Bosa L.1, Da Silva L.2, Mendes D.V.2, Sifna A.2, Sargento Mendes M.2, Riccardi F.3,4 and Colombatti R.4,5
1 Department of Women’s and Child’s Health, Azienda Ospedaliera-Università di Padova, Padova, Italy.
2 Hospital Raoul Follereau, Bissau, Guinea Bissau.
3 Department of Biomedicine and Prevention, University of Tor Vergata, Roma, Italy.
4 Aid, Health and Development Onlus, Roma, Italy.
5
Clinic of Pediatric Hematology-Oncology, Department of Women’s and
Child’s Health, Azienda Ospedaliera-Università di Padova, Padova, Italy.
Corresponding
author: Raffaella
Colombatti, MD, PhD. Clinic of Pediatric Hematology Oncology,
Department of Women’s and Child’s Health, Azienda
Ospedaliera-Università di Padova, Padova, Italy. Tel: 0039-345-5356570;
0039-049-8218006. E-mail:
rcolombatti@gmail.com
Published: October 15, 2017
Received: July 10, 2017
Accepted: October 3, 2017
Mediterr J Hematol Infect Dis 2017, 9(1): e2017059 DOI
10.4084/MJHID.2017.059
This article is available on PDF format at:

This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background and Objectives: The
World Health Organization End tuberculosis (TB) Strategy, approved in
2014, aims at a 90% reduction in TB deaths and an 80% reduction in TB
incidence rate by 2030. One of the suggested interventions is the
systematic screening of people with suspected TB, belonging to specific
risk groups. The Hospital Raoul Follereau (HRF) in Bissau,
Guinea-Bissau, is the National Reference Hospital for Tuberculosis and
Lung Disease of the country. We performed an active case-finding
program among pediatric age family members and cohabitants of admitted
adult TB patients, from January to December 2013.
Methods:
Newly admitted adult patients with a diagnosis of TB were invited to
bring their family members or cohabitants in childhood age for clinical
evaluation in a dedicated outpatient setting within the hospital
compound. All the children brought to our attention underwent a medical
examination and chest x-ray. In children with clinical and/or
radiologic finding consistent with pulmonary TB, a sputum-smear was
requested.
Results: All
admitted adult patients accepted to bring their children cohabitants.
In total, 287 children were examined in 2013. Forty-four patients (15%)
were diagnosed with TB. The number needed to screen (NNS) to detect one
case of TB was 7. 35 patients (80%) had pulmonary TB; 2 of them were
sputum smear-positive. No adjunctive personnel cost was necessary for
the intervention.
Conclusions:
A hospital-based TB active case-finding program targeted to high-risk
groups like children households of severely ill admitted patients with
TB can successfully be implemented in a country with limited resources.
|
Introduction
According
to World Health Organization, tuberculosis (TB) is one of the top 10
causes of death worldwide, having killed 1.4 million people in 2015. In
the same year, there were an estimated 10.4 million new TB cases
worldwide, of which 1.0 million (10%) among children.[1]
TB is considered a poverty-related disease; half of the deaths from TB
are from the African region, where the problem of low resources is
further compounded by the high prevalence of HIV co-infection and
increasing mycobacterial drug resistance.[2-4]
One
of the Sustainable Development Goals (SDGs) adopted by United Nations
in 2015 is to end the epidemics of AIDS, TB, and malaria by 2030.[5]
The World Health Organization End TB Strategy, approved in 2014, aims
at a 90% reduction in TB deaths and an 80% reduction in TB incidence
rate by 2030, compared with 2015.[1] One of the suggested interventions within the resolution is the active case-finding of affected people,[6-7]
meaning the systematic screening of people with suspected TB, belonging
to specific risk groups. The diagnosis made early in the course of the
disease allows initiating treatment earlier, when the illness is not
widespread, and the general health is not heavily compromised, thereby
reducing either morbidity and mortality, and the incidence and
prevalence of the infection in the population. Under or late diagnosis
contributes to sustained transmission of the disease, while active case
finding can hasten the rate of decline. Dynamic models recently proved
that this strategy could be both powerful and cost-effective in
reducing TB incidence and mortality.[6,8] Many screening and diagnostic algorithms have been proposed to date.[6,9]
A
further major challenge is the diagnosis and cure of TB in children.
Childhood TB was long neglected by organizations dedicated both to TB
or child health at a global level. The main reasons for this phenomenon
are both the fact that children with TB are rarely contagious and the
many diagnostic difficulties of TB in childhood. Obtaining adequate
sputum samples from children for laboratory diagnosis is often
troublesome; the proportion of sputum smear-positive pediatric cases is
low. Moreover, the availability of Xpert MTB/RIF assay is low in Africa
outside of the research setting. Diagnosis often relies on clinical
evaluation supported by diagnostic exams, chiefly chest X-ray.[10-11] Since the majority of childhood TB cases are not diagnosed, the burden of the disease has been underestimated for a long time.
In
the last few years, there has been increasing attention in childhood TB
from international organizations and TB programs. In October 2013 WHO,
UNICEF, CDC and other organizations released the Roadmap for Childhood
Tuberculosis, with the goal of zero TB deaths in children.[12]
Guinea Bissau is a West African Country with a high TB burden,[1,13-14] and a high mortality among children living with TB households.[15]
We
performed an active case-finding program among pediatric age family
members, and cohabitants of adult TB patients admitted to the Hospital
Raoul Follereau (HRF) in Bissau, Guinea-Bissau, the National Reference
Hospital for Tuberculosis and Lung Disease of the country,[16] from January to December 2013.
Our
objectives were to demonstrate the high burden of undiagnosed childhood
TB and to show that a hospital-based active screening program could be
both feasible and effective, even in a low resource context.
Material and Methods
Study setting. Guinea-Bissau is a West African country located on the Atlantic Coast with a population of approximately 1.8 million people.[11]
Since independence from Portugal in 1974, Guinea-Bissau has been the
scene of considerable political upheaval, experiencing many military
coups and civil war. It’s one of the least developed countries, with a
poverty headcount ratio at national poverty lines of 69.3% in 2010,
according to World Bank data. In 2012 life expectancy at birth was 54
years, while healthy life expectancy at birth was 7 years lower, being
of 47 years, as reported by Global Health Observatory of WHO.
Infrastructural problems typical of post-conflict countries still
remain in Guinea Bissau and affect the health of the population.[17-18]
TB
is one of the leading causes of morbidity and mortality, with an
incidence rate of 373 cases per 100,000 persons per year. It is also
one of the 30 countries with the highest estimated numbers of incident
TB cases among people living with HIV.[1]
The
Hospital Raoul Follereau (HRF), located in Bissau, capital of
Guinea-Bissau, is the national reference center for the fight against
TB. The services it provides (inpatient, outpatient clinic, radiology,
and laboratory) are entirely free of charge for the patients, in a
beneficial public-private partnership.[16,19]
Patients with poor clinical conditions or with severe disease are
admitted to the HRF after referral from regional hospitals or health
centers across the entire country, according to the National Guidelines
for TB.[20]
Study Design.
Our cross-sectional study describes the outcomes of the pediatric
active case-finding program performed in the HRF from January to
December 2013. All patients admitted to the HRF receive weekly health
education sessions on Thursday afternoons. Moreover, a psychologist and
social service person perform daily rounds to talk with patients and
reinforce health education. During health education sessions the
importance of early screening was explained throughout the year, and
the active case finding project was presented. Every day, a nurse
invited newly admitted adult patients with a diagnosis of TB to bring
their family members or cohabitants in childhood age to clinically
evaluate them in a dedicated outpatient setting within the hospital
compound. Two mornings per week a physician and a nurse attended the
children in the outpatient clinic of the hospital. After obtaining
caregivers’ informed consent, all the children brought to our attention
underwent a medical examination and chest x-ray. In children with
clinical and/or radiologic finding consistent with pulmonary TB, a
sputum-smear was requested.
Three samples of sputum analysis
were collected and stained with Ziehl-Neelsen's staining technique: if
acid-fast bacilli were shown in at least two samples, children were
considered smear positive. Diagnosis of TB was made according to the
routinely used clinical protocol from the National Guidelines.[20]
Smear-positive children were diagnosed with confirmed pulmonary TB. In
case of a negative smear, despite a clinical history and a chest x-ray
suggestive of pulmonary TB, a course of antibiotics was administered
for 10 days and, if no improvement was observed, the child was
diagnosed as having presumptive TB and started on TB treatment. In case
of Extra pulmonary TB involving the lymph nodes, an aspirate from the
lymph nodes was analyzed for acid-fast bacilli; if the clinical
suspicion was of bone TB, an x-ray of the involved skeletal parts was
performed. Children with a diagnosis of TB were admitted while children
with other conditions were given appropriate treatment according to
need. Additional examinations were requested depending on the clinical
findings.
Data were reported on a written medical record,
including the name of the patient, gender, age, reported symptoms, test
results, diagnosis, and prescriptions. All children diagnosed with TB
during the outpatient clinic were admitted for therapy and observation
in the HRF.
The study was approved by the local Institutional Review Board.
Data Analysis.
Personal and clinical information was transferred from written medical
records to Microsoft Excel for Mac 15.32 (Microsoft Corporation,
Redmond, Washington, USA). The number needed to screen (NNS) to detect
one case of TB, i.e., the ratio between the number of persons screened
and the number of persons diagnosed with TB, was calculated.
Results
All
admitted adult patients accepted to bring their children cohabitants.
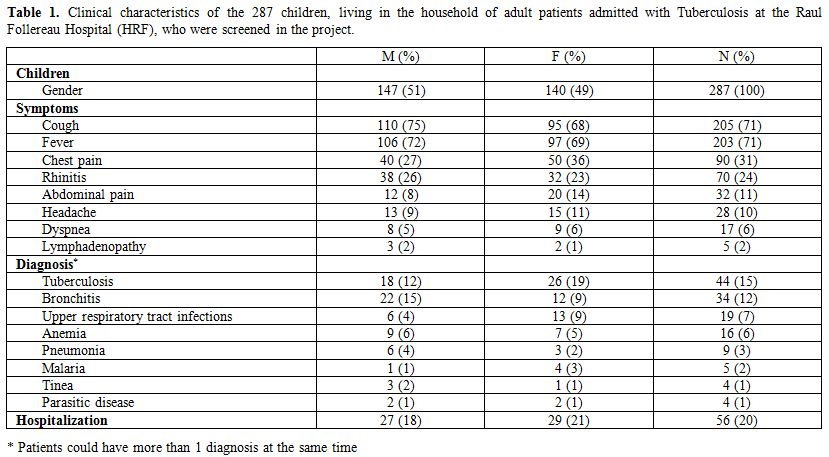
In total, 287 children were examined in 2013. The clinical
characteristics of screened patients are detailed in Table 1.
The children were 147 males (51%) and 140 females (49%). Mean age was
6.45 years (range: 1 month–16 years). The symptoms reported by the
caregiver were recorded. Only 25 patients (9%) were reported healthy,
while 262 (91%) had at least one symptom at home, mainly cough (205
patients, 71%), fever (203 patients, 71%), chest pain (90 patients,
31%) and rhinitis (70 patients, 24%).
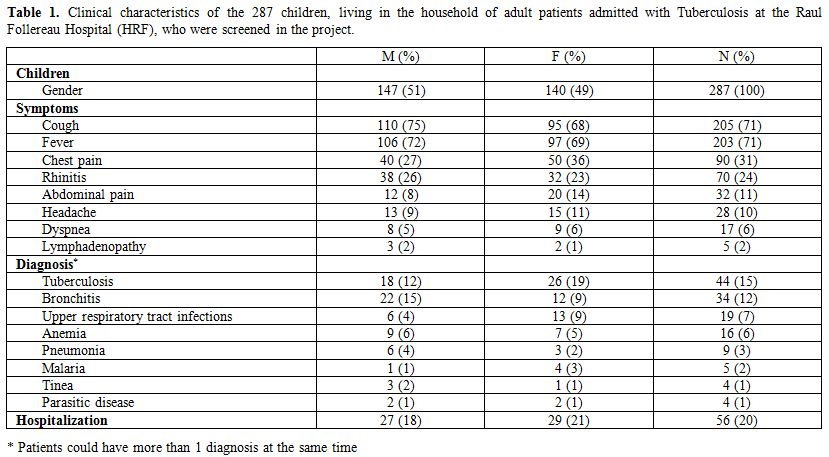 |
Table 1. Clinical characteristics of the
287 children, living in the household of adult patients admitted with
Tuberculosis at the Raul Follereau Hospital (HRF), who were screened in
the project. |
Overall,
the number of patients with concomitant HIV infection or AIDS was 9
(3%), while the total number of hospitalized patients was 56 (20%).
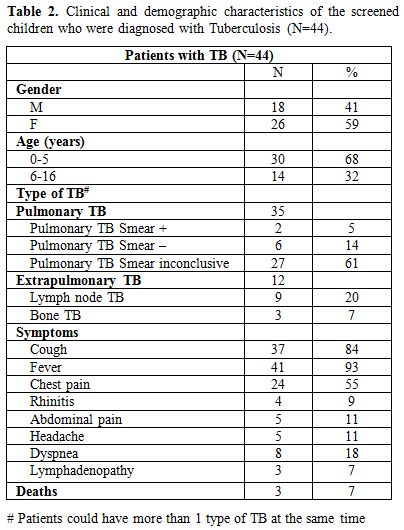
Forty-four patients (15%) were diagnosed with TB. The NNS was 7. The flowchart describing the diagnostic path is described in Figure 1, while clinical characteristics of TB patients are detailed in Table 2.
The patients were 18 males (49%) and 26 females (51%). Mean age was
5.75 years (range: 1 month-16 years). 35 patients (80%) had pulmonary
TB; 2 of them were sputum smear-positive (confirmed pulmonary TB),
while 33 were smear-negative and therefore had presumptive pulmonary
TB. Twelve patients had extra pulmonary TB, 3 of them having both
pulmonary and extra pulmonary disease. Of the 12 extra pulmonary TB, 9
had lymph node TB, 3 bone TB, one of them having Pott’s disease. Three
out of 44 patients with TB (7%) had concomitant HIV infection, although
not all patients received HIV testing. All TB cases were admitted to
HRF for therapy.
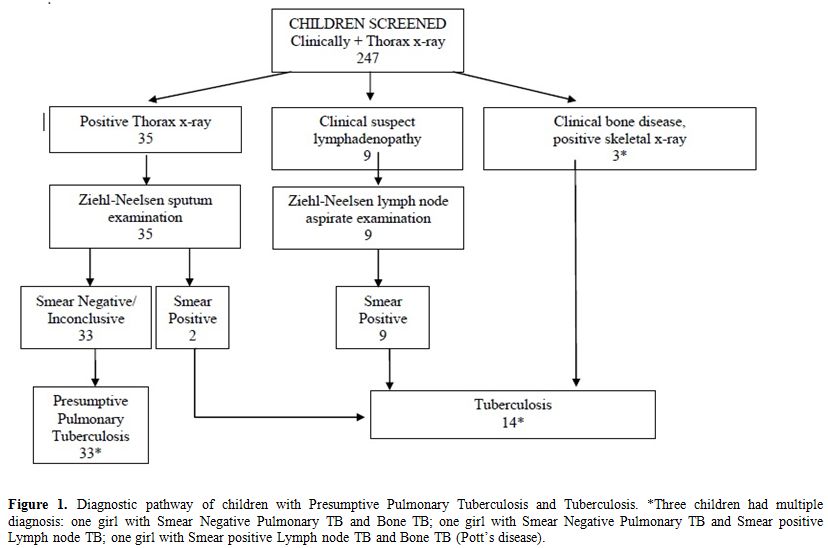 |
Figure 1.
Diagnostic pathway of children with Presumptive Pulmonary Tuberculosis
and Tuberculosis. *Three children had multiple diagnosis: one girl with
Smear Negative Pulmonary TB and Bone TB; one girl with Smear Negative
Pulmonary TB and Smear positive Lymph node TB; one girl with Smear
positive Lymph node TB and Bone TB (Pott’s disease). |
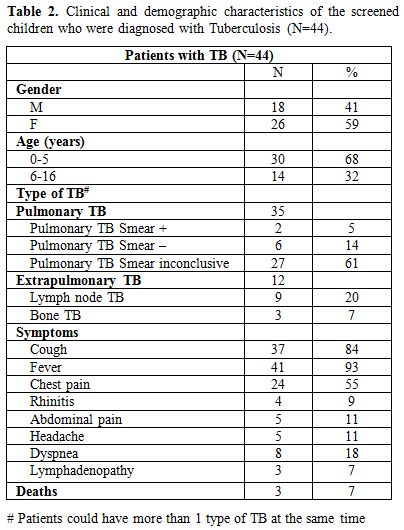 |
Table 2. Clinical and demographic characteristics of the screened children who were diagnosed with Tuberculosis (N=44). |
As
for the outcome of the hospitalized children, 3 patients (7%) died
during treatment; the others (41 patients, 93%) were discharged with
subsequent follow-up.
After TB the most common conditions
diagnosed in the screened patients were bronchitis (34 patients, 12%),
upper respiratory tract infection (19 patients, 7%), anemia (16
patients, 6%), pneumonia (9 patients, 3%) and malaria (5 patients, 2%).
Costs.
A detailed cost analysis was beyond the scope of this study.
Nevertheless, it is worth to notice that no adjunctive personnel cost
was necessary for these interventions: the physician and the nurse
twice a week were already working for the hospital and shifts were
rearranged to perform the planned activity without extra-hours. X-rays
are given to the HRF by the National Program against TB and did not
require further funding. Nevertheless, it can be estimated from our
previous experience[19] that the diagnosis of a TB case at admission would have cost 65,11 USD. Discussion
Our
study shows that TB active case-finding could be a powerful tool when
applied to a high-risk group of people like the pediatric
co-inhabitants of severely ill TB patients admitted in hospitals,
especially in a high TB burden country such as Guinea-Bissau.
The
low NNS (7 patients) to diagnose one case of TB reflects the impact of
the intervention on the target population, especially when compared to
the one that was found in other contact investigation projects in high
burden countries.[6,21-23] It also confirms that children living with adult TB patients are at high risk of contracting the disease.[23]
Even
if a 1 year period of active screening is too short to evaluate
long-term indicators, the low mortality of admitted and treated
patients (7%) demonstrates the value of a diagnosis performed early in
the course of the disease. Adult patients are generally admitted in
severe conditions, frequently with disseminated infections or
comorbidities. Through active screening, patients can be treated
earlier in the course of the disease.
Even though the active case
finding screening program was addressed to assumingly asymptomatic
children, not yet come to medical attention, only 25 patients (9%) were
reported healthy by their caregivers. Most children had at least one
sign or symptoms, such as cough, fever, rhinitis, and dyspnea. This may
be due to the high burden of other diseases among African children,
especially acute respiratory infections, which represent the third
cause of death in children under 5 in the country, according to WHO.[1]
Children living in Guinea-Bissau are still in a precarious situation
concerning water supply and housing and are often malnourished,[17-18] although data regarding malnutrition are not homogeneous among the cohorts evaluated in different parts of the country.[24]
Thus, symptom screening had very low specificity, since pulmonary TB is
a relatively rare cause of lower respiratory symptoms and signs, which
are common in pediatric age. We also hypothesize that the presence of
symptoms of any kind prompted caregivers to bring the children to our
attention. Given the frequent presence of other diseases, medical
history or physical examination alone were often insufficient to
properly discriminate between TB cases and healthy subjects or patients
having other conditions. Consequently, we performed a chest x-ray in
every screened child.
The rate of HIV infection was higher in
children with TB (7% vs. 3% of the whole sample). In fact, patients of
all ages with a new diagnosis of TB are 19 times more likely to be
co-infected with HIV than those without TB; equally, people with HIV
are 20 to 30 times more likely to develop TB than those without HIV.[25-27] Despite that, none of the observed deaths were among HIV infected children.
Our
program was designed to involve children who could be infected by
household contacts having TB, who represent a large proportion of the
pool of undetected TB patients. This is particularly true for young
children, for whom there is a clinical overlap between the features of
TB and other frequent causes of morbidity and mortality, such as
pneumonia. The prevalence of TB among children who are close contacts
of a TB case is high.[15,28-29]
Therefore, screening of children who are contacts is already widely
recommended, although rarely implemented systematically. TB in the
pediatric age seems to be under-reported, so cases with active TB can
spread the infection to their children who are underdiagnosed for TB.[7] Our pediatric active case-finding intervention could contribute to the goal of zero TB deaths in children.
Our
study was not designed to reach conclusive cost-effectiveness
information. Nevertheless, the costs for our active hospital-based case
finding intervention was low, compared to other active community-based
case finding experiences.[29] Early diagnosis could
reduce diagnostic and treatment costs for health services and families
while reducing mortality simply because less ill patients are taken in
care. Isoniazid preventive therapy was not given to children contacting
adult TB patients in this project, nor it is routinely performed in
Guinea Bissau, except for few pilot projects,[30]
despite the WHO recommendations. A further phase of the active case
finding program could be the implementation of a standardized isoniazid
preventive therapy to all contacts and not only the treatment of
children identified with confirmed or presumptive TB.
Our analysis
has several limits. First, we could not detail the magnitude of the
screening population and of the overall adult patients. The screening
was offered to all family members and cohabitants of admitted adult TB
patients, but extended families and house overcrowding have prevented
us from determining the total number of children that could have been
target. A joint project with the part of the TB National Program that
is working on the field could allow home visits by nurses or social
workers. Secondly, we could not compare the NNS of our study with
alternative active case-finding interventions applied in the same
setting, due to lack of comparable data. Moreover, local case
notification rate was unavailable. Finally, no systematic HIV test was
performed; therefore, the incidence of HIV co-infection could have been
underestimated.
Conclusion
Our
experience demonstrates that a simple TB active case-finding program
targeted to high-risk groups like children households of severely ill
admitted patients with TB, can successfully be implemented in a country
with limited resources.
Despite the short timescale and
notwithstanding the limitations of our study, our results show that a
broad implementation of similar active screening could have rapid
effects on TB transmission and disease in different low resource
settings. In fact, WHO recommends such screening for contacts of
bacteriologically confirmed cases to reduce the level of
underdiagnosis. The limited resources required for the intervention
makes it an attractive model that could produce savings in the long
term, and the identified gaps and limitations should guide future
interventions.
Acknowledgements
The Authors would
like to thank the Ministry of Health, the National Program Against
Tuberculosis, the staff of the Hospital Raoul Follereau and all the
patients and their families.
References
- World Health Organization. Global Tuberculosis Report 2016. http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1. Last accessed June 14th 2017
- Kirigia
JM, Muthuri RD. Productivity losses associated with tuberculosis deaths
in the World Health Organization African region. Infect Dis Poverty.
2016;5(1):43 https://doi.org/10.1186/s40249-016-0138-5 PMid:27245156 PMCid:PMC4888542

- Barter
DM, Agboola SO, Murray MB, Bärnighausen T. Tuberculosis and poverty:
the contribution of patient costs in sub-Saharan Africa--a systematic
review. BMC Public Health. 2012;12:980. https://doi.org/10.1186/1471-2458-12-980 PMid:23150901 PMCid:PMC3570447

- Rabna
P, Ramos J, Ponce G, Sanca L, Mané M, Armada A, Machado D, Vieira F,
Gomes VF, Martins E, Colombatti R, Riccardi F, Perdigão J, Sotero J,
Portugal I, Couto I, Atouguia J, Rodrigues A, Viveiros M. Direct
Detection by the Xpert MTB/RIF Assay and Characterization of Multi and
Poly Drug-Resistant Tuberculosis in Guinea-Bissau, West Africa. PLoS
One. 2015;10(5):e0127536. https://doi.org/10.1371/journal.pone.0127536

- United Nation General Assembly. Transforming our world: the 2030 Agenda for Sustainable Development Resolution A/70/L.1. http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E. Last accessed June 14th 2017
- Fox
GJ1, Barry SE, Britton WJ, Marks GB. Contact investigation for
tuberculosis: a systematic review and meta-analysis. Eur Respir J.
2013;41(1):140-56. https://doi.org/10.1183/09031936.00070812 PMid:22936710 PMCid:PMC3533588

- Oshi
DC, Chukwu JN, Nwafor CC, Meka AO, Madichie NO, Ogbudebe CL, Onyeonoro
UU, Ikebudu JN, Ekeke N, Anyim MC, Ukwaja KN, Aguwa EN. Does
intensified case finding increase tuberculosis case notification among
children in resource-poor settings? A report from Nigeria. Int J
Mycobacteriol. 2016;5(1):44-50. https://doi.org/10.1016/j.ijmyco.2015.10.007 PMid:26927989

- Azman
AS, Golub JE, Dowdy DW. How much is tuberculosis screening worth?
Estimating the value of active case finding for tuberculosis in South
Africa, China, and India. BMC Med. 2014;12:216. https://doi.org/10.1186/s12916-014-0216-0 PMid:25358459 PMCid:PMC4224697

- Van't
Hoog AH1, Onozaki I, Lonnroth K. Choosing algorithms for TB screening:
a modelling study to compare yield, predictive value and diagnostic
burden. BMC Infect Dis. 2014;14:532. https://doi.org/10.1186/1471-2334-14-532 PMid:25326816 PMCid:PMC4287425

- Seddon
JA, Jenkins HE, Liu L, Cohen T, Black RE, Vos T, Becerra MC, Graham SM,
Sismanidis C, Dodd PJ. Counting children with tuberculosis: why numbers
matter. Int J Tuberc Lung Dis. 2015;19 Suppl 1:9-16. https://doi.org/10.5588/ijtld.15.0471 PMCid:PMC4708268

- Starke JR. Improving tuberculosis care for children in high-burden settings. Pediatrics. 2014;134(4):655-7 https://doi.org/10.1542/peds.2014-1652 PMid:25266434

- World Health Organization. Roadmap for childhood tuberculosis: towards zero deaths. 2013. http://apps.who.int/iris/bitstream/10665/89506/1/9789241506137_eng.pdf?ua=1&ua=1. Last accessed on June 14th 2017
- Central Intelligence Agency. The World Factbook. Guinea Bissau. 2016. https://www.cia.gov/library/publications/the-world-factbook/geos/pu.html. Last accessed on June 14th 2017
- Lemvik
G, Rudolf F, Vieira F, Sodemann M, Østergaard L, Rodrigues A, Gomes V,
Aaby P, Wejse C. Decline in overall, smear-negative and HIV-positive TB
incidence while smear-positive incidence stays stable in Guinea-Bissau
2004-2011. Trop Med Int Health. 2014;19(11):1367-76. https://doi.org/10.1111/tmi.12378 PMid:25145557

- Gomes
VF, Andersen A, Wejse C, Oliveira I, Vieira FJ, Joaquim LC, Vieira CS,
Aaby P, Gustafson P. Impact of tuberculosis exposure at home on
mortality in children under 5 years of age in Guinea-Bissau. Thorax.
2011;66(2):163-7. https://doi.org/10.1136/thx.2010.141309 PMid:21148136

- Colombatti
R, Penazzato M, Bassani F, Vieira CS, Lourenço AA, Vieira F, Teso S,
Giaquinto C, Riccardi F. Malaria prevention reduces in-hospital
mortality among severely ill tuberculosis patients: a three-step
intervention in Bissau, Guinea-Bissau. BMC Infect Dis. 2011;11:57. https://doi.org/10.1186/1471-2334-11-57 PMid:21366907 PMCid:PMC3056796

- Colombatti
R, Vieira CS, Bassani F, Cristofoli R, Coin A, Bertinato L, Riccardi F.
Contamination of drinking water sources during the rainy season in an
urban post-conflict community in Guinea Bissau: implications for
sanitation priority. Afr J Med Med Sci. 2009;38(2):155-61 PMid:20175419

- Colombatti
R, Coin A, Bestagini P, Vieira CS, Schiavon L, Ambrosini V, Bertinato
L, Zancan L, Riccardi F. A short-term intervention for the treatment of
severe malnutrition in a post-conflict country: results of a survey in
Guinea Bissau. Public Health Nutr. 2008;11(12):1357-64. https://doi.org/10.1017/S1368980008003297 PMid:18652716

- Vieira
F, Sanha MS, Riccardi F, Colombatti R. Short term advantages of a
public-private partnership for tuberculosis in Guinea Bissau: reduction
of mortality and increased diagnostic capacity. Mediterr J Hematol
Infect Dis. 2014;6(1):e2014049. https://doi.org/10.4084/mjhid.2014.049 PMid:25045457 PMCid:PMC4103500

- Ministério da Saúde Pública Programa Nacional de Luta contra a Tuberculose. Manual de Tratamento. Bissau, Guinea Bissau. 2010. http://www.nationalplanningcycles.org/sites/default/files/country_docs/Guinea-Bissau/pndsii_2008-2017_gb.pdf. Last Accessed on June 14th 2017
- Blok
L, Sahu S, Creswell J, Alba S, Stevens R, Bakker MI. Comparative
meta-analysis of tuberculosis contact investigation interventions in
eleven high burden countries. PLoS One. 2015 Mar 26;10(3):e0119822. https://doi.org/10.1371/journal.pone.0119822 PMid:25812013 PMCid:PMC4374904

- Lala
SG, Little KM, Tshabangu N, Moore DP, Msandiwa R, van der Watt M,
Chaisson RE, Martinson NA. Integrated Source Case Investigation for
Tuberculosis (TB) and HIV in the Caregivers and Household Contacts of
Hospitalised Young Children Diagnosed with TB in South Africa: An
Observational Study. PLoS One. 2015;10(9):e0137518. https://doi.org/10.1371/journal.pone.0137518 PMid:26378909 PMCid:PMC4574562

- Puryear
S, Seropola G, Ho-Foster A, Arscott-Mills T, Mazhani L, Firth J,
Goldfarb DM, Ncube R, Bisson GP, Steenhoff AP. Yield of contact tracing
from pediatric tuberculosis index cases in Gaborone, Botswana. Int J
Tuberc Lung Dis. 2013;17(8):1049-55. https://doi.org/10.5588/ijtld.12.0933 PMid:23827029

- Patsche
CB, Rudolf F, Mogensen SW, Sifna A, Gomes VF, Byberg S, Wejse C. Low
prevalence of malnourishment among household contacts of patients with
tuberculosis in Guinea-Bissau. Int J Tuberc Lung Dis.
2017;21(6):664-669. https://doi.org/10.5588/ijtld.16.0673 PMid:28482961

- Kwan CK, Ernst JD. HIV and tuberculosis: a deadly human syndemic. Clin Microbiol Rev. 2011;24(2):351-76. https://doi.org/10.1128/CMR.00042-10 PMid:21482729 PMCid:PMC3122491

- Gustafson
P, Gomes VF, Vieira CS, Rabna P, Seng R, Johansson P, Sandström A,
Norberg R, Lisse I, Samb B, Aaby P, Nauclér A. Tuberculosis in Bissau:
incidence and risk factors in an urban community in sub-Saharan Africa.
Int J Epidemiol. 2004;33(1):163-72. https://doi.org/10.1093/ije/dyh026 PMid:15075165

- Gustafson
P, Gomes VF, Vieira CS, Samb B, Nauclér A, Aaby P, Lisse I. Clinical
predictors for death in HIV-positive and HIV-negative tuberculosis
patients in Guinea-Bissau. Infection. 2007;35(2):69-80 https://doi.org/10.1007/s15010-007-6090-3 PMid:17401710

- Morrison
J, Pai M, Hopewell PC. Tuberculosis and latent tuberculosis infection
in close contacts of people with pulmonary tuberculosis in low-income
and middle-income countries: a systematic review and meta-analysis.
Lancet Infect Dis. 2008;8(6):359-68. https://doi.org/10.1016/S1473-3099(08)70071-9

- Karki
B, Kittel G, Bolokon I Jr, Duke T. Active Community-Based Case Finding
for Tuberculosis With Limited Resources. Asia Pac J Public Health.
2017;29(1):17-27. https://doi.org/10.1177/1010539516683497 PMid:28033717 PMCid:PMC5349312

- Gomes
VF, Wejse C, Oliveira I, Andersen A, Vieira FJ, Carlos LJ, Vieira CS,
Aaby P, Gustafson P. Adherence to isoniazid preventive therapy in
children exposed to tuberculosis: a prospective study from
Guinea-Bissau. Int J Tuberc Lung Dis. 2011;15(12):1637-43. https://doi.org/10.5588/ijtld.10.0558 PMid:22118171

[TOP]