Emanuele Cencini1,2, Alberto Fabbri1, Umberto Arrigucci3, Alfonso Cerase3 and Monica Bocchia1,2
1 Unit of Hematology, Azienda Ospedaliera Universitaria Senese, Siena, Italy.
2 University of Siena, Siena, Italy.
3
Unit of Neuroimaging and Neurointervention, Department of Neurological
and Sensorineural Sciences, Azienda Ospedaliera Università Senese,
"Santa Maria alle Scotte" University and NHS Hospital, Siena, Italy.
Corresponding
author: Dr. Emanuele Cencini, MD. Unit
of Hematology, University Hospital. Viale Bracci, 16 - 53100 Siena,
Italy. tel: + 39 0577 586798, fax:+ 39 0577 586185. E-mail:
cencioema@libero.it
Published: June 16, 2017
Received: March 13, 2017
Accepted: May 10, 2017
Mediterr J Hematol Infect Dis 2017, 9(1): e2017040 DOI
10.4084/MJHID.2017.040
This article is available on PDF format at:

This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Central
nervous system (CNS) relapse is an infrequent but severe complication
for DLBCL patients, associated with poor prognosis. Intravenous
prophylaxis with high-dose methotrexate has shown promising results but
is rarely feasible in elderly and/or nephropathic patients.
A 83
years old woman with CNS relapse occurred 6 months after
chemoimmunotherapy. The patient was defined ineligible for radiotherapy
(RT) and started oral Temozolomide 250mg daily for 5 consecutive days
without any improvement after 1st cycle.
We administered
lenalidomide 25mg daily for 21 days every 28 days together with
temozolomide 250mg daily for 5 days every 28 days. The patient
experienced a rapid improvement of general and cognitive conditions;
Gadolinium-enhanced brain MRI showed a wide reduction of neoplastic
tissue. The patients maintained good clinical conditions with mild
treatment toxicity until the end of the 6th cycle, when brain MRI
showed disease progression and the patient died 1 month later.
We
suggest lenalidomide could be a feasible option for CNS relapse in
elderly DLBCL patients and it could be associated in future studies
with other cytotoxic agents such as temozolomide.
|
Introduction
Central
nervous system (CNS) relapse is an infrequent but severe complication
for diffuse large B-cell lymphoma (DLBCL) patients, associated with
poor prognosis.[1] Several risk factors have been
identified for CNS recurrences, such as localizations at testis, orbit,
paranasal sinuses, more than 1 extranodal involved site and elevated
lactate dehydrogenase (LDH). A new prognostic model has recently been
proposed, called CNS international prognostic index (IPI), including
kidney and/or adrenal localization.[2,3] However, CNS
prophylaxis with intrathecal methotrexate and/or cytarabine is not
possible in all patients, and current guidelines and recent studies
suggest it is not sufficient in a majority of cases due to a prevalent
parenchymal and not meningeal involvement in most relapsed DLBCL
patients.[4,5] Intravenous prophylaxis with high-dose
methotrexate has shown promising results but is rarely feasible in
elderly and/or nephropathic patients.[4,5]
Overall,
very few agents pass through blood brain barrier (BBB), such as
temozolomide, but long-term remissions in primary CNS lymphoma are
seldom observed with this drug.[6]
Lenalidomide has a pleiotropic effect and has been widely used in relapsed DLBCL;[7] there are some interesting reports about its efficacy in CNS relapse and its capacity to cross BBB.[8-11]
According to this background, we would like to report our experience in a case of CNS relapse in an elderly patient.
Case Report
In
2015, April, an 83 years old woman was referred to our institution
because of a diagnosis of DLBCL was made by a biopsy of a right orbit
injury. Physical examination showed no enlarged lymph nodes, blood cell
count was normal, LDH was mildly increased (249IU/l, normal value
135-225 IU/l). Bone marrow biopsy revealed no infiltration, computed
tomography (CT) scan showed multiple mediastinal and celiac enlarged
lymph nodes, together with parenchymal splenic localizations. ECOG
performance status was 2. The patient was considered ineligible for
i.v. high-dose methotrexate (MTX) and, according to conflicting results
of i.t. prophylaxis, recent data by Muravski and colleagues and
patient’s willing, did not receive i.t. MTX.[12]
Immunochemotherapy
with etoposide, mitoxantrone, cyclophosphamide, vincristine,
prednisone, and bleomycin (VNCOP-B) was administered, in association
with rituximab.[13,14] The patient received
chemotherapy weekly and rituximab every 2 weeks for 12 weeks, as
previously published. The regimen was completed without dose delays or
dose reductions; total body CT scan showed a complete remission (CR).
Treatment toxicity was mild with only grade 1 peripheral neuropathy
that disappeared after treatment completion; thank primary prophylaxis
with filgrastim no neutropenia occurred.
The patient maintained CR
for 6 months when she came to the emergency department because of a
headache and cognitive impairment. Brain CT scan showed CNS relapse
with a right frontal mass that extended to the ipsilateral
frontal-basal areas, a wide ipsilateral vasogenic edema with
ventricular compression and initial trans-falcial herniation. The
patient was defined ineligible for radiotherapy (RT) because of age,
wide vasogenic edema and high risk of neurotoxicity and started
intramuscular dexamethasone 8mg daily and oral temozolomide 250mg daily
for 5 consecutive days without any improvement after 1st cycle; total body CT scan (Figure 1 A) showed a further increase of the right frontal mass (diameter 7cm) without other disease localizations.
Given
the promising data of lenalidomide use for CNS lymphoma and the lack of
other treatment options, we decided to administer lenalidomide 25mg
daily for 21 days every 28 days together with temozolomide 250mg daily
for 5 days every 28 days. The patient experienced a rapid improvement
in general and cognitive conditions after the 1st
cycle, headache disappeared, both Activities of Daily Living (ADL) and
Instrumental Activities of Daily Living (IADL) improved. We decided to
continue this association; Gadolinium-enhanced brain MRI (Figure 1 B) was performed after the 2nd
cycle and showed a wide reduction of neoplastic tissue (diameter 37
mm), vasogenic edema, and mass effect. In accordance with these
promising results, the patients received other 4 cycles. Therapy was
well tolerated, grade 2 neutropenia without infections and grade 2
thrombocytopenia that recovered after one-week dose delay were
observed; no extra-hematological toxicity was observed, and no
hospitalization was needed.
The patients maintained good clinical conditions until the end of the 6th cycle when a headache recurred. Gadolinium-enhanced brain MRI (Figure 1 C)
showed disease progression. Clinical conditions rapidly worsened, the
patient came to the hospital, we tried to administer steroid therapy,
mannitol, and oral procarbazine, but the patient did not respond to
treatment and died.
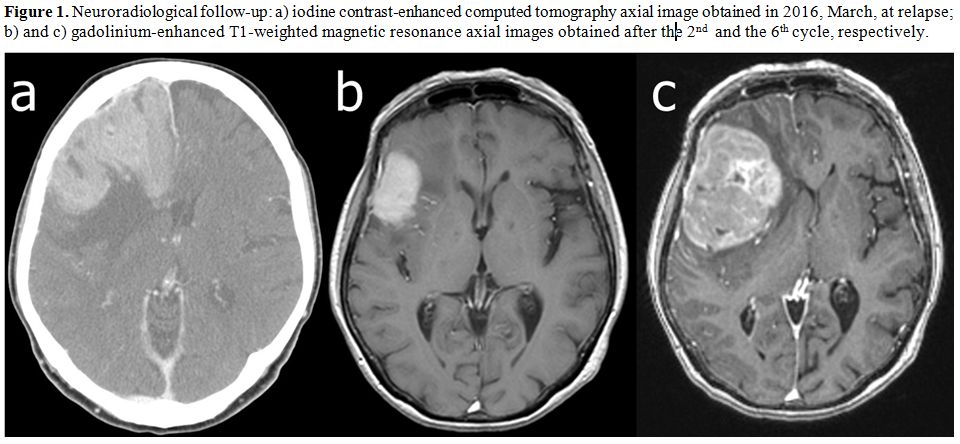 |
Figure 1. Neuroradiological follow-up: a)
iodine contrast-enhanced computed tomography axial image obtained in
2016, March, at relapse; b) and c) gadolinium-enhanced T1-weighted
magnetic resonance axial images obtained after the 2nd and the 6th cycle, respectively. |
Discussion
CNS
relapse in elderly DLBCL patients is an unmet clinical need to date.[1]
These patients are usually not eligible for HD-MTX and/or HD cytarabine
and have a dismal prognosis, mainly because there is a lack of
cytotoxic agents that cross BBB with manageable toxicity. Whole brain
RT is characterized by a substantial neurotoxicity that limits its
feasibility especially in older patients.[15]
Procarbazine,
lomustine, and vincristine (PCV) was administered to 8 recurrent CNS
lymphoma patients (age 36-72 years old) and showed an overall response
rate (ORR) of 50% with a median progression-free survival (PFS) of 7
months.[16] Temozolomide, an alkylating agent that
can penetrate into the brain, demonstrated promising results both as
first-line treatment and for recurrent primary CNS lymphoma. In a
retrospective series of 17 elderly patients CR rate was 47%, median PFS
and overall survival (OS) were 5 and 21 months, respectively.[6]
The
possibility for lenalidomide to accumulate in the cerebrospinal fluid
was reported in a case of blastoid mantle cell lymphoma.[9]
Lenalidomide as salvage therapy for recurrent primary CNS lymphoma was
administered to 6 elderly patients (median age 73.5 years, range
64-78), 2/6 patients achieved CR and 1/6 achieved partial remission
(PR).[8] Salati and colleagues showed a leptomeningeal
relapse in a patient with DLBCL successfully treated with lenalidomide
monotherapy.[11] The patient was elderly, had an
early relapse after first-line chemoimmunotherapy of a double-hit DLBCL
and received high-dose MTX and cytarabine as salvage treatment,
alternating with bi-weekly liposomal cytarabine. MRI showed a
significant reduction of leptomeningeal contrast enhancement, the
patient refused RT and was successfully consolidated with lenalidomide
15mg daily for 21 every 28 days, achieving a complete and durable
response (month+9).
Moreover, an interesting phase I study of
lenalidomide was presented at last International Conference on
Malignant Lymphoma (ICML) meeting, 6 out of 8 patients achieved at
least PR, in 2 patients a duration of response of more than 1 year was
reported.[17]
Lenalidomide in combination has shown an unexpected toxicity, and a dose of 5 mg has been suggested.[18,19]
It is important to note that in our case the combination with
temozolomide of lenalidomide daily dose of 15 mg was well tolerated.
Conclusions
According
to these promising results and our experience in a very elderly
patient, we suggest lenalidomide could be a feasible option for CNS
relapse in aged DLBCL patients, and it could be associated in future
studies with other cytotoxic agents such as temozolomide.
References
- A, Orfao A; Spanish Lymphoma Group (GELTAMO).
Guidelines for diagnosis, prevention and management of central nervous
system involvement in diffuse large B-cell lymphoma patients by the
Spanish Lymphoma Group (GELTAMO). Haematologica, 2017; 102: 235-245
PMID:27846613 https://doi.org/10.3324/haematol.2016.149120

- Schmitz
N, Zeynalova S, Nickelsen M, Kansara R, Villa D, Sehn LH, Glass B,
Scott DW, Gascoyne RD, Connors JM, Ziepert M, Pfreundschuh M, Loeffler
M, Savage KJ. CNS International Prognostic Index: A Risk Model for CNS
Relapse in Patients With Diffuse Large B-Cell Lymphoma Treated With
R-CHOP. J Clin Oncol, 2016; 34: 3150-3156 PMID:27382100 https://doi.org/10.1200/JCO.2015.65.6520

- Cheah
CY, Seymour JF. Central nervous system prophylaxis in non-Hodgkin
lymphoma: who, what, and when? Curr Oncol Rep, 2015; 17: 25
PMID:25912004 https://doi.org/10.1007/s11912-015-0450-4

- Tilly
H, Gomes da Silva M, Vitolo U, Jack A, Meignan M, Lopez-Guillermo A,
Walewski J, André M, Johnson PW, Pfreundschuh M, Ladetto M; ESMO
Guidelines Committee. Diffuse large B-cell lymphoma (DLBCL): ESMO
Clinical Practice Guidelines for diagnosis, treatment and follow-up.
Ann Oncol, 2015; 26: v116-125 PMID:26314773 https://doi.org/10.1093/annonc/mdv304

- Ferreri
AJ, Bruno-Ventre M, Donadoni G, Ponzoni M, Citterio G, Foppoli M,
Vignati A, Scarfò L, Sassone M, Govi S, Caligaris-Cappio F.
Risk-tailored CNS prophylaxis in a mono-institutional series of 200
patients with diffuse large B-cell lymphoma treated in the rituximab
era. Br J Haematol, 2015; 168: 654-662 PMID:25312994 https://doi.org/10.1111/bjh.13194

- Kurzwelly
D, Glas M, Roth P, Weimann E, Lohner H, Waha A, Schabet M, Reifenberger
G, Weller M, Herrlinger U. Primary CNS lymphoma in the elderly:
temozolomide therapy and MGMT status. J Neurooncol, 2010; 97: 389-392
PMID:19841864 https://doi.org/10.1007/s11060-009-0032-0

- Witzig
TE, Vose JM, Zinzani PL, Reeder CB, Buckstein R, Polikoff JA,
Bouabdallah R, Haioun C, Tilly H, Guo P, Pietronigro D, Ervin-Haynes
AL, Czuczman MS. An international phase II trial of single-agent
lenalidomide for relapsed or refractory aggressive B-cell non-Hodgkin's
lymphoma. Ann Oncol, 2011; 22: 1622-1627 doi: 10.1093/annonc/mdq626.
PMID:21228334 https://doi.org/10.1093/annonc/mdq626

- Houillier
C, Choquet S, Touitou V, Martin-Duverneuil N, Navarro S, Mokhtari K,
Soussain C, Hoang-Xuan K. Lenalidomide monotherapy as salvage treatment
for recurrent primary CNS lymphoma. Neurology, 2015; 84: 325-326
PMID:25527263 https://doi.org/10.1212/WNL.0000000000001158

- Cox
MC, Mannino G, Lionetto L, Naso V, Simmaco M, Spiriti MA. Lenalidomide
for aggressive B-cell lymphoma involving the central nervous system? Am
J Hematol, 2011; 86: 957 doi: 10.1002/ajh.22148. No abstract available.
PMID:21990093 https://doi.org/10.1002/ajh.22148

- Rubenstein
JL, Treseler PA, Stewart PJ. Regression of refractory intraocular large
B-cell lymphoma with lenalidomide monotherapy. J Clin Oncol, 2011; 29:
595-597 PMID:21519022 https://doi.org/10.1200/JCO.2011.34.7252

- Salati
M, Tarantino V, Maiorana A, Bettelli S, Luminari S. Durable remission
in a patient with leptomeningeal relapse of a MYC/BCL6-positive
double-hit DLBCL treated with lenalidomide monotherapy. Hematol Oncol
2016 [Epub ahead of print] PMID:27301994 https://doi.org/10.1002/hon.2315

- Murawski
N, Held G, Ziepert M, Kempf B, Viardot A, Hänel M, Witzens-Harig M,
Mahlberg R, Rübe C, Fleckenstein J, Zwick C, Glass B, Schmitz N,
Zeynalova S, Pfreundschuh M. The role of radiotherapy and intrathecal
CNS prophylaxis in extralymphatic craniofacial aggressive B-cell
lymphomas. Blood, 2014; 124: 720-728 https://doi.org/10.112/bl8ood-2013-10-535021 PMID:24939657

- Fina
M, Tani M, Stefoni V, Musuraca G, Marchi E, Pellegrini C, Alinari L,
Derenzini E, Bacci F, Pileri S, Baccarani M, Zinzani PL. VNCOP-B plus
rituximab in the treatment of diffuse large B-cell lymphoma in the
elderly. Leuk Lymphoma, 2007; 48: 2167-2171. PMID:17990178 https://doi.org/10.1080/10428190701642102 PMid:17990178

- Ishii
K, Urase F, Nagare Y, Kimura H, Manabe M, Yagi T, Teshima H, Hayashi K,
Shibano M, Tsukaguchi M, Katsurada T, Mugitani A, Kitayama H, Nomura
S.VNCOP- B plus rituximab therapy in elderly patients with aggressive
B-cell non-Hodkin lymphoma: A multicenter experience. Arch Gerontol
Geriatr, 2010; 51:209-215. https://doi.org/10.1016/j.archger.2009.10 PMID:19926148

- Kasenda
B, Loeffler J, Illerhaus G, Ferreri AJ, Rubenstein J, Batchelor TT. The
role of whole brain radiation in primary CNS lymphoma. Blood, 2016;
128: 32-66 PMID:27207798 https://doi.org/10.1182/blood-2016-01-650101

- Kim
YJ, Choe JH, Park JH, Hong YK. Efficacy of Procarbazine, Lomustine, and
Vincristine Chemotherapy for Recurrent Primary Central Nervous System
Lymphomas. Brain Tumor Res Treat, 2015; 3: 75-80 PMID:26605261 https://doi.org/10.14791/btrt.2015.3.2.75

- Rubenstein
JL, Formaker P, Wang X, Chen N, Fraser E, Munster P, Damato B.
Lenalidomide is highly active in recurrent CNS lymphomas: phase I
investigation of lenalidomide plus rituximab and outcomes of
lenalidomide as maintenance monotherapy. Hematol Oncol (ICML abstracts)
2015; 33 :175.

- Quach
H, Fernyhough L, Henderson R, Corbett G, Baker B, Browett P, Blacklock
Martín A, Redondo AM, Dlouhy I, Salar A, González-Barca E, Canales M,
Montes-Moreno S, Ocio EM, López-Guillermo A, Caballero D; Spanish Group
for Lymphomas and Autologous Bone Marrow (GELTAMO).. Lenalidomide in
combination with R-ESHAP in patients with relapsed or refractory
diffuse large B-cell lymphoma: a phase 1b study from GELTAMO group. Br
J Haematol. 2016 Apr;173(2):245-52. https://doi.org/10.1111/bjh.13945

- H,
Forsyth C, Underhill C, Cannell P, Trotman J, Neylon A, Harrison S,
Link E,Swern A, Cowan L, Dimopoulos MA, Miles Prince H. Upfront lower
dose lenalidomide is less toxic and does not compromise efficacy for
vulnerable patients with relapsed refractory multiple myeloma: final
analysis of the phase II RevLitestudy. Br J Haematol. 2017
May;177(3):441-448. Epub 2017 Feb 15. PubMed PMID: 28197996 https://doi.org/10.1111/bjh.14562 .

]




















