 |
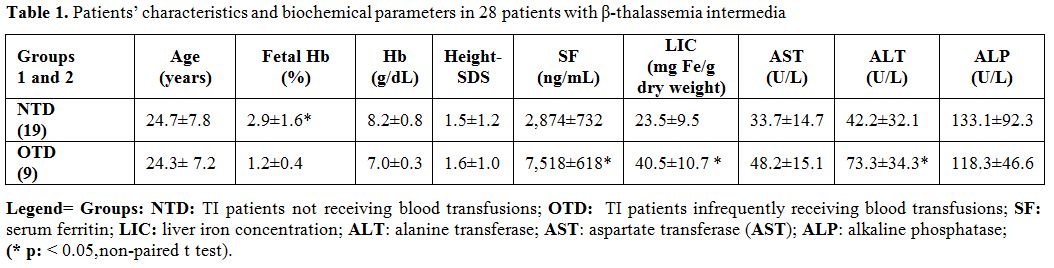
Table 1. Patients’ characteristics and biochemical parameters in 28 patients with β-thalassemia intermedia |
A short final stature (Ht-SDS < -2) occurred in 25% of patients and in 35.7 %. The IGF-1
SDS level was low, with no statistical difference among the two groups. FBG occurred in 17.8% of patients, DM in 25% and acquired hypogonadotrophic hypogonadism in 10.7% of them (2 patients with hypogonadotropic secondary amenorrhea and one male patient with acquired HH). The two females had secondary amenorrhea after a complete spontaneous pubertal development. Morning basal cortisol was low in one patient in the non-transfusion group. No thyroid or parathyroid abnormality was detected in any patient (Table 2).
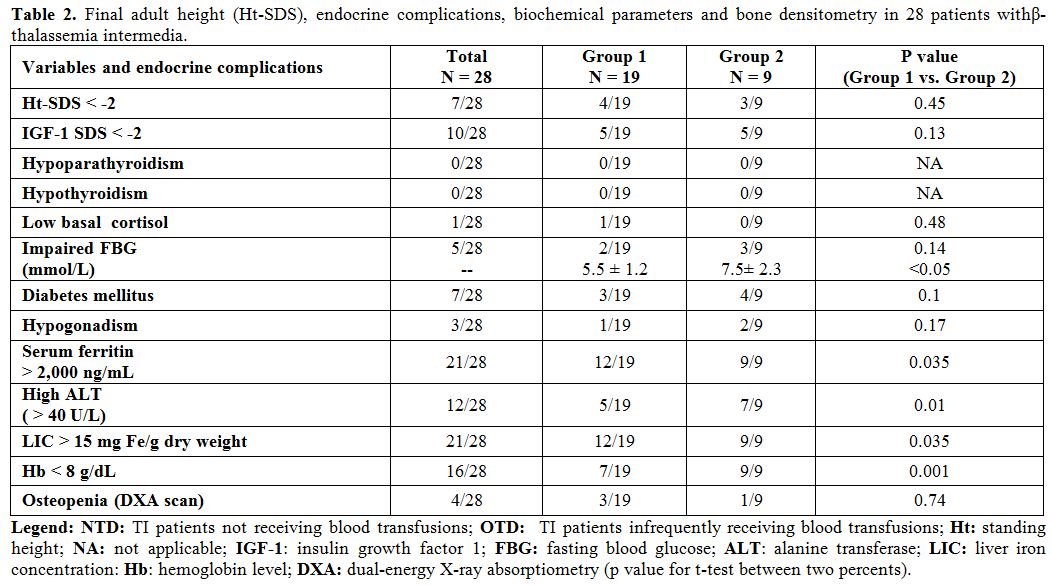 |
Table 2. Final adult height (Ht-SDS), endocrine complications, biochemical parameters and bone densitometry in 28 patients withβ-thalassemia intermedia. |
Increased ALT levels ( > 40 U/L) were detected in 42.8 % of patients. The levels resulted significantly higher in the transfused group (73.3±34.3 vs. 42.2±32.1 in NTD of Group 1). Total Hb and fetal Hb were significantly higher in Group 1 (8.2 ± 2.8 g/dL and 2.8 ± 1.6 %, respectively) versus Group 2 (7.0 ± 0.4 g/dl and 1.2 ± 0.42 g/dL, respectively). (Tables 1 and 2).
SF was > 2,000 ng/mL in 12/19 (63%) and LIC > 15 mg/g liver dry weight in 12/19 (63.1%) of patients who did not receive blood transfusion (Group 1) and in 100 % of patients who received occasional blood transfusions (Group 2). Liver iron content > 15 mg/g dry weight and serum ferritin level > 2, 000 ng/mL were detected in 75% of the patients. Four patients with SF concentration < 1,000 ng/mL had a high LIC > 15 mg/g dry weight. Although the mean SF level in males was comparable to the mean SF level in females, LIC of females was significantly lower.
Comparison of males versus females with TI showed that females had significantly better adult final Ht-SDS (- 0.45 ± 1.06 vs. -1.80 ± 0.88: p: 0.0001), higher IGF-1 SDS (-1.09 ± 1.73 vs. -1.80 ± 1.71;p: 0.01), lower LIC ( 24.4± 8.5 vs.32.3 ± 12.5 mg Fe/g dry weight; p: 0.03) , ALP (85.5 ± 20.9 vs. 144.6 ± 84.5 U/L; p:0.04 , Normal values: 40-129 U/L) and FBG (5.7 ± 2.2 vs. 7.1 ± 4.4 mmol/L; p: 0.04) compared to males.
ALT was not significantly lower in females versus males (43.1± 16.7 vs.55.1 ± 38.7 U/L; p: 0.6. Normal values: < 40 U/L).
LIC was correlated significantly with serum ferritin level (Figure 1). Ht-SDS was correlated significantly with IGF-1 SDS (Figure 2) and BMI. ALT concentrations were correlated significantly with LIC and SF level. Total Hb and fetal Hb did not correlate significantly with Ht-SDS or IGF-1 level. Osteopenia was diagnosed by DXA scan in 14.3% of patients (Table 2).
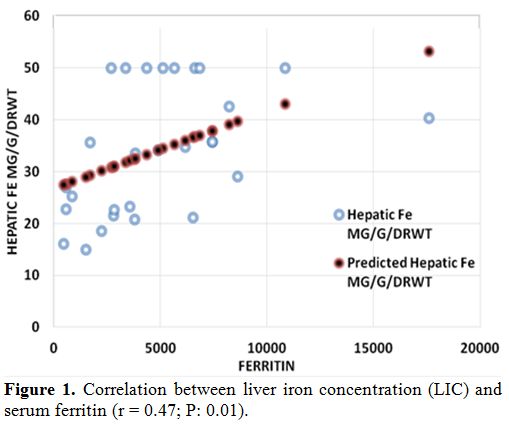 |
Figure 1. Correlation between liver iron concentration (LIC) and serum ferritin (r = 0.47; P: 0.01). |
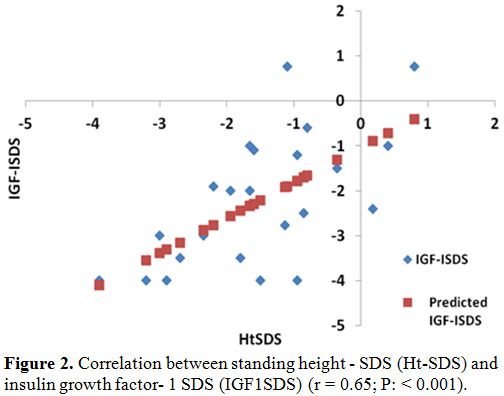 |
Figure 2. Correlation between standing height - SDS (Ht-SDS) and insulin growth factor- 1 SDS (IGF1SDS) (r = 0.65; P: < 0.001). |
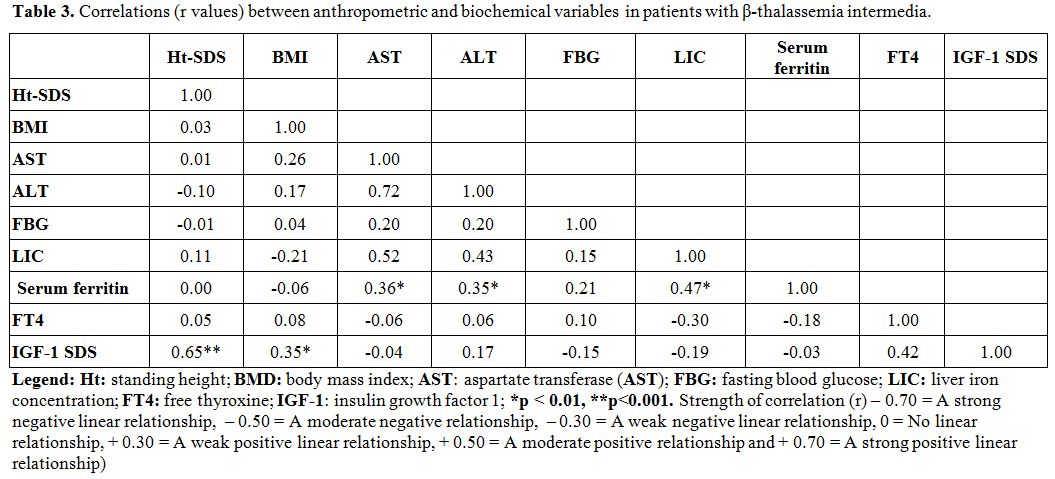 |
Table 3. Correlations (r values) between anthropometric and biochemical variables in patients with β-thalassemia intermedia. |