To date, there are only limited data about clinical characteristic, mode of delivery and newborn management in a pregnant woman infected by SARS-CoV-2.[3]
On March 30, 2020, a 33-year-old Italian pregnant at 40 weeks of gestation was admitted to the hospital on Department of Obstetrics and Gynecology in good health due to childbirth induction. From 24 to 28 March she experienced minor symptoms of rhinitis, anosmia and dysgeusia. A Floqswabs oropharyngeal swab in Copan universal transport medium (Copan Italia S.p.A., Brescia, Italy) was obtained on March 29 and resulted positive for SARS-CoV-2 on real-time reverse-transcription PCR assay, performed according to the Berlin/Cornan protocol.[4] Patient’s husband has been affected by fever, cough and dyspnea for 7 days, with confirmed SARS-CoV-2 three days before wife hospital admission. According to the parity, the weeks of gestation and her positivity to SARS-C-V-2 delivery was planned.
On admission, the physical examination revealed a body temperature of 36.6°C, a blood pressure of 110/70 mmHg, pulse rate of 86 beats per minute, respiratory rate of 16 breath per minute and oxygen saturation of 100% in ambient air. Lung auscultation was unremarkable and arterial blood gases were regular, with pH 7,45, pCO2 30.3 mm/Hg, and pO2 110 mm/Hg. Laboratory tests were within the normal range, except for elevated fibrinogen and d-dimer (Table 1).
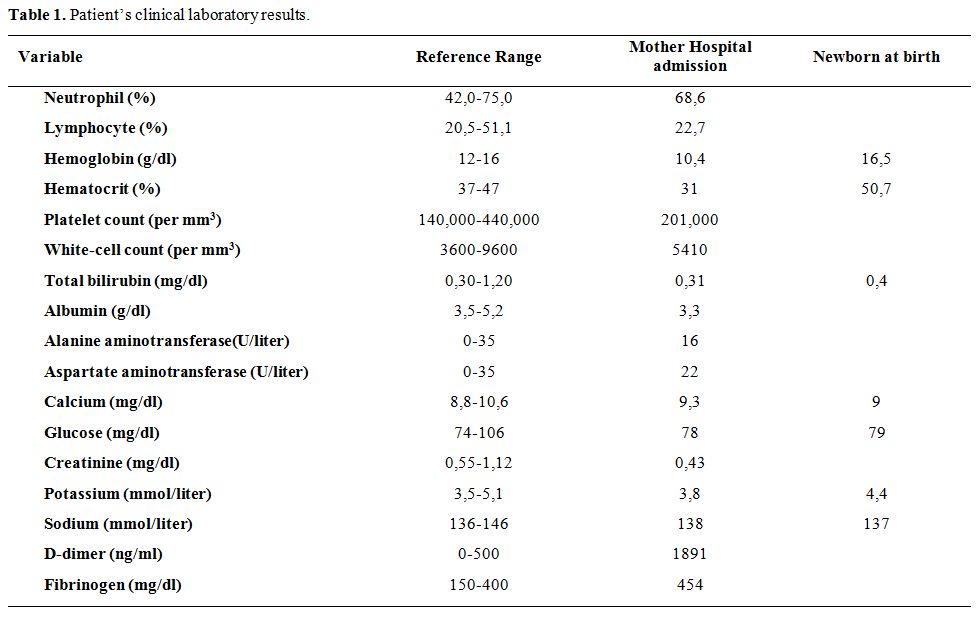 |
Table 1. Patient’s clinical laboratory results. |
The woman was admitted in a restricted COVID-delivery room area, in the presence of two midwives and one gynecologist, according to the internal hospital protocol. They enter the area together with the patient, leaving the room only after delivery or at the end of the work shift. Outside the area, another gynecologist and an anesthesiologist were on call for every need. Our obstetric-hospital COVID area is composed of two bedrooms for the patients, one delivery room, and one surgical room. The surgical room is provided of a surgical bed ready for the radiologic procedure. In the case of postpartum hemorrhage, the patient can be treated in the same area. A fully equipped neonatal islet was placed in the operating room for assistance to the newborn and any advanced neonatal resuscitation.
Since hospitalization, the patient was given surgical mask, and droplet and contact precaution were started.[5] In detail, for the delivery personal protective equipment of all medical personnel included gown, gloves, bouffant disposable surgical cap, knee-high shoe covers, eye protection, and N95 mask as there was a concern for aerosolization during the second stage of labor.
Vaginal birth was induced by oxytocin followed by the rupture of membrane. Oxytocin was administered intravenous according to induction protocol steps (2 mUI/min increasing 2 mUI every 20 min till regular uterine activity started), and then she had an uncomplicated vaginal delivery. The newborn’s Apgar score was 10 and 10. Newborn pharyngeal swab, collected ad immediately after 24 hours, tested negative for SARS-CoV-2.
After childbirth, the neonate was held in the negative pressure isolation room of the neonatal intensive care unit (NICU), placed in an incubator, until SARS-CoV-2 test results were available. The general conditions and vital signs have always remained good with standard routine checks (Table 1). Contextually nurses assisted the mother in the management of the draft of the colostrum, which was promptly administered to the baby in the first hours of life.
The patient remained in the delivery room area until the end of the post-partum period. Then she was transferred to the Infectious Disease Department and contacts between the staff, and the patient was minimized. She was in a good general condition in the absence of fever and cough. Chest radiographs performed after delivery was normal.
A screening test COVID-19 IgG/IgM fast assay (Screen Italia Srl, Perugia, Italy) was performed and yielded positive IgG and weakly positive IgM test. Forty-eight hours after delivery, the mother was assessed for SARS-CoV-2 RNA and resulted negative in the breast milk and positive in the oropharyngeal swab. She remained in the isolation room and, after consult between neonatologist and infectious disease, breastfeeding was permitted. Mother and newborn have been discharged together two days after delivery with the following recommendations: use a surgical mask during the contact with the neonate, wash and clean hands and body surface before touching the baby before breastfeeding.
Clinical follow-up after 7 and 15 days indicated the good clinical condition of the mother and newborn, with no signs of neonatal infection, oropharyngeal and rectal swab tests were negative for SARS-CoV-2 at 7 and 15 days.
This case describes uncomplicated labor and regular vaginal delivery in a woman with asymptomatic SARS-CoV-2 infection. Currently, limited data on the perinatal outcome are available in women who acquired SARS-CoV-2 infection in the proximity of delivery. Physiological and mechanical changes in pregnancy may increase susceptibility to infections with a special concern during the Coronavirus Disease 2019 (COVID-19) outbreak. Once a maternal infection of SARS-CoV-2 is suspected or confirmed, childbirth becomes challenging.
We identify several issues concerning the management of the reported case:
First, choice of childbirth modality, as there is no evidence of vertical transmission, vaginal delivery in asymptomatic SARS-CoV-2 infected is not contraindicated[6] as in this case.
Second, childbirth requires a specific hospital organization with space and staff dedicated. A neonate delivered by a SARS-CoV-2 infected mother requires a complex hospital organization, with the provision of an isolated room for mothers and/or neonates and firm implementation of the protective measures against contagion for health professionals as described in this case. The mother and baby had been cared for by a multidisciplinary medical team, including obstetrics, paediatricians, infectious diseases specialists.
Third, management of the newborn and breastfeeding. Based on current published guideline,[7,8] in asymptomatic mother direct breastfeeding, is advisable, under strict measures of infection control, i.e. a face mask should be worn due to the proximity between mother and child to reduce the risk of droplet transmission.
Fourthly, hospital discharge and the return home of the mother and infant.
Our case provides a preliminary view of the favourable outcome associated with pregnancy-related SARS-CoV-2 asymptomatic infection, and strategies for practical managing the pregnant women with infection.