Received: April 28, 2014
Accepted: May 16, 2014
Meditterr J Hematol Infect Dis 2014, 6(1): e2014041, DOI 10.4084/MJHID.2014.041
This article is available on PDF format at:

Francesca Rinaldi1*, Raffaella Lissandrin1*, Francesco Mojoli2, Fausto Baldanti3, Enrico Brunetti1, Michela Pascarella4 and Maria Teresa Giordani5
1
Department of
Infectious Diseases, IRCCS San Matteo Hospital Foundation, University
of Pavia, Viale Golgi 19, 27100 Pavia, Italy.
2 Clinical-Surgical, Diagnostic and Pediatric
Sciences
Department, Section of Anesthesia and Intensive Care 1, University of
Pavia, IRCCS San Matteo Hospital Foundation, Viale Golgi 19, 27100
Pavia, Italy.
3 Molecular Virology Unit, Virology and
Microbiology
Department, IRCCS San Matteo Hospital Foundation, Viale Golgi 19, 27100
Pavia, Italy.
4 Microbiology Service, San Bortolo Hospital,
Viale
Rodolfi 37, 36100 Vicenza, Italy.
5 Infectious and Tropical Diseases Unit, San
Bortolo
Hospital, Viale Rodolfi 37, 36100Vicenza, Italy.
* These authors contributed equally to the work

|
This
is an Open Access article distributed
under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract Acute
Human Cytomegalovirus
(HCMV) infection is an unusual cause of venous thromboembolism, a
potentially life-threatening condition. Thrombus formation can occur at
the onset of the disease or later during the recovery and may also
occur in the absence of acute HCMV hepatitis. It is likely due to both
vascular endothelium damage caused by HCMV and impairment of the
clotting balance caused by the virus itself. Here we report on two
immunocompetent women with splanchnic thrombosis that occurred during
the course of acute HCMV infection. Although the prevalence of venous
thrombosis in patients with acute HCMV infection is unknown, physicians
should be aware of its occurrence, particularly in immunocompetent
patients presenting with fever and unexplained abdominal pain.
|
Introduction
Acute portal vein thrombosis (PVT) is
clinically
relevant condition usually associated with bowel ischemia caused by the
involvement of superior mesenteric and splenic veins. In the general
population, the prevalence of PVT is about 1% but can reach 16-40% in
patients with cirrhosis or cancer.[1]
In more than 70%
of cases, PVT is associated with local factors, such as cirrhosis,
malignancy, intra-abdominal infection, abdominal surgery, trauma or
liver transplantation. Moreover, up to 72% of presumed idiopathic PVT
may be associated with thrombophilic conditions and hematologic
diseases.[2] PVT has been described
in patients with
acute hepatitis caused by EBV, HAV, HBV, HCV, but it has been more
often associated with acute HCMV hepatitis.[3]
In this
report, we describe two cases of acute PVT associated with an HCMV
acute infection in two adult immunocompetent women.
Case One
A 62-year-old female was admitted to San Bortolo Hospital, Vicenza,
Italy, in September 2011, with fever and abdominal pain lasting for
several weeks. The patient’s and family history were unremarkable.
Physical examination revealed only slight discomfort on palpation of
the epigastric area. Liver and spleen were regular in size.
White blood count (WBC) was 11.7 x103/μL,
60% lymphocytes, and liver
function tests (LFT) were abnormal (AST 333 IU/mL, ALT 433 IU/mL
[normal value <37], GGT 296 IU/mL [n.v. <33], alkaline
phosphatase (ALP) 221 IU/L [normal range 30-105], bilirubin 1.0 mg/dL
[n.v. <1.3]), some inflammatory indices were raised (C-reactive
Protein 3.65 mg/L [n.r 0.00-0.50], ferritin 1442 ng/mL [n.r. 10-160 ],
lactate dehydrogenase 1098 U/L [n.r. 200-420], creatine phosphokinase
24 U/L [n.r. <200] procalcitonin 0.54 ng/mL [n.v.<0.5],
with
normal erythrocyte sedimentation rate (ESR) 27 mm/h [n.r. 2-45]).
Chest X-Ray was negative. An abdominal ultrasound (US) (Aplio XG Model
SSA-790A, Toshiba, Tokyo, Japan), showed a complete thrombosis of the
left portal branch, confirmed by a contrast-enhanced ultrasound
(SonoVue, Bracco, the Netherlands) and a computed tomography (CT) scan
(see Figure 1,
Panel 1a).
No other lesions were
found in the abdomen. A hematologic evaluation ruled out
myeloproliferative and lymphoproliferative disorders; although a
bone-marrow biopsy was not considered, an immune-phenotypic analysis of
the peripheral white blood cells and red blood cells resulted
in
normal range and did not find cellular clones with GPI-linked molecules
deficit (in order to exclude paroxysmal nocturnal hemoglobinuria).
Inherited and acquired risk factors for thrombosis were ruled out (see Table 1). The
patient was a mild
smoker (5 cigarettes/day) and was not on hormones; neoplastic markers
(Carcinoembryonic [CEA] and carbohydrate antigen [Ca]19.9 and 15.3,
alpha-fetoprotein [AFP]) were all negative. Antibodies against the main
hepatotropic viruses (HAV, HBV, HCV, HEV) were negative while HCMV
serology suggested primary infection (IgM 10.86 mg/dL [negative
<1],
IgG 12.8 mg/dL [negative<11]). HCMV DNA (real-time PCR, Real
Time
Alert QPCR, Elitech Group Nanogen, Milan, Italy) was positive at 3434
copies/ml (sensitivity cut-off: >1111). Thus, acute HCMV
hepatitis
complicated with portal vein thrombosis was hypothesized.
The patient was treated with i.v. gancyclovir (5 mg/Kg/bid) and low
molecular weight heparin (sodium enoxaparin 4.000 U.I. bid) for 15
days. On discharge, HCMV DNA was undetectable. An abdominal US
performed before discharge showed thrombus organization (retraction and
hyperechoic clot) (see Figure
1, Panels
1b and 1c). The
patient continued oral anticoagulant treatment (Warfarin 5 mg/day with
INR check every 2-3 days in the first two weeks) for 21 months after
discharge until her abdominal US showed an almost complete
re-canalization of the left portal branch. A prolonged follow-up (40
months) including clinical interview, abdominal ultrasound, blood and
LFT resulted normal.
Case Two
A 20-year-old Caucasian woman was admitted to Maggiore Hospital in
Crema, Italy, in November 2011, for gastric pain and headache lasting
three days. A US scan of the upper abdomen (Esaote myLab25, Esaote,
Genova, Italy) showed portal thrombosis of the intra-hepatic right and
left branches, splenomegaly and free fluid in the perihepatic area and
in the Douglas pouch. Chest X-Ray was negative. Biochemical examination
revealed abnormal liver function tests: (AST 162 IU/ml, ALT 243 IU/mL,
GGT 167 IU/mL, ALP 402 IU/L) and increased inflammatory indices
(Lactate dehydrogenase 747 U/L, C-reactive Protein 1.5 mg/L); ESR was
normal at 23 mm/h.
The patient received anticoagulant therapy (continuous infusion of
unfractionated heparin, 18 UI/Kg/h). An abdominal CT confirmed portal
thrombosis involving the left and the right intra-hepatic branches and
the superior and inferior mesenteric veins. A 3 cm long thrombus was
identified at the beginning of the splenic vein, which was still
patent. The patient was transferred to the Intensive Care (ICU) of San
Matteo Hospital, Pavia, Unit where blood tests confirmed abnormal liver
enzymes with normal white blood cells (WBC: 4100/mm3, 63% of
lymphocytes). At ICU admission, a new CT scan confirmed the thrombosis
(see Figure 1,
Panel 1d)
and showed also
pericardial and bilateral pleural effusions.
Thrombophilic conditions were ruled out by specific tests (see Table 1). The
patient did not smoke
and was not on hormones.
Lymphocyte immunophenotyping was consistent with acute viral illness
(CD4/CD8 0.5, CD4: 31.1%, CD8: 57.8%). Serology revealed acute HCMV
infection: IgM anti CMV (ELISA): 11.8 (negative < 0.9, positive
>
1.1), IgG avidity test (ELISA): 18%, (low < 35, high
>50). HCMV
DNA (real-time PCR) was positive 100 copies/ml (cut-off >100
copies). Serology for HIV, HCV, HBV, S.typhi, Yersinia spp, Hantavirus,
Listeria spp, Leptospira spp, Borrelia spp and HSV-8 were negative.
Neoplastic markers (CEA, Ca 19.9 and Ca15.3, AFP) were all negative.
She was treated with anticoagulants (unfractionated heparin followed by
enoxaparin 100 UI/Kg), with progressive regression of the thrombosis
and disappearance of the fluid collections. A US scan one month after
discharge showed further regression of PVT.
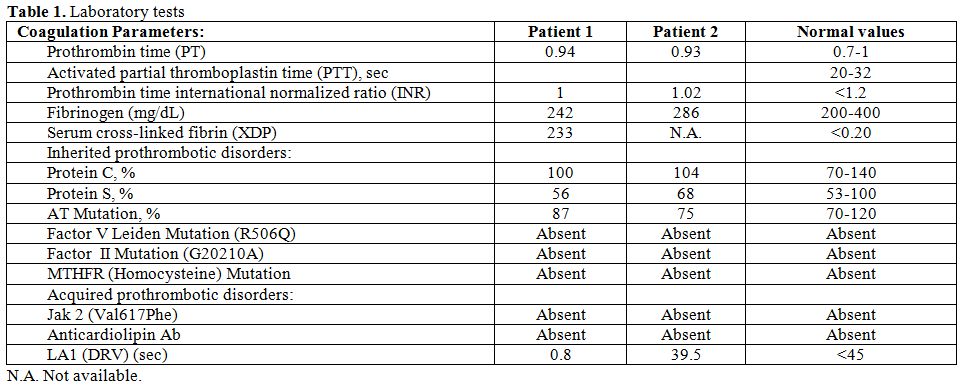 | Table 1. Laboratory tests |
Discussion
Although HCMV infection is very common, up to 40% of adult
immunocompetent subjects are seronegative for HCMV. The prevalence of
HCMV infection is underestimated, since it occurs in childhood when it
is usually asymptomatic. In the adult it is frequently characterized by
fever, swollen neck lymph nodes and mild hepatitis, spleen enlargement
and low platelet count. The true rate of symptomatic disease is,
however, unknown. The diagnosis is commonly made by serology (IgM
anti-CMV positivity and rising title of IgG anti-CMV).
HCMV reactivation is commonly seen in immunocompromised individuals
such as transplant and AIDS patients, leukemia and lymphomas, or in
situations such as prolonged steroids administration for rheumatologic
and autoimmune diseases. Portal thrombosis is an uncommon but not so
rare event occurring during acute HCMV infection and has been recently
sporadically documented.[4,5]
Atzmony and Abgueguen in
2010 reported a prevalence of thrombosis among hospitalized patients
with acute HCMV infection of about 6.4% and 7.9% respectively, while
Justo et al. reported a 1.9-9.1% incidence of HCMV infection in
patients with thrombotic events.[6,7,4]
HCMV-related thrombosis can occur also several weeks after the
diagnosis of acute HCMV.[7]
Unlike other HCMV lesions, which differ in immunocompetent and
immunocompromised patients, deep venous thrombosis seems to occur in
both categories of patients,[8] but
with different
localization. Justo et al. in 2011 showed how immunocompetent patients
experienced more splanchnic vein thrombosis while HIV immunocompromised
ones are more susceptible to deep vein thrombosis and pulmonary
embolism during highly active antiretroviral treatment (HAART).[4]
Several mechanisms have been proposed to explain HCMV-induced vascular
thrombosis, including a direct action by HCMV itself and the activation
of different molecules. HCMV could directly invade the endothelial
cells, causing endothelial damage and the activation of coagulation
factors.[9] It could also
facilitate thrombin
production and interrupt the synthesis of prostaglandin and
interleukin-2 due to procoagulant phospholipids on its surface. Both
these mechanisms cause platelet adhesion.[9]
HCMV, like other viruses and bacteria, seem to induce the production of
anti-phospholipid antibodies[10]
and can inhibit
P53-mediated apoptosis through the activation of its first gene
transcribed, IE84, which binds P53 and inhibits its transcriptional
activity.[7]
Predisposition to thrombosis can be linked to different clinical
situations, such as the use of oral contraceptives, surgery, pregnancy,
active malignancy (directly or as part of paraneoplastic syndrome), and
protracted immobility.[4,11] All
these factors seem to be prevalent in immunocompetent patients.[4] In hematological disorders, causes of
vein thrombosis
are transient or permanent antiphospholipid syndrome, factor V Leiden
heterozygote mutation, protein C or protein S deficiency. In a recent
literature review, chronic myeloproliferative neoplasms (MPN) are
associated in 6-33% of patients with portal vein thrombosis.[2] In the review, the JAK2 V617F somatic
mutation was
reported both in overt and non-overt MPN.[2]
Coagulation factors defects and myeloproliferative disorders, including
JAK2 V617F somatic mutation had been ruled out in both cases (see Table 1).
The clinical manifestations of acute portal vein thrombosis (PVT)
depend on the extent of the obstruction and the speed of its
development. The consequences of an untreated PVT depend on the same
factors: if portal flow is suddenly interrupted (as happens in
experimental thrombosis) a liver infarction or an ischemia of the bowel
may follow.
Even incomplete thrombosis can alter intestinal permeability and lead
to bacterial sepsis, enteric bleeding or diarrhea. In the absence of
treatment, thrombus organization can lead to chronic thrombosis and
portal cavernoma.
When PVT occurs, anticoagulation therapy for at least 3 months is
recommended, starting with low molecular weight heparin in order to
achieve rapid anticoagulation and shifting to oral anticoagulation as
soon as the patient’s condition has stabilized. Long-term
anticoagulation therapy in patients with acute PVT and permanent
thrombotic risk factors that are not otherwise correctable is
recommended.[11]
Antiviral treatment is mandatory in immunocompromised patients, while
its administration in immunocompetent patients is debatable. In case
one, HCMV-DNA tested positive, and the clinician decided to treat the
patient with gancyclovir. Moreover, the initial suspicion of an
associate neoplasm or a hematological malignance played a role in this
decision. In case two the viremia was borderline due to the immune
system control, so in spite of the more aggressive presentation, virus
infection was left untreated.
Finally, bedside US (or “point of care US”) may prove to be a
life-saving approach in emergency settings; a protocol finalized to
achieve a prompt diagnosis of the thrombotic events can be easily
learned by physicians with no previous experience in US.[12]
In our experience, bedside abdominal US can help recognize portal vein
thrombosis due to infectious agents like HCMV and avoid its dangerous
consequences.
Conclusions
Physicians should consider hematologic, neoplastic and infectious etiologies in the workup of patients with fever and PVT. Although venous thrombosis during acute HCMV infection is uncommon in immunocompetent patients, physicians should maintain a high index of suspicion, and testing for HCMV IgM in these cases is recommended.
Acknowledgments
We thank Sam Goblirsch, MD, for reviewing the manuscript and Dr. Carlo Scolarin, MD, for providing patient informations.
References












[TOP]