Received: March 26, 2014
Accepted: June 10, 2014
Meditterr J Hematol Infect Dis 2014, 6(1): e2014049, DOI 10.4084/MJHID.2014.049
This article is available on PDF format at:

Fina Vieira1, Mamadu Saliu Sanha1,2, Fabio Riccardi2,3 and Raffaella Colombatti2,4
1
Hospital Raoul Follereau, Bissau, Guinea Bissau.
2 Aid, Health and Development-Onlus.
3 Department of Biomedicine and Prevention,
University of Tor Vergata, Rome, Italy.
4 Clinic of Pediatric Hematology-Oncology,
Department
of Maternal and Child Health, Azienda Ospedaliera-University of Padova,
Padova, Italy.

|
This
is an Open Access article distributed
under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract Background:
Tuberculosis (TB) is widespread in Africa, but weak health systems in
developing countries, often display poor quality of care with delays in
case identification, irrational therapy and drug shortage, clinical
mismanagement, unnecessary expenditures for patients, reduced adherence
and increased mortality. Public-private partnership has demonstrated to
increase TB case detection, but less is known about its effects on
quality of care, mortality and costs for hospitalized TB patients.
Methods: Clinical outcomes and costs for TB patients at the TB National Reference Center of Bissau, in Guinea Bissau, West Africa, were determined during the first 5 months of the public-private management and compared to the ones of previous years when the hospitals was under direct Government’s management. Results: 215 (2009-2010) and 194 (2012-2013) patients were admitted, respectively. Improvement (p<0.05) was observed in mortality reduction (21% vs 6%), cause of death determination (50% vs 85%), treatment abandonment (15 vs 1). Direct costs for patients during TB diagnostic pathway and inpatient care were significantly reduced, 475 vs. 0 USD. Conclusions: Public-private partnerships displays significant short term benefits in National TB reference centers, even in post-conflict countries. Further studies could aid in determining the overall long term benefits of this type of cooperation, and the specific characteristic of TB and concomitant hematologic and infectious diseases in TB admitted patients. |
Introduction
Tuberculosis (TB) treatment has saved
more than 2 million people since 1995.[1]
Nevertheless, too many are not diagnosed, not treated or not properly
treated. Public-private partnership has increased Tuberculosis (TB)
case detection in different contexts.[2-3]
Weak health systems in developing countries, often display poor quality
of care, delays in case identification, irrational therapy and drug
shortage, unnecessary expenditures for patients and increased
mortality.[2,3] Despite a policy of
free drug
treatment, TB health services in many countries charge all income
groups, costs are high and adherence measures are inadequate.[4-5] Patients’ costs can be particularly
burdensome for TB affected households in Africa.[6]
Guinea-Bissau, in West Africa, has been experiencing annual military
coups since the 1999 civil war. The country's health indicators are
among the worst in Africa.[7]
Proportion of budget
spent on health is 2% of GDP, with total dependence on external
financial support to the budget of the Health Ministry. The payment of
salaries to health workers has often been subject to delay, and morale
is poor.[7]
TB incidence is 242/100.000.[1]
Case detection rate
for all forms of TB, at 48%, has been declining since it reached 81% in
1995, indicating a decline in programmatic performance.[1,7] The treatment success rate, for
smear-positive TB (60%) and other forms (about 55%) is low.[1]
The TB National Program operates through the National Reference Center
in Bissau, Hospital Raoul Follereau (HRF), Regional Hospitals in the
Regions and TB Health Centers throughout the country. According to the
National Guidelines, TB patients in poor clinical conditions or with
severe disease are admitted to the HRF, after referral from regional
hospitals or health centers.[8]
The National Reference Center for Tuberculosis and Lung Diseases, HRF,
is an 115 bed hospital which includes an in-patient service (three
words: men, women and children), an outpatient service, laboratory, two
X-Ray Units, a pharmacy, service area (kitchen, laundry, ironing) and
two cafeterias. Since October 1st
2012
the Health Ministry has entrusted the management of the HRF to the
International Organization, Aid, Health and Development (AHEAD). The
Government would give TB drugs received from international donors, pay
the staff salaries and provide electricity. AHEAD would supply a top-up
for the personnel and the diagnostic and treatment pathway for free to
inpatients (including exams, non-specific drugs, food). The public
hospital would be managed by the private sector, but within the
framework of the National TB Program. It was hoped that this
public-private partnership would improve the quality of diagnosis and
treatment of TB suspects, increase adherence while reducing mortality
and costs.
Materials and Methods
Methods
According to the National Guidelines,[8]
as part of
routine clinical diagnostic evaluation, patients who are admitted to
the HRF with a suspect of TB, received a three sample sputum analysis
and a thorax X-Ray. Ziehl-Neelsen’s sputum staining technique is used,
and patients are considered smear positive if acid fast bacilli are
shown on at least two samples. Sputum Culture and PCR are not available
in the country for the present being. Smear negative patients are
considered to have TB according to the physician’s evaluation of chest
X-Ray and clinical condition. Additional analyses (complete blood
count, biochemistry, urine and stool evaluation and culture) are
performed if necessary, based on physician’s judgment. TB is treated
according to the National Guidelines,[8]
with a four
drug regimen for two months (rifampicin, isoniazid, ethambutol and
pyrazinamide) followed by two drugs for the following six months
(isoniazid and ethambutol); five drugs are used in case of relapsed TB
(streptomycin, rifampicin, isoniazid, ethambutol and pyrazinamide).
We evaluated all-cause mortality rates, adherence to the
hospitalization phase of TB treatment, diagnostic procedures and direct
costs for inpatients in the first 5 months of the public-private
management (October 1st
2012-February 28th
2013); furthermore, we compared them to the five months of the same
season in previous years (October 1st
2009-February 28th
2010), when complete data were available. Data on TB co-infections or
hematologic malignancies and severity score were seldom available and
not routinely utilized to grade and classify patients in both periods
and therefore could not be compared. No user fees were applied during
the public-private management while user fees were applied during
previous years under the Government direct management of the hospital
both during the diagnostic pathway and for admission. Patients’
clinical cards and hospital registries were used to cross-check
diagnosis, therapy and admission-discharge dates. Pearson's chi-square
test was used to compare variables within groups. p-values<0.05
were
considered statistically significant.
Materials and Methods
Results
The majority of patients came from Bissau (82% in 2009 and 71% in
2012); there was a slight increase in patients coming from outside the
capital in 2012 (29 % vs 18%).
No treatment abandonment was observed in the two periods, but 15 drop
outs were registered between January 2009 and May 2012 - when user fees
were applied - and only 1 between June 2012 and May 2013 - when
treatment was free.
The clinical characteristics of admitted inpatients are detailed in Table 1.
A significant reduction in mortality (21 vs 6%) was observed in October
2012-February 2013, both during the first week of admission and
afterwards (Table 1 and
Table 2).
Within the population of patients who died, the number of diagnostic
exams was significantly different, with improved quality of diagnostic
pathway in October 2012-February 2013 compared to October 2009-February
2010 (Figure 1 A-B).
This allowed a significant increase in the number of patients in which
the cause of death could be determined (Table 2).
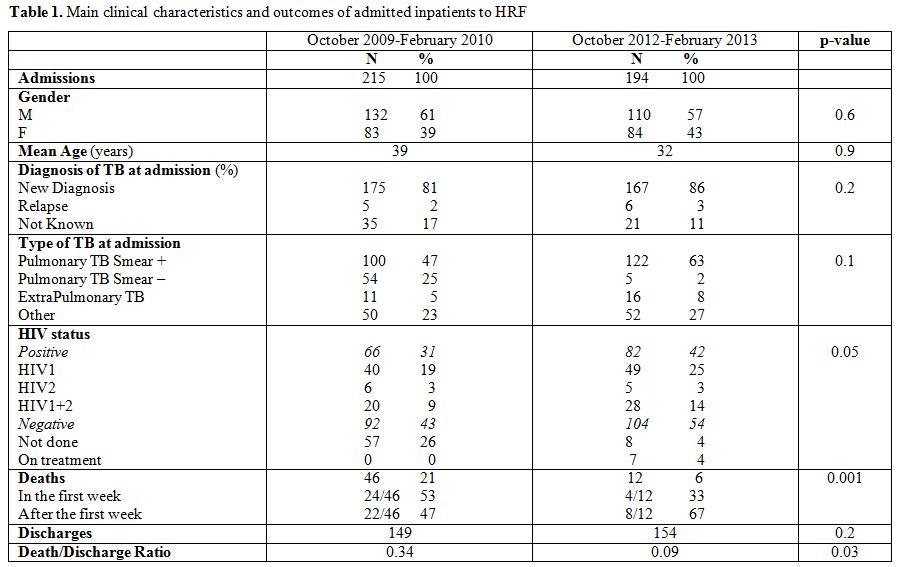 | Table 1. Main clinical characteristics and outcomes of admitted inpatients to HRF. |
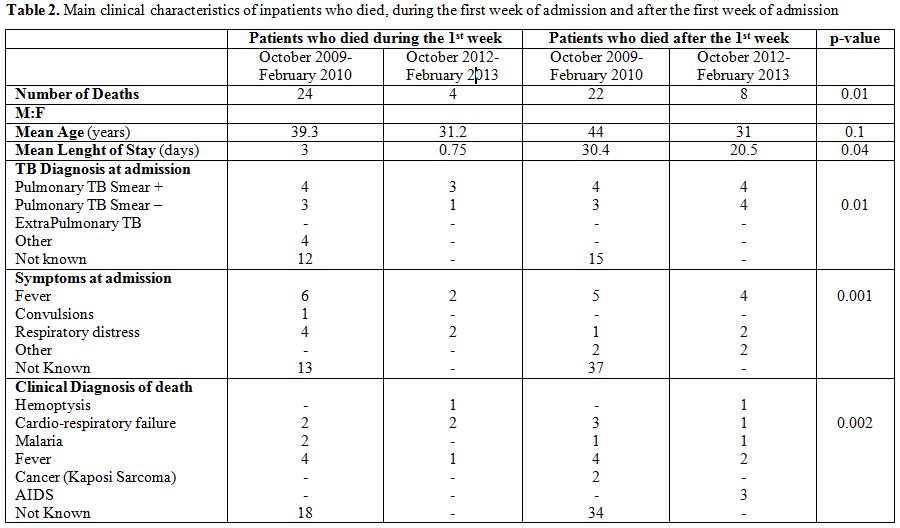 |
Table 2. Main clinical characteristics of inpatients who
died, during the first week of admission and after the first week of
admission. |
The
number and type of available drugs was also different in the two
periods with increased availability of i.v. antibiotics and
antimalarials in 2012-2013 compared to 2009-2010 (1.6 vs 0.2 per
patient).
Direct costs of TB diagnosis (XRays, BK analysis, Laboratory exams) in
October 2009-February 2010 were 31000 CFA per patient (65,11 USD) while
in October 2012-February 2013 they were zero. No direct cost for
hospitalization was required in October 2012-February 2013 while in
October 2009-February 2010 they were estimated in 195000 CFA per
patient (409,5 USD) (bed occupation, food, non specific drugs).
Discussion
Our experience suggests that a public-private partnership within the
framework of the National TB Program in a National Reference Center,
can be successfully implemented in a low resource and post-conflict
country. Even if a six months period is too short to evaluate long term
indicators, significant reductions in mortality and improvements in
diagnosis can already be observed in the short term.
In-hospital mortality for TB patients is multifactorial and remains
high in many countries.[9]
The significant reduction in mortality (21 vs 6%) observed in our
cohort was due to the reduction of mortality both during the first week
of admission and afterwards. Patients, usually admitted in severe
conditions, frequently have disseminated infections or comorbidities.
It is likely that patients have sought care earlier in the course of
the disease, knowing it was free of charge. Moreover, the increased
availability of diagnostic tools, iv antibiotics, antimalarials and
saline solutions might have had an impact in the possibility of
physicians to manage acutely ill patients and therefore contributed to
the mortality reduction both in the first week of admission and
afterwards.[10]
No treatment default was observed since the free hospitalization
regimen was implemented; meaning that lack of will to be cured is not
an issue. TB patients in Africa often default in the hospitalization
phase: hospitalization is problematic due to poor general conditions in
TB hospitals, costs incurred by patients during hospitalisation and
because patients need to earn living or take care of their families.[11]
Stock ruptures, shortage of reagents and drugs and low salaries produce
lack of motivation and poor morale impairing health personnel’s work
and dramatically reducing diagnostic and treatment performances in
Africa. The free care of severely ill TB patients, including drugs and
nutritional support, coupled with top-up for the personnel is likely to
have contributed to eliminate drop outs and reduce mortality after the
first week of admission.
Our short term analysis has several limits. First, we considered all
cause mortality and could not detail TB related mortality, mainly due
to the limited number of diagnostic exams performed in the first
period. It is likely that considering complete blood count and other
laboratory exams on a routine basis will allow a better definition of
other causes of mortality in TB inpatients such as acute anemia,
concomitant infections, hematologic malignancies, etc. Second, the
direct cost that were evaluated included the costs that are necessary
for TB diagnosis and inpatient care and not all the direct cost that
the patients experience, therefore they are probably underestimated and
overall direct costs are likely to be higher in both periods. Third, a
short term evaluation of public private partnership in only five months
does not allow detailing all the benefits and drawbacks of such a
collaboration. Nevertheless, post conflict and low resource countries
such as Guinea-Bissau that do not seem able to find rational and
appropriate ways to come out of isolation and to tackle health
challenges, desperately need positive experiences. We think it’s worth
reporting the improvement obtained in a short period of time of a
public-private international partnership in order to move forward and
enhance TB diagnosis, definition of co-morbidities, treatment and care
in the long term.
Conclusion
The main challenge in fighting the TB epidemics in Sub-Saharian Africa is to improve the sanitary system. Our experience demonstrates that international public-private partnerships in TB hospital settings can contribute, in the short term, to increase adherence to the hospitalization phase of intensive treatment, improve quality of diagnosis and care and reduce mortality through a free pathway of diagnosis and care.[12]
Acknowledgments
The Authors would like to thank the Ministry of Health, the National
Program Against Tuberculosis, the staff of the Hospital Raoul Follereau
and all the patients and their families.
References









[TOP]