Benedetta Rambaldi1, Domenico Russo1 and Livio Pagano2
1 Cattedra
di Ematologia, Unità di Malattie del Sangue e Trapianto di Midollo
Osseo, Dipartimento di Scienze Cliniche e Sperimentali, Università di
Brescia e ASST Spedali Civili, Brescia, Italy
2 Istituto di Ematologia, Università Cattolica S. Cuore, Roma, Italy
Corresponding
author: Benedetta Rambaldi. Cattedra di Ematologia, Unità di Malattie
del Sangue e Trapianto di Midollo Osseo, Dipartimento di Scienze
Cliniche e Sperimentali, Università di Brescia e ASST Spedali Civili,
Brescia, Italy. E-mail:
detta.rambaldi@hotmail.it
Published: January 1, 2017
Received: November 16, 2016
Accepted: December 11, 2016
Mediterr J Hematol Infect Dis 2017, 9(1): e2017012 DOI
10.4084/MJHID.2017.012
This article is available on PDF format at:

This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
Dear Editor,
Invasive
fungal infections (IFIs) represent an important cause of morbidity and
mortality in patients affected by hematological malignancies (HMs),
particularly those with an immunocompromised status.[1,2]
In this setting, IFIs still represents a major clinical problem also
for the high costs related to the antifungal prophylaxis and treatment.[3,4]
When considering the high clinical heterogeneity of these patients, the
risk of IFIs may be remarkably different. Accordingly, if such a risk
is not appropriately evaluated, the possibility of an overtreatment in
some or an undertreatment in other patients is very likely.Pagano
et al., on behalf of SEIFEM (Sorveglianza Epidemiologica Infezioni
Fungine nelle Emopatie Maligne) group, recently published a systematic
review of the literature on the risk and incidence of IFIs in the
setting of HMs with the aim to consider the main predisposing factors
and to suggest practical strategies for prevention and treatment of
IFIs.[5] In this review, specific IFI predisposing
factors are summarized for each disease class. Depending on the risk of
developing IFIs, patients are then divided into three groups: high,
intermediate, low-risk group. Briefly, patients with acute myeloid
leukemia (AML) or treated with an allogeneic hematopoietic stem cell
transplantation (HSCT) have per se
an increased risk of IFI. Moreover, some conditions predispose a high
risk of IFI, independently of the underlying disease, like neutropenia,
relapse/refractory disease, previous history of IFI, salvage therapy
and a high dose of steroids.To
facilitate the reading of this analysis and to estimate in each patient
the IFI specific risk, we here propose a practical consultation tool
composed of a table where risk categories, their related risk factors,
and the HMs, are reported and matched (Table 1, part 1 and 2).
This estimated risk stratification was developed correlating each
disease class with the variables risk factors, categorized according to
patient’s features, underlying comorbidities, immunity status,
environmental factors, neutropenic status, disease and therapy or
transplant’s procedures.
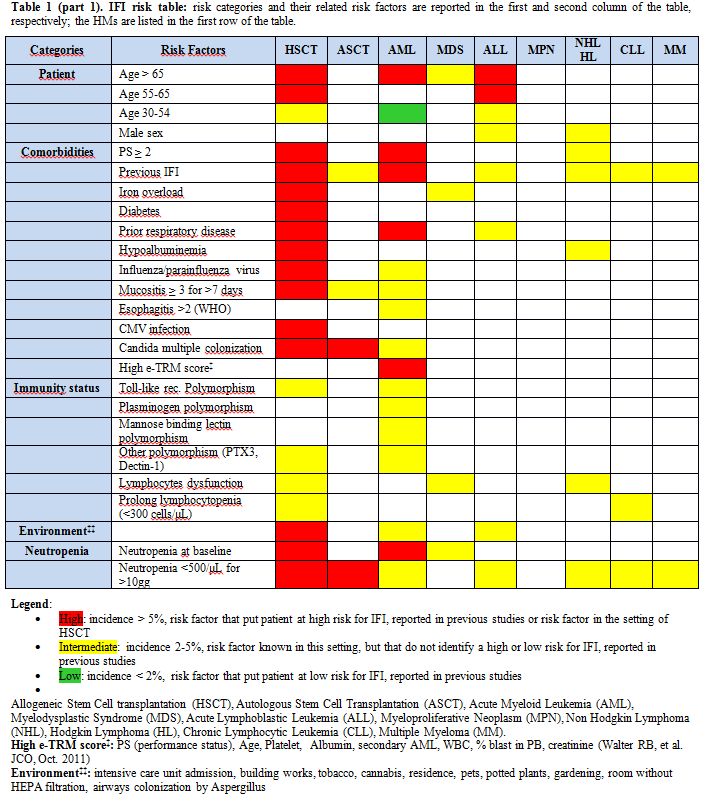 |
Table
1 (part 1). IFI risk table: risk categories and their related risk
factors are reported in the first and second column of the table,
respectively; the HMs are listed in the first row of the table. |
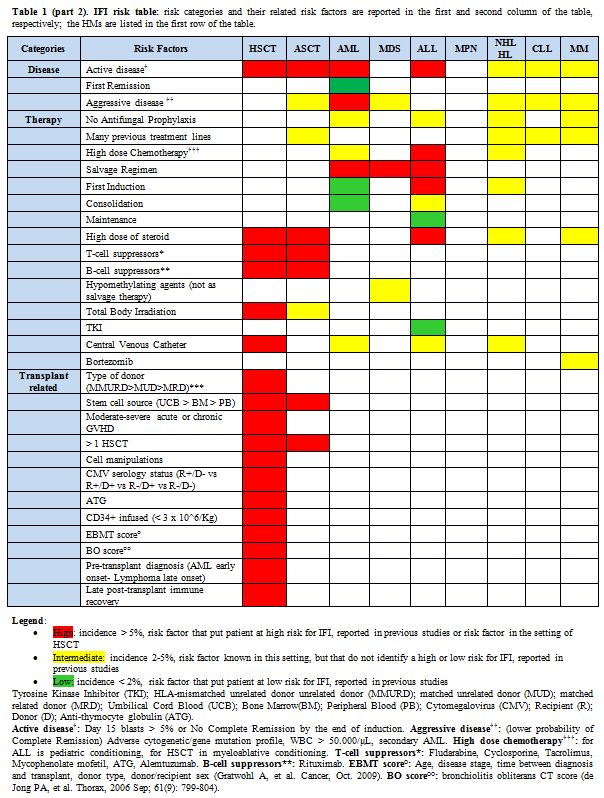 |
Table
1 (part 2). IFI risk table: risk categories and their related risk
factors are reported in the first and second column of the table,
respectively; the HMs are listed in the first row of the table. |
By
this approach, each box of the table represents a matching of a
specific disease with a specific risk factor. Red boxes, expressing a
high risk (HR) of IFI, are used to indicate a reported incidence of IFI
above 5%; yellow boxes, expressing an intermediate risk (IR) of IFI,
are used to indicate a reported incidence of IFI of 2-5%; green boxes,
expressing low risk (LR) of IFI, are used to indicate a reported
incidence of IFI minor of 2%. In the case of lacking data, the boxes
are white.Looking
at the colored boxes, people can read this table from two different
points of view, by focusing on the risk categories or vice versa
on the specific HM. In general, the horizontal reading of the table
highlights the principal IFI risk factors, regardless of the underlying
disease. In particular, red boxes appear to be associated with a long
history of HM, with a relapse or refractory disease, a prolong
neutropenia, older age, predisposing polymorphisms, pulmonary
comorbidities, intense chemotherapy and prolong used of steroids. Some
of these risk factors are routinely screened in the clinical practice,
others, like predisposing genetic polymorphisms, are used only in
experimental setting, but look promising. On the other hand, the
vertical reading of the table highlights the disease mostly associated
with IFI, in particular, AML and patients undergoing HSCT.It
should be underlined that each disease may present one or more risk
factors and that the risk factors may vary during the course of illness
and due to the type of treatments. For this reasons, it is important to
follow the patient over time, with a dynamic score, evaluating the
presence or absence of risk factors, with the aim to start or withdrawn
an appropriate antifungal prophylaxis or treatment. In this setting,
this table allows a rapid consultation in the clinical practice. In
conclusion, this IFI’s risk table may represent a useful and simple
tool to assess over time the risk of developing IFI in patients with
HMs and may help to plan an appropriate antifungal stewardship. References
- Pagano L, Akova M, Dimopoulos G, Herbrecht R,
Drgona L, Blijlevens N. Risk assessment and prognostic factors for
mould-related diseases in immunocompromised patients. Journal of
Antimicrobial Chemotherapy 2011: 66: i5-i14. http://jac.oxfordjournals.org/content/66/suppl_1/i5.abstract
- Herbrecht
R, Bories P, Moulin J-C, Ledoux M-P, Letscher-Bru Vr. Risk
stratification for invasive aspergillosis in immunocompromised
patients. Annals of the New York Academy of Sciences 2012:1272: 23-30. http://dx.doi.org/10.1111/j.1749-6632.2012.06829.x

- Ananda-Rajah
MR, Cheng A, Morrissey CO, et al. Attributable Hospital Cost and
Antifungal Treatment of Invasive Fungal Diseases in High-Risk
Hematology Patients: an Economic Modeling Approach. Antimicrobial
Agents and Chemotherapy 201: 55: 1953-1960. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3088208/

- Heimann
SM, Vehreschild MJGT, Cornely OA, et al. A cost and resource
utilization analysis of micafungin bridging for hemato-oncological
high-risk patients undergoing allogeneic stem cell transplantation.
European Journal of Haematology 2015: 94: 526-531. http://dx.doi.org/10.1111/ejh.12466

- Pagano
L, Busca A, Candoni A, et al. Risk stratification for invasive fungal
infections in patients with hematological malignancies: SEIFEM
recommendations. Blood Reviews 2016. http://www.sciencedirect.com/science/article/pii/S0268960X16300753

[TOP]





