Received: March 25, 2014
Accepted: June 9, 2014
Meditterr J Hematol Infect Dis 2014, 6(1): e2014046, DOI 10.4084/MJHID.2014.046
This article is available on PDF format at:

Sanjeev Kumar Sharma, Dharma Choudhary, Nitin Gupta, Mayank Dhamija, Vipin Khandelwal, Gaurav Kharya, Anil Handoo, Rasika Setia and Arpita Arora
1Department
of Hemato-oncology and Bone marrow transplantation. BLK Superspeciality
Hospital, Pusa Road, New Delhi, India.

|
This
is an Open Access article distributed
under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract Hematopoietic
stem cell transplantation (HSCT) is a definite cure for many
hematological diseases. With the increasing indications for HSCT and
its relatively low cost in Indian subcontinent, an increasing number of
patients are opting for this procedure. We retrospectively analyzed the
cost of one hundred sixty two HSCTs done at our center in the last
three years. The median cost of autologous transplant was USD, $ 12,500
(range $ 10,331-39,367) and the median cost of allogeneic transplant
was $ 17,914 (range $ 10,832-44,701). The cost of HSCT is cheaper here
compared to that in developed countries and success rates are nearly
equivalent. The major factors contributing to the cost are related to
the complications post-transplant mainly infections and graft versus
host disease, which are also the reasons for the increased stay in the
hospital.
|
Introduction
One
fifth of the world population resides in India. The burden of
hematological diseases both malignant and non-malignant is huge in the
country. About 10,000 children are born with thalassemia major each
year, and about 6,000 cases are diagnosed with aplastic anemia per
year.[1,2] The number of leukemia
and lymphoma patients is about 100,000.[3]
The number of patients requiring bone marrow transplant is also
increasing. With the increasing awareness about hematological diseases
and rising economy, many patients are opting for bone marrow transplant
as a definite treatment for many curable hematological diseases. We
retrospectively evaluated the cost of HSCT in our country and compared
it with data from developed countries.
Materials and Methods
Study
population.
Between January 2011 and September 2013, a total of 162 patients with
hematological diseases received HSCT at the Bone marrow transplant
(BMT) center, BLK Superspeciality Hospital, New Delhi. The study
included patients with thalassemia major, leukemia, lymphoma, aplastic
anemia, multiple myeloma and others. Written informed consent for HSCT
was provided by patients after a discussion of the risks and benefits
of each method with the patient. The total cost included the cost of
chemotherapy, stem cell/bone marrow harvest, antibiotic usage,
supportive care with blood, platelet transfusion and growth factors,
the hospital stay charges, the investigation charges and consultation
fees. The data was obtained from computerized hospital information
system. All patients were treated in Hepa-filtered BMT rooms in the 12
bedded BMT unit. Patients who expired before engraftment were excluded.
The cost of outpatient follow-up or subsequent admissions was also
excluded. The study also excluded the cost of procurement of matched
unrelated donor harvest charges and the cost of HLA typing and donor
assessment. Peripheral blood stem cell harvest was done in the blood
bank by trained apheresis team; bone marrow harvest was done in the
operation theater under general anesthesia. Transplant program employed
a primary transplant team which conducted and monitored all
pre-transplantation and post-transplantation care, supported by medical
and pediatric intensivists. The study was approved by the Institutional
Review Board and hospital’s Ethical committee.
Conditioning
regimen, GVHD prophylaxis, and supportive care.
Conditioning before HSCT consisted of high-dose chemotherapy or reduced
conditioning regimens with or without antithymocyte globulin. The
commonly used regimens were busulfan/cyclophosphamide,
fludarabine/cyclophosphamide/anti-thymocyte globulin,
fludarabine/melphalan, thiotepa/triosulphan/fludarabine, melphalan and
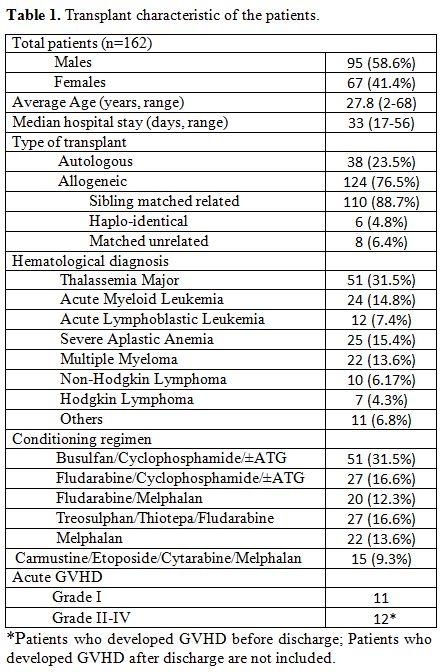
carmustine/etoposide/cytarabine/melphalan (Table 1).
Conditioning regimen, graft source and graft versus host disease (GvHD)
prophylaxis were protocol driven or based on the recommendation of the
transplant team. The day of stem cell infusion was designated as day 0.
For thalassemia major bone marrow was the source of stem cells and for
leukemia and aplastic anemia, granulocyte colony stimulating factor
(G-CSF)-mobilized peripheral blood stem cell from allogenic donor was
the source of stem cells. For myeloma and lymphoma patients autologous
stem cell harvest was done after G-CSF mobilization. Patients received
standard anti-viral prophylaxis with acyclovir and Pneumocystis
jiroveci prophylaxis with trimethoprim-sulfamethoxazole. Levofloxacin
was used as bacterial prophylaxis if specified by protocols. Patients
were treated with broad spectrum antibiotics at the time of their first
neutropenic fever, and with antifungal agents as per institutional
policy.
 | Table 1. Cost of autologous and allogeneic bone marrow transplantation. |
Results
A total of 162 consecutive patients were evaluated for the cost of the procedure, focusing on the inpatient costs, till discharge from the hospital (Table 1). The median total cost of bone marrow transplantation was $ 16,650 (range $ 10,331-44,701). The median days of stay in the hospital were 33 days (range 17-56) (Table 2). Seven patients expired before engraftment and were excluded. The cost of management of acute gut GvHD grade II-IV was $ 11,600-25,500 extra. This cost study excluded the cost for treatment in those patients who developed GvHD after discharge from hospital and required readmission for GvHD treatment. Table 3 shows the distribution of the cost of stem cell transplantation.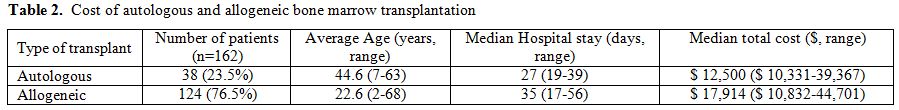 | Table 2. Cost of autologous and allogeneic bone marrow transplantation. |
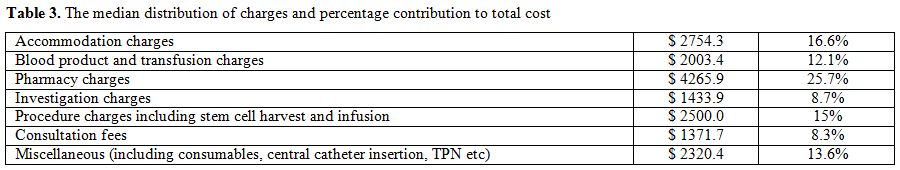 | Table 3. The median distribution of charges and percentage contribution to total cost. |
Discussion
HSCT is the cure for many hematological and non-hematological diseases;
and in developing countries, where socio-economic status is a major
limiting factor, the cost factor associated with BMT is an important
issue. We retrospectively analyzed the costs of bone marrow
transplantation in 162 consecutive patients transplanted in a tertiary
care centre in northern India. The period of cost calculation was from
the day of admission to the hospital for transplantation to the day of
discharge. The median stay was 33 days (range 17-56 days). The median
cost of autologous transplant was $ 12,500 (range $ 10,331-39,367) and
the median cost of allogeneic transplant was $ 17,914 (range $
10,832-44,701). The major cost was of the drugs (chemotherapeutic drugs
and antimicrobials) and the blood products.
We also compared the cost of bone marrow transplants (BMT) done at our
center with the cost of BMT in developed countries. Because of wide
variations in the conditioning protocols and GVHD prophylaxis used,
differences in supportive care practices, physician’s discretion in
using the available resources and the different time periods of
treatment follow-up, included in various studies, the cost factors are
difficult to be compared. Still, when compared to the cost of the
transplant in Europe and USA where it ranges from $30,000 to $88,000
for a single autologous transplantation to $200,000 or more for a
matched unrelated myeloablative allogeneic procedure,[4-7]
the cost of the transplant in developing countries is much lower.[2,8]
In spite of this, many patients are not able to afford this due to low
socio-economic condition in developing countries and lack of sufficient
insurance companies and governmental support.
Cost of transplant also varies with the type of transplant (autologous,
allogeneic), source of graft (sibling or matched unrelated), intensity
of conditioning regimens used etc.[4,10-12] No correlation has been found in
the cost of transplant and patient’s age and sex, disease risk, or
status.[5,9]
The cost of transplantation increases with the number of complications
and duration of stay in the hospital.[5,7,12]
Cost of transplant increases in patients who develop grade III-IV acute
GvHD,[4,6,7]
our patients who developed grade III-IV acute gut GvHD refractory to
first line treatment had 2-3 times higher cost of the transplant.
The variation in the cost of the transplant is also directly related to
the complications post transplant. These are a) infections (bacterial,
fungal and viral), b) requirement of blood product transfusions,
particularly because of the delay in platelet engraftment- requiring
irradiated single donor platelets, c) Intensive care- patients
requiring admission in medical intensive care units or ventilator
support, d) onset of severe acute GvHD. Also, various infective and
non-infective complications can develop later on, following the
discharge from the hospital, and can increase the total cost of stem
cell transplantation.[13-15]
In developing countries, the advantage of opting for transplant in
patients with thalassemia major seems beneficial and much more cost
effective than lifelong transfusion, chelation and investigation cost,[2,15,16]
with nearly equal success rates. Even in acute lymphoblastic leukemia,
allogeneic transplant in CR-1 has been found to be cost effective
compared to chemotherapy.[17] The
patients who
deserve transplant should be considered for transplant early in the
disease course to make it cost effective, particularly in developing
countries, where mostly the cost is borne by the patients themselves,
unlike in developed countries where the government or the insurance
companies support.
The weakness of our study is that we have analyzed the cost of
transplantation from the period of admission for transplantation till
discharge after engraftment. The cost of successive admissions and the
cost of GvHD prophylaxis and anti-microbial prophylaxis and the cost of
regular out-patient follow-up and investigations were not included in
the study. Moreover, the cost effectiveness was also not analyzed.
Conclusion
The cost of bone marrow transplant till engraftment is much lesser in
developing countries compared to developed countries with nearly equal
success rate. In spite of this, many patients are not able to afford a
much needed life saving procedure because of poor financial support.
Further interventions to reduce the cost of the transplant to make it
more affordable to the general population needs to be searched,
considering the growing burden of patients with hematological diseases.
Acknowledgement
We are thankful to Bharti Sharma for collecting and compiling the
transplant data. We are also thankful to Dr Sandeep Kumar Sharma and
Aashna Sharma for formatting the manuscript.
References

















[TOP]