dL. These women
require replacement therapy with VWF-FVIII concentrates. Delayed
post-partum bleeding may occur when replacement therapy is not
continued for some days. Tranexamic acid may be useful at discharge to
avoid excessive lochia.
Introduction
Von Willebrand disease (VWD) is a common autosomal inherited bleeding disorder caused by quantitative or qualitative defects of von Willebrand factor (VWF), a multi-adhesive protein which binds platelets to exposed subendothelium and carries factor VIII (FVIII) in circulation.[1,2] As a consequence, FVIII, the protein deficient in hemophilia A, may be variably reduced. Clinical manifestations are mainly represented by mucous membrane and soft tissue bleeding and their severity is variable depending on the degree of VWF and FVIII reduction.[2] Women with VWD are at particularly high risk of bleeding because of menorrhagia and delivery.
Women may undergo to naturally-occurring physiological events (menstruation, pregnancy and parturition) that may cause undue bleeding complications even in absence of a specific bleeding disorder. At the time of delivery, several obstetric complications may cause bleeding with or without associated hematologic alterations.[3] A standard definition of post-partum hemorrhage (PPH) considers the threshold of 500 mL blood loss for vaginal delivery and of 1,000 mL for caesarean section.[4] Rates of PPH in Western Countries based on hospital discharge may range from 3 to 6%, while cases needing blood transfusion are as low as 1%.[3]
Uterine atony is still the leading cause of hemorrhage at parturition accounting for approximately 75% of all cases with PPH and may be burdened with a high risk of being transfused or even death in otherwise healthy women.[3,5] Of course, these complications may add to the inherent risk of bleeding in women with inherited bleeding disorder.
Risk of bleeding at parturition in women with von Willebrand disease
There are conflicting results in the literature about the correct estimation of the risk and the severity of bleeding at parturition in women with VWD. Historical series reported percentages of VWD women with post-partum bleeding ranging from 15 to 60%.[6-10] This uncertainty is also reported when women with wide range of basal FVIII and VWF are included among the type 1 patients. In the MCMDM-1VWD study no difference of bleeding risk at parturition was observed between women with VWD and their normal relatives.[11] In a recent large case-control study from the USA including 4067 deliveries in women with VWD based on all pregnancy-related discharge codes for the years 2000-2003, they were more likely to experience PPH (OR 1.5; 95% CI 1.1-2.0) and had a fivefold increased risk of being transfused (OR 4.7; 95% CI 3.2-7.0) compared with women without VWD.[12] However, no data about anti-hemorrhagic prophylaxis and adequacy of treatment was available and thus it is not possible to give a reliable figure of the risk. Furthermore, in this study, women with VWD were 10 times more likely to experience other ante-partum bleeding (OR 10.2; 95% CI 7.1-14.6),[12] but this latter data was not confirmed in a recent study where the risk of PPH in women with VWD was similar to that of normal women.[13]
Only a single study has tackled the estimation of the risk of bleeding occurring in women before the diagnosis of VWD was made.[14] This is important since in this case no prophylactic anti-hemorrhagic treatment was administered and thus the results reflect the unmodified risk of bleeding in these women. In the IMS study, for the first time a structured bleeding questionnaire was used and grading the severity of the symptoms allowed the estimation of the risk of bleeding and its severity between women belonging to families with a clear autosomal dominant type 1 VWD and normal women (Table 1).[14] The risk of receiving blood transfusion, undergoing uterine dilation/curettage or suturing was about 8-fold greater in VWD women. Furthermore, the risk of hysterectomy for post-partum bleeding was extremely high. Thus, women with VWD without treatment have a clear risk of post-partum bleeding if untreated. However, again this risk may vary depending on the pathophysiologic mechanisms causing VWF deficiency and the inherent likelihood to achieve normal levels at the end of pregnancy (see below).
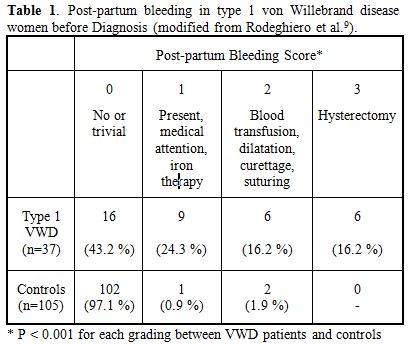
Table 1. Post-partum bleeding in type 1 von Willebrand disease women before Diagnosis (modified from Rodeghiero et al.[9]).
Factor VIII and von Willebrand factor changes during pregnancy in normal women and women with von Willebrand disease
Pregnancy is considered as a hypercoagulable state because the increase of several hemostatic factors is observed. Factor VII, X, fibrinogen and plasminogen activator inhibitor type 1 do increase, but free protein S decrease.[15] The common view considers these changes to be in preparation for the hemostatic challenge of delivery. Also VWF and FVIII increase significantly during pregnancy in normal women and the greatest increase is evident during the third trimester, with levels far exceedingly >100 U/dL by the time of parturition.
A progressive increase of these moieties is also evident in women with type 1 VWD, the partial quantitative deficiency of the disorder, with levels >50 U/dL in the third trimester.[16] However, owing to the wide heterogeneity of phenotypes and genotypes underlying also this type, this general statement needs to be interpreted cautiously and careful evaluation of any pregnant woman with a diagnosis of VWD is recommended. In general, women with levels at baseline of VWF and FVIII >30 U/dL show usually a high likelihood to achieve normal levels at the end of pregnancy.[17] Women with basal level <20 U/dL usually have a poor increase since most of these women carry mutations associated with increased VWF clearance or are compound heterozygous for different VWF mutations which prevent the achievement of physiologically satisfactory hemostatic levels.[18,19] Some frequent autosomal dominant mutations (e.g. R1205H, C1130F) are associated with an increased clearance of VWF, as documented by an increased VWF propeptide/VWF:Ag ratio,[20] which do not allow the achievement of significant levels at the end of pregnancy.[21,22] Similarly, women with compound heterozygosity for null and missense mutations, associated with clearly measurable FVIII/VWF levels do not achieve significant improvements during pregnancy.[19] Since the genetic background which is highly predictive of the type of response to desmopressin and changes during pregnancy is no available for most of these patients,[19] a careful monitoring during pregnancy or at least during the third trimester is highly recommended to identify those who will need specific treatment.
Type 2A VWD is characterized by the lack of high molecular weight multimers and an abnormal VWF:RCo/VWF:Ag (<0.6).[19] During pregnancy, multimer abnormality does not correct. A significant increase of FVIII and VWF:Ag may occur, but VWF:RCo remains markedly reduced.
Worsening of an already existing thrombocytopenia is the most important change observed in type 2B VWD women during pregnancy because an increased release of abnormal multimers with enhanced affinity for glycoprotein Ib on platelet surface occurs.[23,24] However, the severity of this phenomenon is strongly dependent on the type of mutations in A1 domain of VWF responsible for this type, with some mutations showing normal platelet count (e.g., P1266L) while others being associated with severe thrombocytopenia (e.g. R1308C, M1316V).[25] In any case, platelet count should be also closely monitored during pregnancy in women with this type.
Type 2M women usually show a significant correction of FVIII and VWF:Ag, while VWF:RCo does not attain levels around 50 U/dL, as is usually observed after desmopressin.[19,26]
In type 2N, normalization of FVIII, which is more reduced compared to VWF in this type, usually occurs in women heterozygous or homozygous for the most frequent mutation R854Q responsible for this type,[27] while information with the rarer mutations is still scanty.
Women with typical type 3 VWD do not show any change during VWF because their endothelial VWF stores are lacking.
Figure 1 summarizes the typical pattern of FVIII and VWF modifications occurring during normal pregnancy and in women with the more frequent types of VWD.
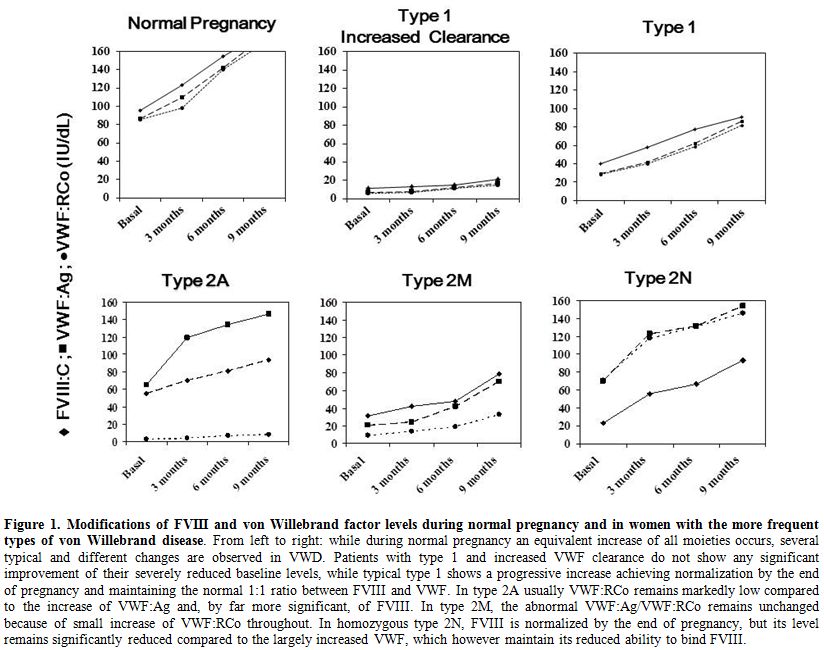
Figure 1. Modifications of FVIII and von Willebrand factor levels during normal pregnancy and in women with the more frequent types of von Willebrand disease.
Treatment of women with von Willebrand disease at delivery
Since pregnant women with VWD are at increased risk of postpartum hemorrhage if untreated,[12,14-16] treatment options should be already planned at the beginning of pregnancy. Invasive management of delivery with ventouse, rotational forceps etc should be avoided for the risk of bleeding for the neonate potentially affected.[2,19] Ideally, the results of a test-infusion with desmopressin should be available before pregnancy for every woman with VWD and basal level of FVIII and VWF <30 U/dL.[28] However, choosing the treatment at parturition on the basis of basal levels alone, without knowledge of mutational background and/or the modifications of FVIII and VWF during pregnancy could be risky since several heterogeneous patterns are possible. In general, VWD patients should be monitored for VWF:RCo and FVIII:C at least once during the third trimester of pregnancy.[14] The risk of bleeding is minimal when FVIII:C and VWF:RCo levels are around or higher than 50 U/dL.[19,29,30]
In type 1 VWD pregnant women with FVIII:C and/or VWF levels lower than 30 U/dL, the administration of desmopressin usually after umbilical clamping and for 3-4 days thereafter is required,[2,19] especially when midline episiotomy is required. Urinary output and fluid restriction are advisable to avoid the risk of hyponatremia.[2] The same approach, with less infusions can be applied to those with VWF >30 and <50 U/dL. A recent experience suggests the possibility to start treatment immediately before delivery, without evident side-effects for the mother and the newborn.[26] The use of desmopressin during the first trimester of pregnancy to cover chorionic villus sampling or amniocentesis appears to be feasible and safe, without risk of miscarriage.[32]
In type 3 VWD women, VWF and FVIII do not increase during pregnancy and thus VWF/FVIII concentrates may be required during pregnancy to control intermittent vaginal bleeding and at delivery or for Cesarean section.[2,19,29,30] The latter should be reserved only for the usual obstetrical indications. Daily doses of 50 IU/kg VWF are required to maintain FVIII:C level >50 U/dL for 3-4 days.[29,30] Usual thrombo-prophylactic treatment with LMWH should be implemented in patients at high risk of venous thrombosis during replacement therapy for caesarean section.[2] If performed, VWF:RCo and FVIII:C peak levels should be >50 U/dL.[29,30]
In patients with type 2A, 2B and 2M usually VWF:RCo does not attain normal levels and thus replacement therapy is similarly advised.[2,29,30] However, in VWD 2B the increase of the abnormal VWF can cause or worsen thrombocytopenia[23-25] and platelet concentrate transfusion could be also required at parturition.[33]
FVIII and VWF fall to baseline levels soon after delivery[16,17,19] and thus oral antifibrinolytic agents (e.g., tranexamic acid 1 gr every 8 hours for 3-4 days) can be used during this period to prevent delayed postpartum bleeding due to heavy lochia.
Von Willebrand disease (VWD) is a common autosomal inherited bleeding disorder caused by quantitative or qualitative defects of von Willebrand factor (VWF), a multi-adhesive protein which binds platelets to exposed subendothelium and carries factor VIII (FVIII) in circulation.[1,2] As a consequence, FVIII, the protein deficient in hemophilia A, may be variably reduced. Clinical manifestations are mainly represented by mucous membrane and soft tissue bleeding and their severity is variable depending on the degree of VWF and FVIII reduction.[2] Women with VWD are at particularly high risk of bleeding because of menorrhagia and delivery.
Women may undergo to naturally-occurring physiological events (menstruation, pregnancy and parturition) that may cause undue bleeding complications even in absence of a specific bleeding disorder. At the time of delivery, several obstetric complications may cause bleeding with or without associated hematologic alterations.[3] A standard definition of post-partum hemorrhage (PPH) considers the threshold of 500 mL blood loss for vaginal delivery and of 1,000 mL for caesarean section.[4] Rates of PPH in Western Countries based on hospital discharge may range from 3 to 6%, while cases needing blood transfusion are as low as 1%.[3]
Uterine atony is still the leading cause of hemorrhage at parturition accounting for approximately 75% of all cases with PPH and may be burdened with a high risk of being transfused or even death in otherwise healthy women.[3,5] Of course, these complications may add to the inherent risk of bleeding in women with inherited bleeding disorder.
Risk of bleeding at parturition in women with von Willebrand disease
There are conflicting results in the literature about the correct estimation of the risk and the severity of bleeding at parturition in women with VWD. Historical series reported percentages of VWD women with post-partum bleeding ranging from 15 to 60%.[6-10] This uncertainty is also reported when women with wide range of basal FVIII and VWF are included among the type 1 patients. In the MCMDM-1VWD study no difference of bleeding risk at parturition was observed between women with VWD and their normal relatives.[11] In a recent large case-control study from the USA including 4067 deliveries in women with VWD based on all pregnancy-related discharge codes for the years 2000-2003, they were more likely to experience PPH (OR 1.5; 95% CI 1.1-2.0) and had a fivefold increased risk of being transfused (OR 4.7; 95% CI 3.2-7.0) compared with women without VWD.[12] However, no data about anti-hemorrhagic prophylaxis and adequacy of treatment was available and thus it is not possible to give a reliable figure of the risk. Furthermore, in this study, women with VWD were 10 times more likely to experience other ante-partum bleeding (OR 10.2; 95% CI 7.1-14.6),[12] but this latter data was not confirmed in a recent study where the risk of PPH in women with VWD was similar to that of normal women.[13]
Only a single study has tackled the estimation of the risk of bleeding occurring in women before the diagnosis of VWD was made.[14] This is important since in this case no prophylactic anti-hemorrhagic treatment was administered and thus the results reflect the unmodified risk of bleeding in these women. In the IMS study, for the first time a structured bleeding questionnaire was used and grading the severity of the symptoms allowed the estimation of the risk of bleeding and its severity between women belonging to families with a clear autosomal dominant type 1 VWD and normal women (Table 1).[14] The risk of receiving blood transfusion, undergoing uterine dilation/curettage or suturing was about 8-fold greater in VWD women. Furthermore, the risk of hysterectomy for post-partum bleeding was extremely high. Thus, women with VWD without treatment have a clear risk of post-partum bleeding if untreated. However, again this risk may vary depending on the pathophysiologic mechanisms causing VWF deficiency and the inherent likelihood to achieve normal levels at the end of pregnancy (see below).
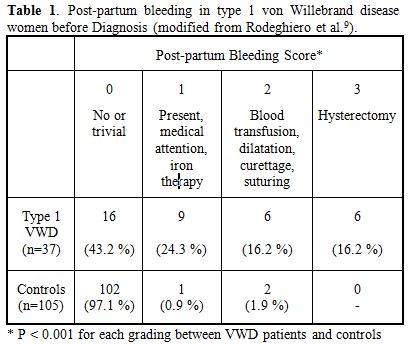
Table 1. Post-partum bleeding in type 1 von Willebrand disease women before Diagnosis (modified from Rodeghiero et al.[9]).
Factor VIII and von Willebrand factor changes during pregnancy in normal women and women with von Willebrand disease
Pregnancy is considered as a hypercoagulable state because the increase of several hemostatic factors is observed. Factor VII, X, fibrinogen and plasminogen activator inhibitor type 1 do increase, but free protein S decrease.[15] The common view considers these changes to be in preparation for the hemostatic challenge of delivery. Also VWF and FVIII increase significantly during pregnancy in normal women and the greatest increase is evident during the third trimester, with levels far exceedingly >100 U/dL by the time of parturition.
A progressive increase of these moieties is also evident in women with type 1 VWD, the partial quantitative deficiency of the disorder, with levels >50 U/dL in the third trimester.[16] However, owing to the wide heterogeneity of phenotypes and genotypes underlying also this type, this general statement needs to be interpreted cautiously and careful evaluation of any pregnant woman with a diagnosis of VWD is recommended. In general, women with levels at baseline of VWF and FVIII >30 U/dL show usually a high likelihood to achieve normal levels at the end of pregnancy.[17] Women with basal level <20 U/dL usually have a poor increase since most of these women carry mutations associated with increased VWF clearance or are compound heterozygous for different VWF mutations which prevent the achievement of physiologically satisfactory hemostatic levels.[18,19] Some frequent autosomal dominant mutations (e.g. R1205H, C1130F) are associated with an increased clearance of VWF, as documented by an increased VWF propeptide/VWF:Ag ratio,[20] which do not allow the achievement of significant levels at the end of pregnancy.[21,22] Similarly, women with compound heterozygosity for null and missense mutations, associated with clearly measurable FVIII/VWF levels do not achieve significant improvements during pregnancy.[19] Since the genetic background which is highly predictive of the type of response to desmopressin and changes during pregnancy is no available for most of these patients,[19] a careful monitoring during pregnancy or at least during the third trimester is highly recommended to identify those who will need specific treatment.
Type 2A VWD is characterized by the lack of high molecular weight multimers and an abnormal VWF:RCo/VWF:Ag (<0.6).[19] During pregnancy, multimer abnormality does not correct. A significant increase of FVIII and VWF:Ag may occur, but VWF:RCo remains markedly reduced.
Worsening of an already existing thrombocytopenia is the most important change observed in type 2B VWD women during pregnancy because an increased release of abnormal multimers with enhanced affinity for glycoprotein Ib on platelet surface occurs.[23,24] However, the severity of this phenomenon is strongly dependent on the type of mutations in A1 domain of VWF responsible for this type, with some mutations showing normal platelet count (e.g., P1266L) while others being associated with severe thrombocytopenia (e.g. R1308C, M1316V).[25] In any case, platelet count should be also closely monitored during pregnancy in women with this type.
Type 2M women usually show a significant correction of FVIII and VWF:Ag, while VWF:RCo does not attain levels around 50 U/dL, as is usually observed after desmopressin.[19,26]
In type 2N, normalization of FVIII, which is more reduced compared to VWF in this type, usually occurs in women heterozygous or homozygous for the most frequent mutation R854Q responsible for this type,[27] while information with the rarer mutations is still scanty.
Women with typical type 3 VWD do not show any change during VWF because their endothelial VWF stores are lacking.
Figure 1 summarizes the typical pattern of FVIII and VWF modifications occurring during normal pregnancy and in women with the more frequent types of VWD.
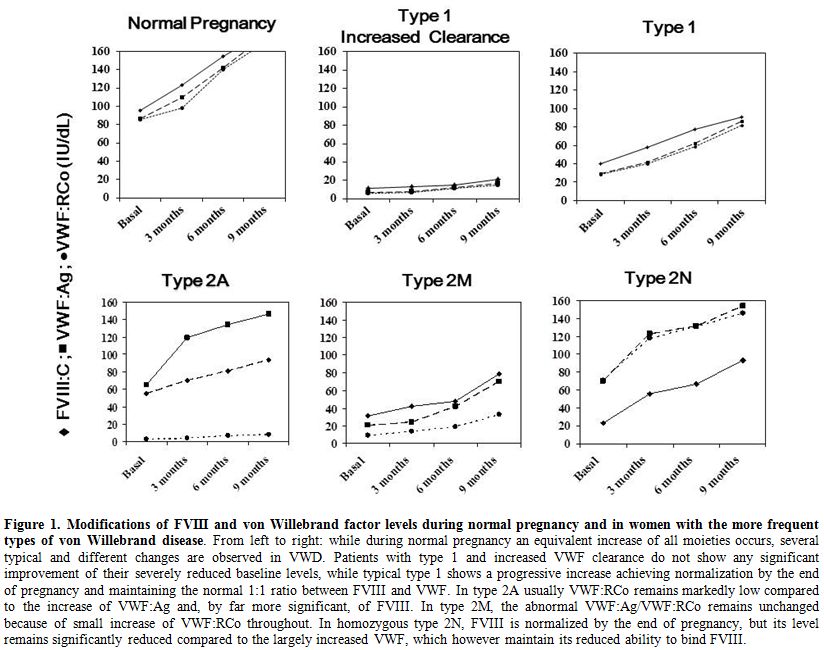
Figure 1. Modifications of FVIII and von Willebrand factor levels during normal pregnancy and in women with the more frequent types of von Willebrand disease.
Treatment of women with von Willebrand disease at delivery
Since pregnant women with VWD are at increased risk of postpartum hemorrhage if untreated,[12,14-16] treatment options should be already planned at the beginning of pregnancy. Invasive management of delivery with ventouse, rotational forceps etc should be avoided for the risk of bleeding for the neonate potentially affected.[2,19] Ideally, the results of a test-infusion with desmopressin should be available before pregnancy for every woman with VWD and basal level of FVIII and VWF <30 U/dL.[28] However, choosing the treatment at parturition on the basis of basal levels alone, without knowledge of mutational background and/or the modifications of FVIII and VWF during pregnancy could be risky since several heterogeneous patterns are possible. In general, VWD patients should be monitored for VWF:RCo and FVIII:C at least once during the third trimester of pregnancy.[14] The risk of bleeding is minimal when FVIII:C and VWF:RCo levels are around or higher than 50 U/dL.[19,29,30]
In type 1 VWD pregnant women with FVIII:C and/or VWF levels lower than 30 U/dL, the administration of desmopressin usually after umbilical clamping and for 3-4 days thereafter is required,[2,19] especially when midline episiotomy is required. Urinary output and fluid restriction are advisable to avoid the risk of hyponatremia.[2] The same approach, with less infusions can be applied to those with VWF >30 and <50 U/dL. A recent experience suggests the possibility to start treatment immediately before delivery, without evident side-effects for the mother and the newborn.[26] The use of desmopressin during the first trimester of pregnancy to cover chorionic villus sampling or amniocentesis appears to be feasible and safe, without risk of miscarriage.[32]
In type 3 VWD women, VWF and FVIII do not increase during pregnancy and thus VWF/FVIII concentrates may be required during pregnancy to control intermittent vaginal bleeding and at delivery or for Cesarean section.[2,19,29,30] The latter should be reserved only for the usual obstetrical indications. Daily doses of 50 IU/kg VWF are required to maintain FVIII:C level >50 U/dL for 3-4 days.[29,30] Usual thrombo-prophylactic treatment with LMWH should be implemented in patients at high risk of venous thrombosis during replacement therapy for caesarean section.[2] If performed, VWF:RCo and FVIII:C peak levels should be >50 U/dL.[29,30]
In patients with type 2A, 2B and 2M usually VWF:RCo does not attain normal levels and thus replacement therapy is similarly advised.[2,29,30] However, in VWD 2B the increase of the abnormal VWF can cause or worsen thrombocytopenia[23-25] and platelet concentrate transfusion could be also required at parturition.[33]
FVIII and VWF fall to baseline levels soon after delivery[16,17,19] and thus oral antifibrinolytic agents (e.g., tranexamic acid 1 gr every 8 hours for 3-4 days) can be used during this period to prevent delayed postpartum bleeding due to heavy lochia.
References
- De Meyer SF, Deckmyn H, Vanhoorelbeke K.
von Willebrand factor to the rescue. Blood. 2009; 113: 5049–57.
http://dx.doi.org/10.1182/blood-2008-10-165621 PMid:19318682

- Castaman G, Goodeve A, Eikenboom J, on
behalf of the European Group on von Willebrand disease (EUVWD).
Principles of care for the diagnosis and treatment of von Willebrand
disease. Haematologica 2013; 98: 667-74.
http://dx.doi.org/10.3324/haematol.2012.077263 PMid:23633542
PMCid:PMC3640108

- McLintock C, James AH. Obstetric
haemorrhage. J Thromb Haemost 2011; 9: 1141-51.
http://dx.doi.org/10.1111/j.1538-7836.2011.04398.x
PMid:21668737

- ACOG. ACOG Practice Bulletin: Clinical
Management Guidelines for Obstetrician-Gynecologists. Number 76,
October 2006: postpartum haemorrhage. Obstet Gynecol 2006; 108:
1039-47. PMid:17012482

- Bateman BT, Berman MF, Riley LE, Leffert
LR. The epidemiology of postpartum haemorrhage in a large, nationwide
sample of deliveries. Anesth Analg 2010; 110: 1368-73.
http://dx.doi.org/10.1213/ANE.0b013e3181d74898
PMid:20237047

- Kirtava A, Drews C, Lally C, Dilley A,
Evatt B. Medical, reproductive and psychosocial experiences of women
diagnosed with von Willebrand's disease receiving care in haemophilia
treatment centres: a case–control study. Haemophilia 2003; 9: 292–7.
http://dx.doi.org/10.1046/j.1365-2516.2003.00756.x
PMid:12694520

- James AH. More than menorrhagia: a review
of the obstetric and gynaecological manifestations of bleeding
disorders. Haemophilia 2005; 11: 295–307.
http://dx.doi.org/10.1111/j.1365-2516.2005.01108.x
PMid:16011580

- Kouides PA, Phatak PD, Burkart P, Braggins
C, Cox C, Bernstein Z, Belling L, Holmberg P, MacLaughlin W, Howard
F.Gynaecological and obstetrical morbidity in women with type I von
Willebrand disease: results of a patient survey. Haemophilia 2000; 6:
643–8. http://dx.doi.org/10.1046/j.1365-2516.2000.00447.x PMid:11122390

- Silwer J. von Willebrand's disease in Sweden. Acta Paediatr Scand Suppl 1973; 238: 1–159. PMid:4550005

- Chi C, Shiltagh N, Kingman CE, Economides
DL, Lee CA, Kadir RA. Identification and management of women with
inherited bleeding disorders: a survey of obstetricians and
gynaecologists in the United Kingdom. Haemophilia 2006; 12: 405–12.
http://dx.doi.org/10.1111/j.1365-2516.2006.01282.x
PMid:16834742

- Tosetto A, Rodeghiero F, Castaman G,
Goodeve A, Federici AB, Budde U, et al. A quantitative analysis of
bleeding symptoms in type 1 von Willebrand disease: results from a
multicenter European study (MCMDM-1 VWD). J Thromb Haemost. 2006; 4:
766-73. http://dx.doi.org/10.1111/j.1538-7836.2006.01847.x PMid:16634745

- James AH, Jamison MG. Bleeding events and
other complications during pregnancy and childbirth in women with von
Willebrand disease. J Thromb Haemost 2007; 5: 1165-9.
http://dx.doi.org/10.1111/j.1538-7836.2007.02563.x
PMid:17403089

- Siboni SM, Spreafico M, Calň L, Maino A,
Santagostino E, Federici AB, Peyvandi F. Gynaecological and obstetrical
problems in women with different bleeding disorders. Haemophilia 2009;
15: 1291-9. http://dx.doi.org/10.1111/j.1365-2516.2009.02072.x
PMid:19664014

- Rodeghiero F, Castaman G, Tosetto A, Batlle
J, Baudo F, Cappelletti A, et al. The discriminant power of bleeding
history for the diagnosis of type 1 von Willebrand disease: an
international, multicenter study. J Thromb Haemost 2005; 3: 2619-26.
http://dx.doi.org/10.1111/j.1538-7836.2005.01663.x
PMid:16359502

- Lee CA, Kadir RA, Kouides PA. Inherited bleeding disorders in women. Wiley-Blackwell, Oxford, 2009.
- Kadir RA, Lee CA, Sabin CA, Pollard D,
Economides DL. Pregnancy in women with von Willebrand's disease or
factor XI deficiency. Br J Obstet Gynaecol 1998; 105: 314-21.
http://dx.doi.org/10.1111/j.1471-0528.1998.tb10093.x
PMid:9532993

- Leone G, Moneta E, Paparatti G, Boni P. von
Willebrand's disease in pregnancy. N Eng J Med 1975; 293: 456.
http://dx.doi.org/10.1056/NEJM197508282930918 PMid:1080256

- Castaman G, Tosetto A, Rodeghiero F.
Shortened von Willebrand Factor survival: pathophysiologic and clinical
relevance. J Thromb Haemost 2009; 7 (Suppl 1): 71-4.
http://dx.doi.org/10.1111/j.1538-7836.2009.03381.x
PMid:19630772

- Castaman G, Tosetto A, Rodeghiero F.
Pregnancy and delivery in women with von Willebrand's disease and
different von Willebrand factor mutations. Haematologica 2010; 95:
963-9. http://dx.doi.org/10.3324/haematol.2009.011239
PMid:19951969 PMCid:PMC2878795

- Haberichter SL, Castaman G, Budde U et al.
Identification of type 1 von Willebrand disease patients with reduced
von Willebrand factor survival by assay of the VWF propeptide in the
European study: molecular and clinical markers for the diagnosis and
management of type 1 VWD (MCMDM-1VWD). Blood 2008; 111: 4979-85.
http://dx.doi.org/10.1182/blood-2007-09-110940 PMid:18344424
PMCid:PMC2384129

- Castaman G, Eikenboom JCJ, Contri A,
Rodeghiero F. Pregnancy in women with type 1 von Willebrand disease
caused by heterozygosity for von Willebrand factor mutation C1130F.
Thromb Haemost 2000; 84: 351-2. PMid:10959713

- Castaman G, Federici AB, Bernardi M, Moroni
B, Bertoncello K, Rodeghiero F. Factor VIII and von Willebrand factor
changes after desmopressin and during pregnancy in type 2M von
Willebrand disease Vicenza: a prospective study comparing patients with
single (R1205H) and double (R1205H-M740I) defect. J Thromb Haemost
2006; 4: 357-60.
http://dx.doi.org/10.1111/j.1538-7836.2006.01706.x
PMid:16420565

- Giles AR, Hoogendoorn H, Benford K. Type
IIB von Willebrand's disease presenting as thrombocytopenia during
pregnancy. Br J Haematol. 1987; 67: 349-53.
http://dx.doi.org/10.1111/j.1365-2141.1987.tb02356.x
PMid:3500738

- Rick ME, Williams SB, Sacher RA, McKeown
LP. Thrombocytopenia asscociated with pregnancy in a patient with type
IIB von Willebrand's disease. Blood 1987; 69: 786-9. PMid:3028536

- Federici AB, Mannucci PM, Castaman G,
Baronciani L, Bucciarelli P, Canciani MT, Pecci A, Lenting PJ, De Groot
PG. Clinical and molecular predictors of thrombocytopenia and risk of
bleeding in patients with von Willebrand disease type 2B: a cohort
study of 67 patients. Blood 2009; 113: 526-34.
http://dx.doi.org/10.1182/blood-2008-04-152280
PMid:18805962

- Federici AB, Mazurier C, Berntorp E, Lee
CA, Scharrer I, Goudemand J, et al. Biologic response to desmopressin
in patients with severe type 1 and type 2 von Willebrand disease:
results of a multicenter European study. Blood 2004; 103: 2032-8.
http://dx.doi.org/10.1182/blood-2003-06-2072 PMid:14630825

- Castaman G, Bertoncello K, Bernardi M,
Rodeghiero F. Pregnancy and delivery in patients with homozygous or
heterozygous R854Q 2N VWD. J Thromb Haemost 2005; 3: 391-2.
http://dx.doi.org/10.1111/j.1538-7836.2005.01162.x
PMid:15670054

- Castaman G, Lethagen S, Federici AB,
Tosetto A, Goodeve A, Budde U, et al. Response to desmopressin is
influenced by the genotype and phenotype in type 1 von Willebrand
disease (VWD): results from the European Study MCMDM-1VWD. Blood 2008;
111: 3531-9. http://dx.doi.org/10.1182/blood-2007-08-109231
PMid:18230755

- Mannucci PM. Treatment of von Willebrand's
Disease. N Engl J Med 2004; 351: 683-94.
http://dx.doi.org/10.1056/NEJMra040403 PMid:15306670

- Rodeghiero F, Castaman G, Tosetto A. How I
treat von Willebrand disease. Blood 2009; 114: 1158-65.
http://dx.doi.org/10.1182/blood-2009-01-153296
PMid:19474451

- Sánchez-Luceros A, Meschengieser SS, Turdó
K, Arizó A, Woods AI, Casais P, et al. Evaluation of the clinical
safety of desmopressin during pregnancy in women with a low plasmatic
von Willebrand factor level and bleeding history. Thromb Res 2007; 120:
387-90. http://dx.doi.org/10.1016/j.thromres.2006.09.004
PMid:17056101

- Mannucci PM. Use of desmopressin (DDAVP)
during early pregnancy in factor VIII-deficient women. Blood 2005; 105:
3382. http://dx.doi.org/10.1182/blood-2004-11-4472 PMid:15802549

- Mathew P, Greist A, Maahs JA, et al. Type
2B vWD: the variable clinical manifestations in two kindreds.
Haemophilia 2003; 9: 137-44.
http://dx.doi.org/10.1046/j.1365-2516.2003.00712.x
PMid:12558793
