Received: January 5, 2016
Accepted: February 22, 2016
Mediterr J Hematol Infect Dis 2016, 8(1): e2016019, DOI 10.4084/MJHID.2016.019
This article is available on PDF format at:


| This is an Open Access article distributed
under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |
|
Abstract Background: Neutropenic
patients are susceptible to any anorectal disease, and symptomatic
anorectal disease afflicts 2-32% of oncology patients. Perianal
infections are the most feared complication, considering the lack of
natural defense against infectious microorganisms. When septic
complications develop, the anorectal disease is potentially fatal,
especially in neutropenic patients in whom mortality rates range
between 11-57%. Although anorectal diseases are a frequent complication
with potentially fatal outcomes among patients with hematologic
diseases, sufficient data are not available in the literature. In this
study, we aimed to investigate the anorectal complications developing
during the neutropenic period in patients with hematologic diseases. Methods: A total of 79 patients whose neutropenic period (absolute neutrophil count <500/mcL) continued for 7 days, or longer were included in the study. Results: A total of 34 patients out of 79 (43%) were detected to develop anorectal complications, of them 6 (7.6%) developed an anorectal infection. The patients were characterized according to the hematological disease and its status (active or not), the type of treatment and the presence of a history of an anorectal pathology before the onset of the hematologic disease. Nineteen (24.1%) patients had the history of anorectal disturbances before diagnosis of the hematologic disease, and recurrence of an anorectal pathology was found in 14 out of 19 patients (73.7%). In addition, the overall mortality rate was higher among the patients who developed anorectal complications compared to another group (41.2% vs. 22.2%, p=0.059). Conclusion: Anorectal pathology is a common complication with high recurrence rate in neutropenic patients. Perianal infections are important as they can cause life-threatening outcomes although they are relatively rare among all anorectal complications. Therefore perianal signs and symptoms should be meticulously evaluated concerning early diagnosis and treatment. |
Introduction
Febrile neutropenia is an important cause of mortality occurring commonly after myelosuppressive treatment in cancer patients.[1,2] Neutropenic patients are susceptible to any anorectal complications,[3] and symptomatic anorectal pathology afflicts 2-32% of oncology patients.[4]
Perianal infections (represented by an abscess or infected fistula) are
the most feared complication, considering the lack of natural defense
against infectious microorganisms.[3] The incidence of perianal infection is approximately 8-9% of patients with acute leukemia.[5]
When septic complications develop, the anorectal disease is potentially
fatal, especially in neutropenic patients, in whom mortality rates
range from 11-57%.[4]
Although anorectal diseases
are a frequent complication with potentially fatal outcomes among
patients with hematologic diseases, sufficient data are not available
in the literature. In this study, we aimed to investigate the anorectal
complications developing during the neutropenic period in patients with
hematologic diseases.
Methods and Patients
This study was conducted as a retrospective, cross-sectional,
single-center investigation. A total of 79 patients, admitted to our
clinic between 01 November 2014 and 01 November 2015, with a diagnosis
of acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL),
myelodysplastic syndrome (MDS), Hodgkin lymphoma (HL), non-Hodgkin
lymphoma (NHL), multiple myeloma (MM) and aplastic anemia (AA), whose
neutropenic period (absolute neutrophil count <500/mcL) continued
for 7 days or longer, were included in the study. Anorectal problems
were defined according to anamnesis, physical examination findings,
gastroenterology and general surgery consultations, and imaging methods
(pelvic computer tomography or magnetic resonance imaging) when
required.
Patients who had a newly diagnosed disease, or
refractory, relapsed and progressive were defined as the ones who had
“an active disease”. Comorbidities included diabetes mellitus,
hypertension, a pulmonary, cardiac, hepatic and renal disease, or a
history of a previous malignancy other than the current one,
Statistical Analysis:
Patient characteristics were examined using descriptive statistics.
Continuous variables were given as mean ± standard deviation (SD), and
categorical variables were defined as a percentage. Chi-square test and
t-test were used to compare proportions and means for categorical and
continuous variables, respectively. Statistical Significance was
defined as p<0.05. All test significances were two-tailed. SPSS
statistical software (SPSS 17.0 for Windows, Inc., Chicago, IL, USA)
was used for all statistical calculations.
Results
The study included 30 (38%) female and 49 (62%) male patients with mean age of 42.9±14.4 years (44.8±15.6 for women and 41.8±13.7 for men). Clinical characteristics of the patients are given in Table 1.
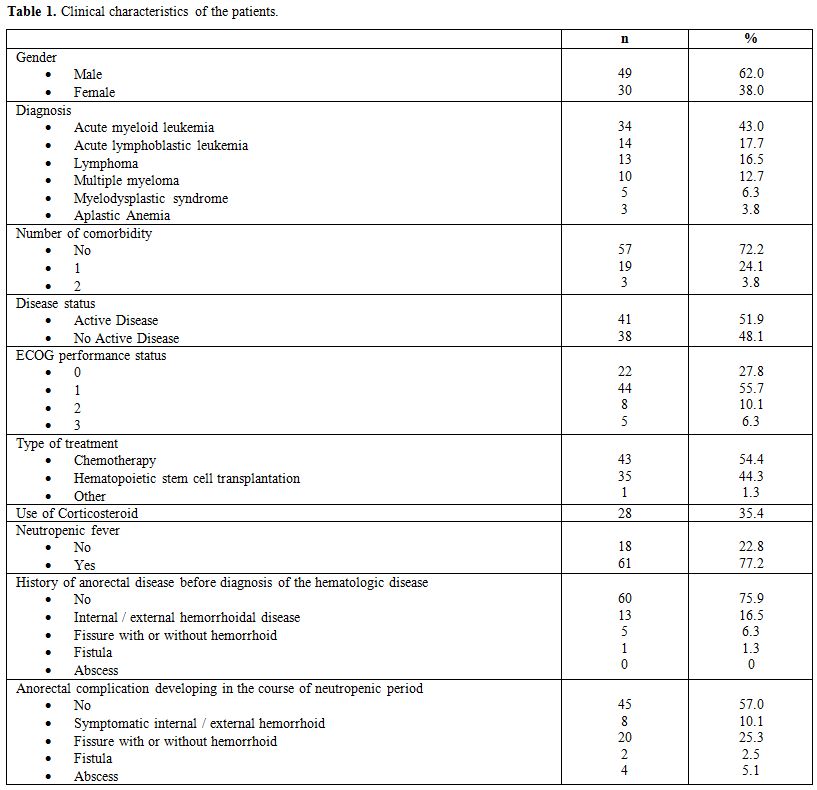 |
Table 1. Clinical characteristics of the patients. |
The mean duration of neutropenia period was found as 14.6 days (range 7-60). A total of 34 patients out of 79 (43%) were detected to develop anorectal complications, of them 6 (7.6%) developed a perianal infection (abscess and fistula). Anorectal complications were observed on average by day 12 (0-28) of neutropenia, and the period of neutropenia lasted an average of 8 days (range 1-60). When the patients were compared regarding anorectal complications, the patients who developed anorectal complication were seen to be older (43.8±14.7 vs. 42.3±14.4 years, p=0.661) and stayed neutropenic for a longer period (16.7±7.5 vs. 13.7±8.2 days, p=0.102) however the difference was not statistically significant for both parameters. Comparison of the groups about anorectal complications development is given in Table 2.
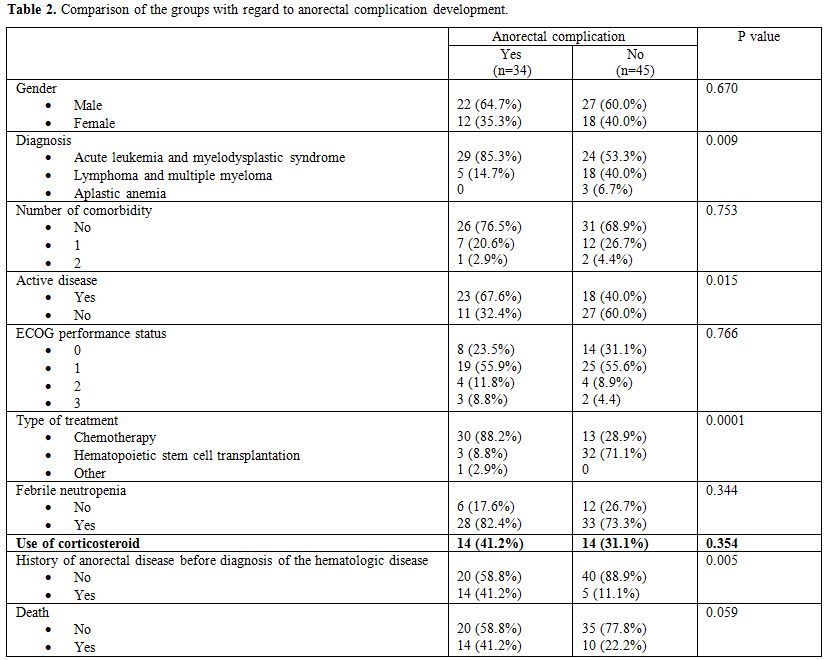 |
Table 2. Comparison of the groups with regard to anorectal complication development. |
Of 6 patients who developed a perianal infection, septic
shock develop in 3, Fournier’s gangrene developed in one, and the
overall mortality rate was 50%. Culture positivity was detected in 2
(33.3%) out of 6 patients, and growing microorganisms were Pseudomonas
aeruginosa and Escherichia coli.
An anorectal complication was
seen to develop in a total of 34 (43%) patients during the neutropenic
period. Nineteen patients ((24.1%) had the history of anorectal
diseases before the diagnosis of the hematologic disease, and a
recurrence of anorectal disease was found in 14 out of 19 patients
(73.7%). Of 60 patients without previous anorectal diseases 20 (33,3%)
suffered from an anorectal complication, and a statistically
significant difference was detected between the two groups (p=0.003).).
The anorectal complication was detected in 29 out of 53 patients
(54.7%) who had acute leukemia and MDS, in 5 out of 23 patients (21.7%)
who had lymphoma and MM, and no anorectal complications developed in AA
patients. Febrile neutropenia ratio was higher among the patients who
developed anorectal complications as expected although the difference
was not significant (82.4% vs. 73.3%, p=0.344).
When the groups
were compared, the disease type (acute leukemia or MDS vs. lymphoma),
the presence of active disease, the kind of treatment and presence of
the history of an anorectal pathology before the diagnosis of the
hematologic disease were influent in determining anorectal disease
development. On the other hand, corticosteroid use was detected not to
be effective on anorectal complication development. A statistically
significant difference was not detected between the groups which
developed and did not develop anorectal complications in steroid use
(41.2% vs. 31.1%, respectively; p=0.354). In addition, the overall
mortality rate was higher among the patients who developed anorectal
complications compared to another group (41.2% vs. 22.2%, p=0.059). In
our study, 14 out of 23 patients (60.9%) who developed anorectal
complications and had an active disease died, however, no deaths
occurred in 11 patients who developed anorectal complications but who
did not have an active disease.
Discussion
Manifestations of perianal infections may differ from those with a competent immune system[3] and are often accompanied by severe pain, swelling, constipation, and may cause systemic infection.[6]
However, the clinical presentation of an anorectal infection is often
masked by the absence of inflammatory cells so recognition of the signs
and symptoms can be difficult in neutropenic patients.[7]
Perianal infections are a life-threatening complication including
Fournier’s gangrene that requires rapid diagnosis and intervention as
recurrence and mortality rates may be expressive.[3,8]
In a series of 92 patients with acute or chronic leukemia, most common
manifestations were a perirectal abscess (27%) followed by anal
fissures (23%), external hemorrhoids (19%) and perianal ulcerations
(13%).[3] Another retrospective study found a perianal infection prevalence of 6.7% and recurrence was diagnosed in 31% of the cases.[3] Grewal et al.[4] reported that 5.8% patients hospitalized with leukemia had the concomitant symptomatic anorectal disease. Büyükaşık et al.[5]
found the incidence of perianal infections in acute leukemia as 7.3
percent. We detected that 43% of the patients developed anorectal
complications, and 7.6% developed a perianal infection (abscess and
fistula), consistently with literature. Recurrence of anorectal disease
was found as 73.7% (14 out of 19 patients) in our study suggesting that
anorectal disease development is a common and recurrent complication
during the neutropenic period. Anorectal complication development rate
was higher among the patients who had an active disease compared to the
patients whose disease was under control (67.6% vs. 40.0, p=0.015).
This finding suggests that anorectal complications can cause severe
morbidity in the presence of an active disease. While overall mortality
rate was found in 41.2% of all patients with anorectal complication,
this proportion increases to 60.9% in the presence of active disease
together. On the other hand, no deaths occurred in 11 patients who had
an anorectal complication but not an active disease. Similarly to our
results, Musa et al.[9] found that the overall
mortality was 53% among 17 adults with hematologic malignancy in whom
anorectal complications developed, the death rate was 69% for those in
whom the disease was not in remission compared with zero for patients
who were in remission. However, these data are insufficient for to say
that anorectal complications increase mortality in patients with active
disease.
In
literature, no consensus is available for the treatment of anorectal
complications in neutropenic patients together with the lack of studies
investigating these complications.[5] Some authors
defended operative treatment, whereas others reported high mortality
rate with operative treatment compared with medical procedures.[5]
Interestingly, internists reported success with surgery or failure with
medical treatment; however, most of the surgeons were unsatisfied with
the surgical approach and concluded that surgical treatment should be
reserved for patients who recovered from neutropenia and active
disease.[5] Grewal et al.[4] did not
observe excessive morbidity or mortality in the operated neutropenic
patients with anorectal disease as compared with the non-operated
patients. Nowadays, the number of patients requiring surgical
intervention decreased substantially, which it was ascribed to the use
of broad-spectrum antibiotics coverage of gram-negative and anaerobic
bacteria.[7] We had a similar clinical approach;
namely, we prefer administration of a broad spectrum antibiotic
effective on gram negative and anaerobic bacteria (usually a carbapenem
antibiotic) when perianal infection develops during the severe
neutropenic period. The surgical approach is considered in the case of
failure of medical treatment or persistence of the perianal infection
even after the restore from neutropenia.
Conclusion
An anorectal pathology is a common complication with high recurrence rate in neutropenic patients. It is a serious cause of morbidity which impairs quality of life particularly in patients with acute leukemia and MDS, who receive intensive chemotherapy and who have an active disease. Perianal infections are important as they can cause life-threatening outcomes although they are relatively rare among all anorectal complications. Therefore perianal signs and symptoms should be meticulously evaluated to do an early diagnosis and treatment.
References









[TOP]