Phakatip Sinlapamongkolkul1 and Pacharapan Surapolchai1.
1 Department of Pediatrics, Faculty of Medicine, Thammasat University, Thailand.
Correspondence to: Pacharapan Surapolchai, MD. Department of
Pediatrics, Faculty of Medicine, Thammasat University, 99/209 Moo 18
Phaholyothin Rd, Khlongluang, Pathumthani, 12120, Thailand. Tel:
+6629269514. E-mail:
doctorning@hotmail.com
Published: July 1, 2020
Received: March 16, 2020
Accepted: June 3, 2020
Mediterr J Hematol Infect Dis 2020, 12(1): e2020036 DOI
10.4084/MJHID.2020.036
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background:
Thalassemia remains a challenging chronic disease in Thailand, but
national prenatal screening, along with better treatment and
management, may have improved health-related quality of life (HRQoL)
for pediatric patients. We aimed to measure the HRQoL of
transfusion-dependent (TDT) and non-transfusion dependent (NTDT) of
these pediatric patients at our institute.
Methods:
We included all patients 2 – 18 years old, with TDT and NTDT, using the
Pediatric Quality of Life Inventory 4.0 Generic Core Scales (PedsQL)
and the EuroQol Group's Five Dimensions for Youth (EQ-5D-Y)
instruments. Patients and caregivers responded as appropriate for age.
Results:
Mean PedsQL total summary scores (TSS) (SD) of child self-reports and
parent proxy-reports were 81.00 (10.94) and 78.84 (16.72) from 150
participants. Mean EQ-5D-Y VAS (SD) for children was 89.27 (11.56) and
86.72 (10.62) for parent proxies. The most problematic EQ-5D-Y
dimension was "having pain or discomfort”. These scores had
significant correlations between the child and parental proxy
perspectives, as well as between the PedsQL and EQ-5D-Y. An age of 8 -
12 years and oral chelation therapy predicted lower self-reported
PedsQL TSS. Parental proxy-report predictors for reduced PedsQL TSS and
EQ-5D-Y VAS were primary school education for children, parental proxy
secondary school education, Universal Coverage insurance, and TDT.
Conclusion:
HRQoL scores of our pediatric thalassemia patients had improved from
the previous decade, and these findings may represent our better
standard of care. Some sociodemographic and clinical characteristics
may present negative impacts on HRQoL. More exploration is needed to
understand predictors and further improve HRQoL, especially for TDT
patients.
|
Introduction
Thalassemia
is an inherited hemoglobin disorder in which alpha and beta-globin
genetic mutations decrease globin synthesis. It is highly prevalent in
Africa, the Mediterranean region, the Middle East, the Indian
subcontinent, and Southeast Asia:[1-3] 40-50% of the Thai population likely carries some sort of thalassemia gene.[4-5]
In 1993, the Thai government began screening pregnant women for three
severe forms: homozygous β-thalassemia, β-thalassemia/HbE disease, and
Hb Bart's hydrops fetalis.[5] Thalassemia has
varying severity from asymptomatic/mild anemia (thalassemia minor) to
severe (thalassemia major), the latter requiring lifelong blood
transfusions. Stem cell transplantation is the sole curative treatment[3]
but is reserved for only the most severe cases as it is expensive and
requires a direct family donor; thus, blood transfusions and iron
chelation remain standard treatments. Between 2013-4, the Thalassemia
International Federation (TIF)[6,7] created two
classification guidelines for the management of transfusion-dependent
thalassemia (TDT) and non–transfusion-dependent thalassemia (NTDT).
While this has resulted in improvements, complications from disease and
treatment persist, especially regarding iron overload.
Children
and adolescents with chronic illnesses also experience apprehension
about physical health, effects on growth and puberty, body image,
school absences, and disruption of social activities. Health-related
quality of life (HRQoL) is a measure of how well patients can
participate in a lifestyle typical for their age.[8,9] Before TIF guidelines implementation, thalassemia patients reported suboptimal HRQoL, associated with disease severity.[10,11] The Pediatric Quality of Life Inventory 4.0 Generic Core Scales (PedsQL) is well known and easy to score.[12] Previous research in Thailand demonstrated that healthy children had significantly higher mean HRQoL scores[13] to chronically-ill ones in all PedsQLsubscales. The EuroQol Group's Five Dimensions for Youth (EQ-5D-Y)[14]
is another tool to evaluate child and adolescent HRQoL; the
questionnaire layout may be more child-friendly. Both instruments have
Thai versions with adequate reliability and validity.
While
there is a large global body of research on HRQoL for pediatric
thalassemia patients, not much has been done in Thailand. In
2015, a Thai study of adolescents with thalassemia reported higher
serum ferritin levels, and comorbidities were associated with lower
HRQoL.[15] We previously published a report from our hospital (2010) with 2008-9 data,[16]
using the PedsQL with 75 pediatric patients and found that family
finance and disease severity affected HRQoL outcomes. Somewhat
similarly, recent studies from Egypt and Sri Lanka noted comorbidities
(short stature, splenectomy, and undernutrition), transfusion
dependence, and lower patient and mother educational levels as
associated with lower HRQoL scores.[17,18]
As of
2019, our hospital has a broader patient demographic,
better-established treatment guidelines, and improved access to
pediatric endocrinology and cardiology staff. Our objectives were
to assess HRQoL among children and adolescents with thalassemia using
both the PedsQL and EQ-5D-Y and examine possible factors affecting
HRQoL. We also wanted to determine if improvements occurred in
thalassemia management that impacted HRQoL and observe outcome
discrepancies for TDT versus NTDT patients.
Methods and Materials
Participants.
The clinical and socioeconomic data of TDT and NTDT patients receiving
treatment at our institute, aged 2 - 18 years old, were collected from
outpatient records and patient files at the Pediatric Hematology
Clinic, Thammasat University Hospital from June 2019 to December
2019. Our study protocol was approved by the Human Ethics
Committee of Thammasat University No. 1 Faculty of Medicine; assent
and/or informed consent forms were obtained from patients > 7 years
old and all parents or guardians. Patients and parents/guardians who
did not speak or understand Thai adequately were excluded as were cases
with incomplete history or records.
Growth assessment.
Anthropometric measurements, including weight, height and body mass
index (BMI), were recorded. Z-scores or standard deviation (SD) scores
of BMI for age were calculated using WHO Anthro and AnthroPlus
software.[19,20] BMI Z-scores (BMIZ) < 2 standard
deviations (SD), > 1, and > 2 SD were categorized as underweight,
overweight, and obese, respectively.
Measurement of HRQoL.The
validated Thai versions of the PedsQL and the EQ-5D-Y questionnaires
were used to assess pediatric HRQoL. The corresponding user agreement
was signed with MAPI Research Institute, Lyon, France, prior to using
the PedsQL, and our research was registered at the EuroQol Research
Foundation for the EQ-5D-Y. Questionnaires were either completed
independently by parent proxies or patients as possible; for very young
patients, the questions were given as an interview and forms filled out
by research assistants.
The PedsQL has forms for different stages of development per age groups: 2 - 4, 5 - 7, 8 - 12, and 13 - 18 years.[8,9,12]
All forms have four sections on physical health (8 items), emotional
wellbeing (5), social interaction (5), and/or school (5). All this
makes up an 8-item physical health summary score (PHS) and a 15-item
psychosocial health summary score (PCHS). Parallel child self-reports
and parental proxy-reports were filled out for each age group, except
for children 2 - 4 years old, which had only parental proxies. Possible
responses to each item were coded 0 to 4, i.e., never to almost always.
The child self-report form for the 5 - 7 years old group has a
three-point scale instead of five: not at all, sometimes, and a lot.
For children 2 - 4 years old not attending kindergarten, daycare, etc.,
the school section was omitted; if these children were attending some
form of school, parent proxies had to complete only three items in this
section.
The EQ-5D-Y is a two-part tool
to be completed by all parents/guardians as well as children aged 8 -15
years old. We extended this tool to the age of 18 years, as recommended
by the original developer, in order to have only one EQ-5D version in
this study.[14,21] The first
section has five questions on "mobility" "looking after myself" "doing
usual activities" "having pain or discomfort," and "feeling worried,
sad or unhappy". There are three possible answers to each question: no
problem, some/moderate problem/s, a lot of/severe problem/s. In the
last section of the EQ-5D-Y, participants indicate the current level of
health on a visual analog scale (VAS) from 0 to 100, 100 being highest
or best.
Statistical analysis.
Data were expressed as mean (SD; the standard deviation of the mean),
range, or percentage (%). Differences in variables between groups were
analyzed by t-test, Mann-Whitney U test, or ANOVA for continuous
variables and by Chi-square or Fisher's Exact tests for categorical
variables as appropriate. Internal reliability was assessed with
Cronbach's alpha for summary and total scores of the PedsQL and
EQ-5D-Y. We used Pearson's or Spearman's rank correlation coefficients
as appropriate to examine the strength of the relations between
preference values. Univariate or multivariate stepwise linear
regression analysis was undertaken to identify independent predictors
of HRQoL. All analyses incorporated Microsoft Excel 2019 and SPSS for
Windows (Statistical Package for the Social Sciences version 17.0, SPSS
Inc., Chicago, IL, USA). All p-values were two-tailed: p < 0.05 was
considered statistically significant.
Results
We
had 150 patients with TDT and NTDT. All children and their guardians
(including 94 mothers, 35 fathers, 15 grandmothers, one grandfather,
and five other relatives) completed the PedsQL and EQ-5D-Y as
appropriate. All children > 8 years old completed the EQ-5D-Y (85
participants); 121 children > 5 years responded to the PedsQL, as
expected.
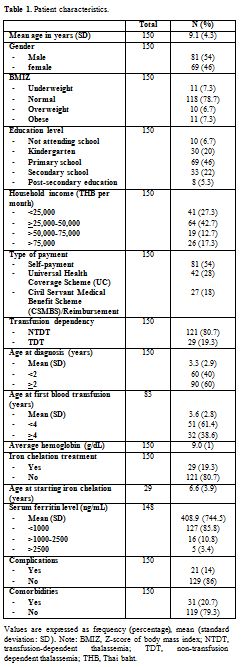
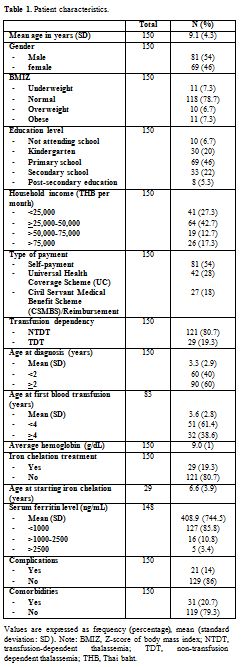
Patient characteristics. The demographic and clinical characteristics of all children are given in Table 1.
There was a mean age of 9.1 years (SD 4.3, range 2-18.8 years), with 81
males (54%). Most had normal nutritional status, i.e., normal BMIZ, and
were studying in primary school. Within the total, 3 had β thalassemia
major, 42 with β thalassemia/Hb E, 56 with Hb H disease (with/without
Hb Constant Spring [CS]/Hb Pakse [PS]), 25 with AE Bart's disease
(with/without Hb CS/Hb PS), 2 with EF Bart's disease (with/without Hb
CS), 16 with homozygous Hb E disease, and 6 having homozygous Hb CS
disease.
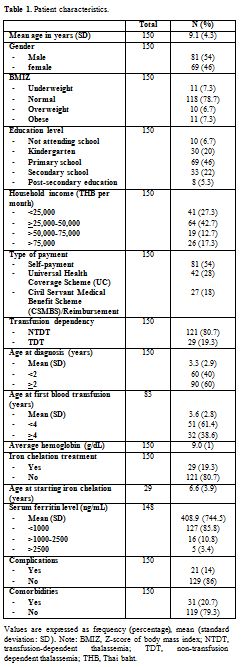 |
Table 1. Patient characteristics. |
Almost 20% (19.3%)
were TDT (three with β thalassemia major, 21 with β thalassemia/Hb E, 2
with Hb H disease, 3 with AE Bart's disease (with/without Hb CS/Hb PS),
all receiving iron chelation therapy regularly. Around 55% (55.17%) of
the patients (16/29) were receiving deferiprone (DFP), only one patient
receiving deferasirox (DFX), and 12/29 were receiving combination
therapy: eight with deferoxamine (DFO)+DFP and four with DFO+DFX.
The
mean age (SD) at diagnosis, at first blood transfusion, and at starting
iron chelation was 3.3 (2.9) years (range 0.1- 15 years), 3.6 (2.8)
years (range 0.1 - 15 years), and 6.6 (3.9) years (range 2-17.7 years),
respectively. Only 21 patients (14%) had complications, mostly
endocrinal diseases, including vitamin D deficiency (14 patients),
adrenal insufficiency (three), and short stature or growth failure
(three). Hypogonadism, hypothyroidism, or hypoparathyroidism was not
found in our participants. We screened for pulmonary hypertension
only in TDT, NTDT with iron overload, and splenectomy patients due to
hospital protocol; we had no cases of pulmonary hypertension. There was
one case of gallstones. In the 20.7% of total patients with some sort
of comorbidity, 45.2% suffered from allergic diseases, including seven
cases of allergic rhinitis, four cases of asthma, and three cases of
asthma with allergic rhinitis (data not shown).
HRQoL scores comparisons and correlations.
The reliability of the PedsQL and EQ-5D-Y was very acceptable with
Cronbach's alpha values > 0.7 (0.925 and 0.863, respectively).
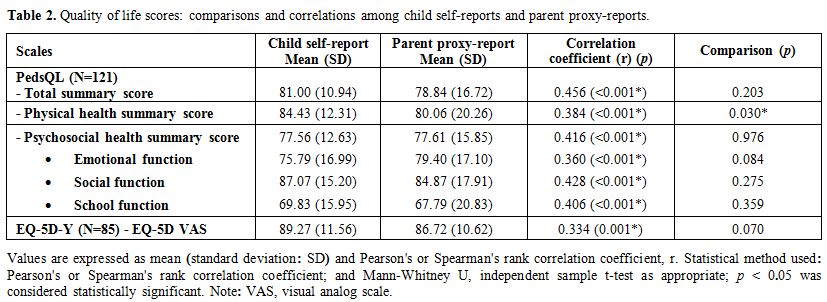
All mean (SD) scores for PedsQL and EQ-5D-Y self-reports, as well as
proxy-reports, are seen in Table 2.
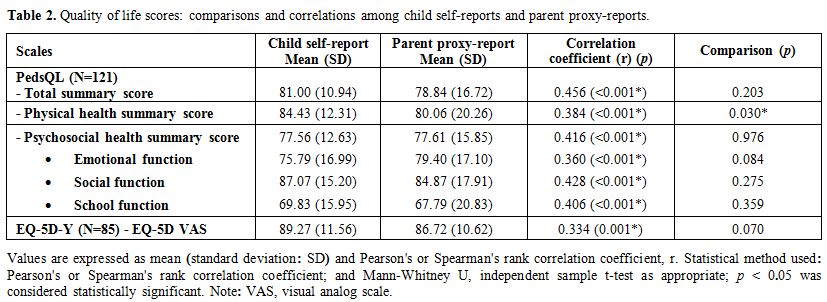 |
Table
2. Quality of life scores: comparisons and correlations among child self-reports and parent proxy-reports. |
Quality of life
scores were shown to have significant correlations between child self
and parental proxy reports for both PedsQL and EQ-5D-Y. For mean
PedsQL scores (SD), children's self-reports were slightly higher than
parental proxies for two categories: total summary score (TSS) and PHS;
only PHS was significantly different (p
= 0.030), the others not being statistically significant. PCHS child
and parental proxy reports were practically identical. EQ-5D-Y VAS
showed a statistically significant correlation with the PedsQL TSS of
both self-reports and proxy-reports: (r = 0.344, p = 0.001 and r = 0.271, p
= 0.001, respectively). In addition, the EQ-5D-Y dimensions revealed
statistically significant correlations with the PedsQL of both
self-reports and proxy-reports. Significant relationships were found
between the EQ-5D-Y dimensions of "mobility" "looking after myself" and
"doing usual activities" with PedsQL PHS scores (r = -0.220 and -0.171;
-0.477 and -0.138; -0.401 and -0.183: for self- and proxy-reports,
respectively). Moderate correlations were also seen between the EQ-5D-Y
dimensions of "having pain or discomfort" and "feeling worried, sad or
unhappy" with the PedsQL PCHS scores (r = -0.271 and -0.254; -0.381 and
-0.274: for self- and proxy-report, respectively). Please see Supplementary Table 1.
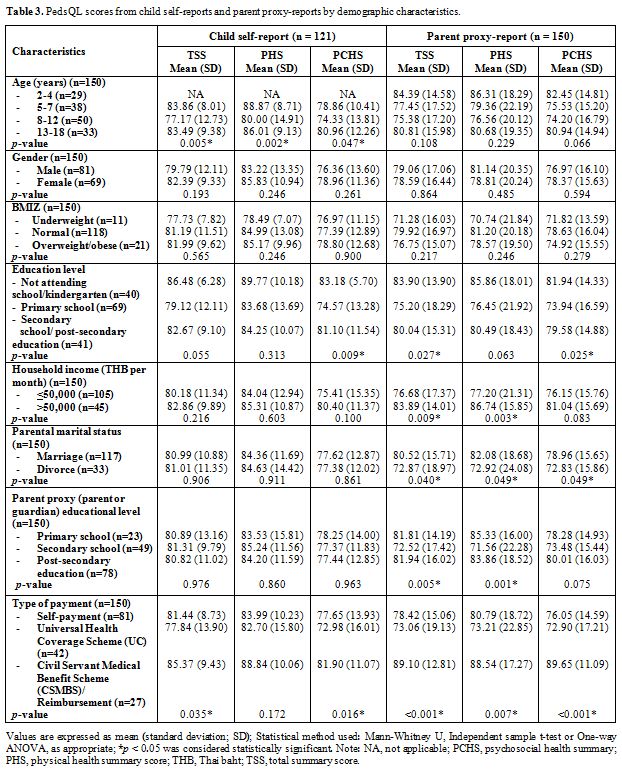
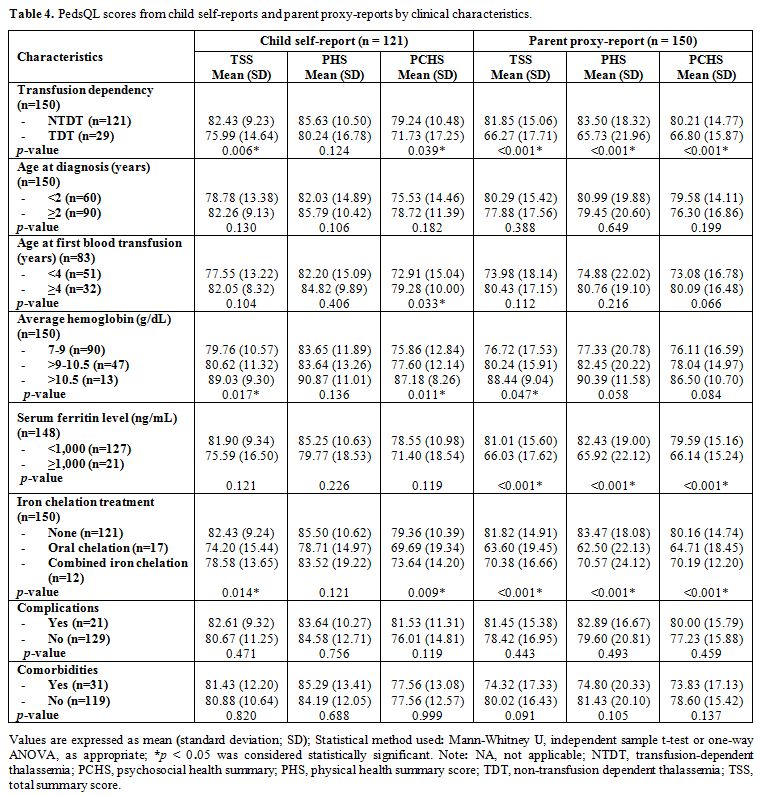
HRQoL scores and related factors. PedsQL child self-report and parent proxy-report scores along with patient demographic and clinical characteristics are in Table 3 and 4. Age group and type of payment demonstrated significant differences within self-reported TSS (p
= 0.005 and 0.035). For parental proxy reports, child education level,
parental marital status, household income, parent proxy education, and
type of payment revealed significant differences in TSS (p = 0.027, 0.040, 0.009, 0.005 and < 0.001, respectively) in Table 3. Being TDT or NTDT, average Hb, and having iron-chelation therapy were all significantly related to self-reported TSS (p = 0.006, 0.017, and 0.014, respectively), as indicated in Table 4.
In addition, transfusion dependency, average Hb, ferritin level and
iron-chelation therapy were also associated with parental proxy TSS (p = < 0.001, 0.047, < 0.001, and < 0.001, respectively); these patients typically had lower self-assessed HRQoL scores.
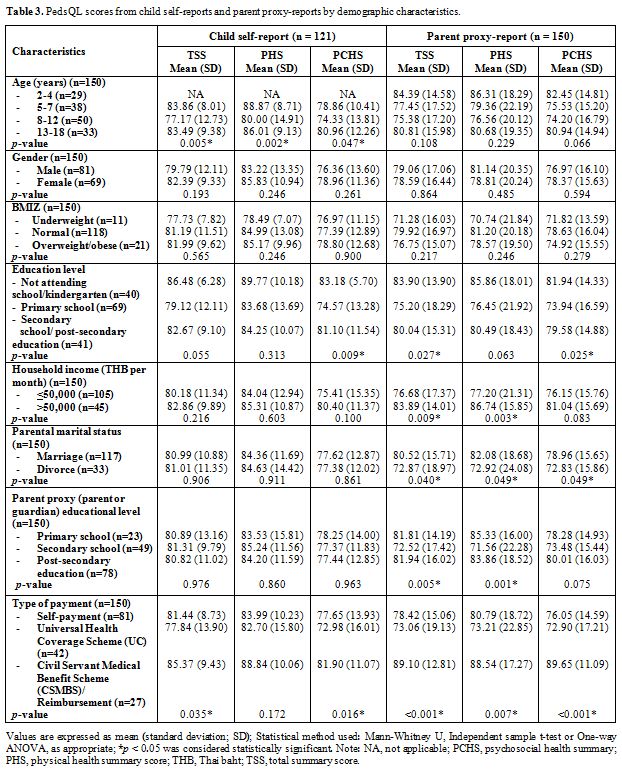 |
Table 3. PedsQL scores from child self-reports and parent proxy-reports by demographic characteristics. |
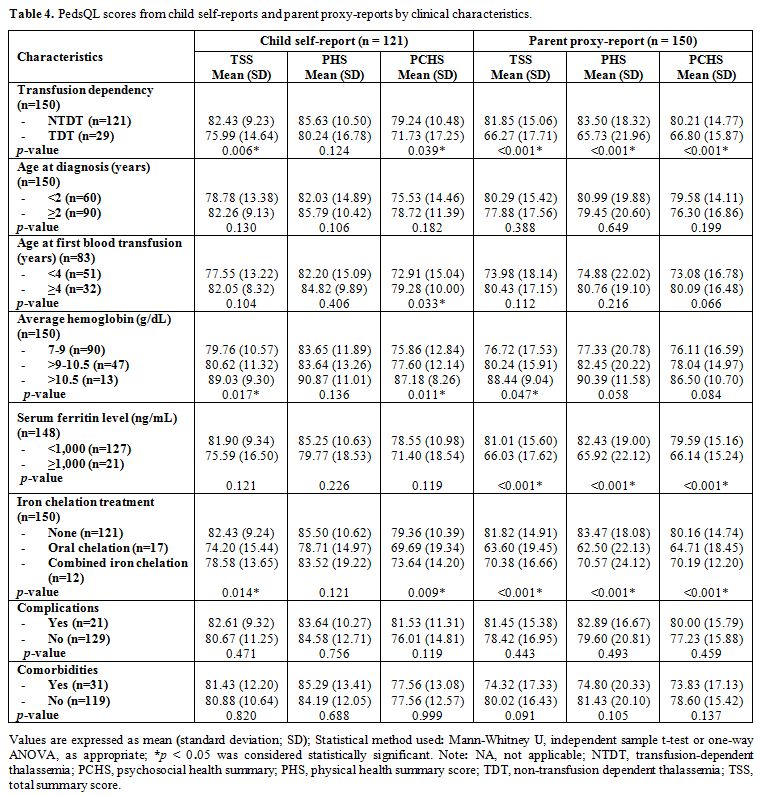 |
Table 4. PedsQL scores from child self-reports and parent proxy-reports by clinical characteristics. |
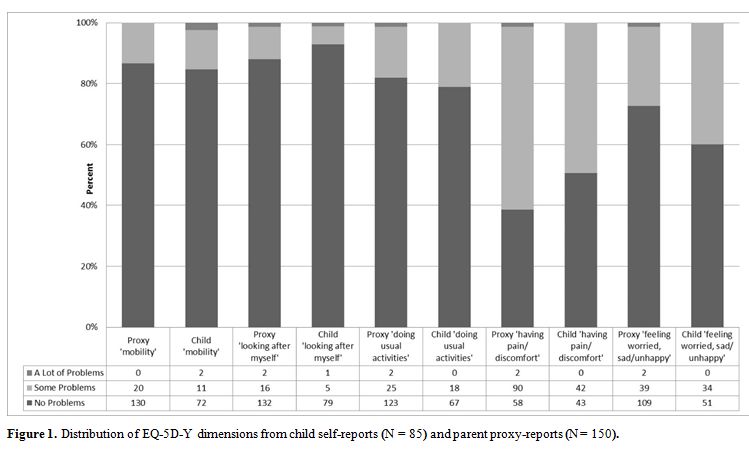
Figure 1
shows proxy and self-report EQ-5D-Y dimensions. Having some or many
problems in "suffering pain or discomfort" (49.4% child report and
61.3% parental proxy) and "feeling worried, sad or unhappy" (40% child
and 27.3% parental proxy) was reported more often than for "doing usual
activities" (21.2% child and 18% parental proxy) and "mobility" (15.3%
and 13.3%). "Looking after myself" seemed to pose the least difficulty:
7.1% and 12%. Mobility was the sole area with more problems for TDT
patients versus NTDT from parental proxy perspectives (p
= 0.004) (data not shown). Significant differences were seen in
parental proxy reports for EQ-5D-Y VAS regarding the type of payment
and serum ferritin levels. Those using any reimbursement and patients
with lower ferritin levels had higher EQ-5D-Y VAS compared to those
with self-payment or under UC coverage with higher ferritin levels (p = 0.026 and 0.031) (data not shown).
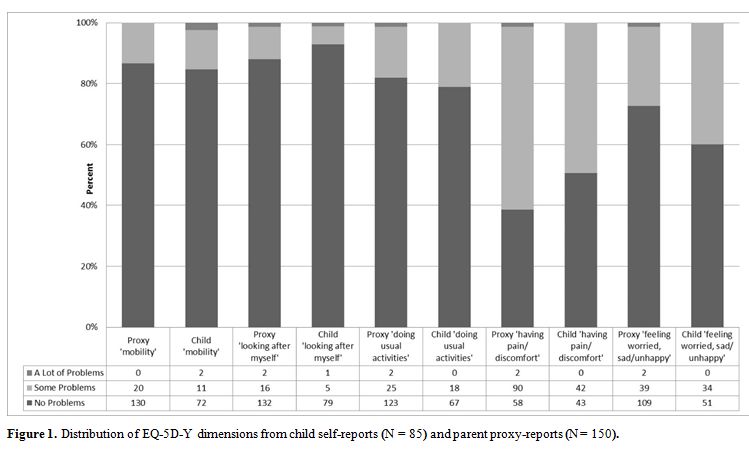 |
Figure 1. .Distribution of EQ-5D-Y dimensions from child self-reports (N = 85) and parent proxy-reports (N = 150). |
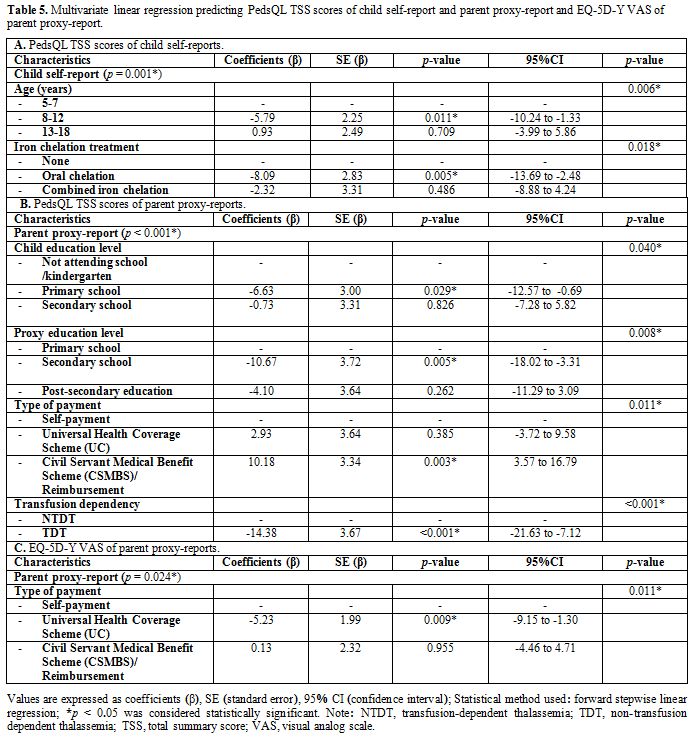
Linear regression analysis for predictors of HRQoL scores.
Using a forward stepwise linear regression method for our final model,
age group and iron chelation treatment were independently associated
with child self-report PedsQL TSS (R2 = 0.118, p = 0.001) (Table 5A). An age of 8-12 years negatively predicted PedsQL TSS versus one of 5 - 7 years (p = 0.011). Oral chelation therapy reduced PedsQL TSS significantly as compared to those having no iron chelation (p = 0.005). The same regression model examined factors affecting PedsQL TSS for parental proxy-reports: Table 5B.
This TSS was predicted by children's education, proxy education, type of payment, and TDT (R = 0.239, p
< 0.001). Primary school children appeared to experience negative
impacts, according to their parents/guardians, as opposed to those not
attending school or in kindergarten (p
= 0.029). Parent proxies with a secondary school education seemed to
have lower TSS compared to parents/guardians with less education (p =
0.005). Parental proxy reports of TDT patients displayed poorer TSS
than those children with NTDT (p < 0.001). Interestingly, there was a positive relationship between TSS and medical payment by
Civil Servant Medical Benefit Scheme (CSMBS) or any reimbursement scheme versus self-payment (p = 0.003). UC negatively predicted parental proxy EQ-5D-Y VAS in comparison with self-payment (p = 0.009) (R = 0.037, p = 0.024) (Table 5C).
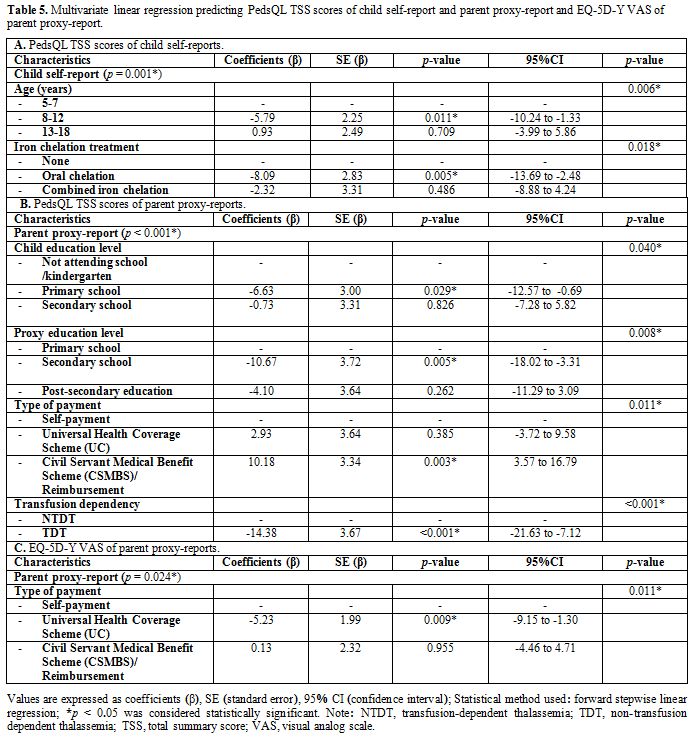 |
Table 5. Multivariate
linear regression predicting PedsQL TSS scores of child self-report and
parent proxy-report and EQ-5D-Y VAS of parent proxy-report. |
Discussion
In
this single-institution study of HRQoL in Thai children with
thalassemia, we compared the unique perspectives of children and their
parent proxies from two discrete instruments: PedsQL and EQ-5D-Y.
A wealth of research using PedsQL in pediatric patients with
thalassemia[10,15-18] generally
shows it to be a reliable and valid tool for healthy and
chronically-ill children. While the EQ-5D-Y has also been used in
chronic illness, we could not find any reports of it for children with
thalassemia; our study may be the first. Two other studies have
examined children with thalassemia using different versions: EQ-5D and
EQ-5D-3L.[22,23]
EQ-5D-Y appears to have some
favorable attributes: the questionnaire is relatively quick and
straightforward for participants to complete and appropriately
comprehensible for each cognitive-developmental stage.[14,24,25]
However, we should also note that the EQ-5D-Y does not cover some
aspects of child HRQoL, such as some psychometric properties and family
relationships, which are covered by other generic instruments like
PedsQL.[26] In addition, the EQ-5D-Y can be used with
confidence in acutely-ill children but has not been as good in chronic
disorders or healthy children.[27] This study supported that EQ-5D-Y was proper to assess in chronically-ill children, like thalassemia, rapidly.
In
place of any existing research with pediatric thalassemia, we compared
our patients' EQ-5D-Y dimensions with studies on children having a
different chronic illness such as cystic fibrosis in Germany, diabetes
mellitus in Spain, and chronic kidney disease in Taiwan.[28-30]
Our thalassemia patients reported more difficulties in pain/discomfort
and anxiety/depression as compared to their usual activities, mobility,
and self-care; this mirrored the previous research. It might be assumed
that the children experience more psychosocial challenges versus
physical hindrances. Further research needs to be done using EQ-5D-Y
with pediatric thalassemia patients in other settings and certainly
over the long term.
The study demonstrated both EQ-5D-Y VAS and
dimensions had statistically significant correlations with the PedsQL
TSS, PHS, and PCHS, particularly of both child and parent proxy
reports. Parental proxy scores were also in line with the children's
from both PedsQL and EQ-5D-Y and which is consistent with our prior
research using PedsQL[16,31,32] solely. In other research,[15,16,33]
parent proxy-rated HRQoL scores were typically lower than child-rated
ones. Notably, for us, only the PHS for parent proxy-rated PedsQL was
significantly lower (p =
0.030); our TSS were slightly lower but not significantly. Regarding
this lower TSS, we can speculate parent proxies may be more concerned
about the current and future effects of their child's physical
disability, i.e., financial burdens, social interactions, etc., than
these young children are at present. However, for the significantly
lower PHS, parents/guardians may be merely relying on what they can
observe of their child's suffering. This topic could be useful to
explore in future research. Children rated their psychosocial health
lower than their physical health in the PedsQL, particularly for the
scholarly function; this also matches several past studies.[10,15-18,24]
Perhaps this is due to frequent school absences, restrictions within
social activities at school, physical pain from medical procedures such
as venipuncture, intravenous access for transfusion, or injection, or
even lower self-esteem.
We were pleasantly surprised that all of
our current parental proxy and self-reported HRQoL scores were
noticeably higher when compared to a decade-old report that was written
pre-implementation of the TIF guidelines, from our hospital.[16]
It is hoped this is a result of consistent improvements in medical care
over the last ten years, but it may also reflect a broader social
acceptance of chronic illnesses and other external changes. The
implementation of the TIF guidelines toward improving thalassemia care
management at our hospital, better subspecialty pediatric care, and
greater availability of oral iron chelation drugs may have raised HRQoL
scores. Better health care is likely to have resulted in less pain and
discomfort for patients and improved social interactions and
functions. One important point may be the ability to have
subcutaneous administration equipment at home in cases requiring
combined iron chelation. Although the procedure remains physically
uncomfortable, it may be more convenient for children and
parents/guardians to have this take place in the home.
It
must be noted that our lower ratio of TDT versus NTDT, 1/5 of the
patients in this paper as compared to 1/3 in the past, may have
resulted in higher HRQoL than previously. While it may merely be that
patients are happier because their disease is less severe, this finding
requires further examination as we had twice the number of participants
here: 150 versus the 75 before. This lower proportion of TDT may
be the longer-term outcomes of the national screening policy for severe
types of thalassemia, coupled with the better general social awareness
of thalassemia and its effects.
This study examined predictors
of HRQoL using stepwise linear regression from both PedsQL and EQ-5D-Y
VAS. For the PedsQL, age was significantly associated with HRQoL
according to children's self-report data, similar to prior reports.[10,34]
Patients 8-12 years old had lower HRQoL, leading to us to see this age
group as a negative predictor. As this age group often experiences a
transition from preschool to elementary school, they may be worried
about their learning ability or school absences. As they grow older,
children naturally become more aware of any differences from their
peers.
For our patients, iron chelation therapy, particularly
oral chelation, significantly and negatively impacted HRQoL. Leafy MS
et al.[35] observed all patients experienced burden with chelation, no matter which type. Similarly, Thavorncharoensap et al.[10]
stated that iron chelation treatment was associated with poorer
HRQOL.Three other studies found that patients using oral chelators,
especially deferasirox, had a better quality of life versus those using
injectable forms.[22,36,37]
However, we must state that these findings may differ from ours due to
the particular breakdown of our chelation patients. First of all, only
29/150 of our patients received any kind of chelation therapy (Table 4), which is relatively low. Of these 29 patients, 17 used oral chelation, and 12 used combined oral/injection.
Moreover,
most of our patients use deferiprone versus deferasirox as it is
cheaper and more accessible in Thailand. We imagine that any
patients taking oral chelation already are experiencing iron overload
and more likely to develop complications related to this; thus, they
would have a worse quality of life in relation to more severe disease.
Medications' side effects and the burden of compliance would likely be
factors to explore further.
Parental proxy-reports for PedsQL
outlined some unique and significant associations with
HRQoL: child education, proxy education, type of payment, and
transfusion dependency. Similar to the self-reports, parents/guardians
also believed that primary school children had lower HRQoL. Caregivers
may be concerned about both social integration and school performance
at this age. Furthermore, our results seemed to show that parental
proxy education at the secondary school level was significantly
correlated with lower perceived children's HRQoL; university education
was as well but not significantly. A subgroup analysis of the impact of
parental education on HRQoL (N=129: 94 mothers and 35 fathers) also
revealed a concordance in which parents with secondary school
completion had the lowest PedsQL TSS (p
= 0.037, data not shown). Our datum does not appear to concur
with an Egyptian and Iraqi paper that reported high levels of parental
education were associated with higher HRQoL outcomes.[18,32,36]
It is only speculation at this point, but perhaps caregivers who
completed secondary school in Thailand are more anxious about the
challenges their children might face, or this might merely be a
cultural difference. Thailand people with less education could be more
inclined to trust the public health care system, whereas those with
more education may be prone to have more doubt as they may have access
to alternatives. This tendency should be further explored by an
in-depth interview study.
Family economic status appeared to play
a significant role in the PedsQL measurement of HRQoL, similar to the
previous Thai study.[16] For example, CSMBS/any
reimbursement system had positive impacts on parental proxy
perspectives. Probably, the type of payment is, in itself, a proxy for
familial disposable income and access to financial assets. Besides,
CSMBS and the other reimbursement schemes offer a wider variety of
treatment choices and convenience. This is especially relevant for the
location of treatment, as people under UC are obligated to seek care in
the region where they were registered, and sometimes families work and
live elsewhere. Indeed, parental proxy reports showed that the
Use of UC negatively predicted the EQ-5D-Y VAS, in comparison with
self-payment.
Overall, all PedsQL scores, both parental and
child proxies, were lower for children who were TDT. Unsurprisingly,
parent proxies of children with TDT reported significantly lower TSS
than NTDT parent proxies, after using multivariate linear regression.
This finding is in line with prior research[10,16,18]
and is likely because of disease severity along with the inconvenience
and perceived distress during treatment, as mentioned before. However,
another Thai study[15] in teenagers with thalassemia
reported no differences in PedsQL scores between TDT and NTDT; this
latter paper had a higher amount of TDT patients. The differing scores
may be a result of attitude changes with age.
The most critical
limitation in our study is the absence of a control group of healthy
children. It would be useful to repeat this work incorporating healthy
controls with the EQ-5D-Y, to see if the results still stand, along
with the PedsQL.The EQ-5D-Y may indeed be appropriate for children with
thalassemia; however, this is unknown at this point as we have no other
research to compare it with. It certainly would be appropriate to
repeat this study in five or ten years and see if scores improve or
reduce in line with public policy and health care access. A higher
number of participants, along with data from other centers, would also
give a clearer picture of HRQoL.
Conclusions
This
is the first study attempting to use the EQ-5D-Y with Thai pediatric
thalassemia patients, comparing EQ-5D-Y and PedsQL scores from parent
proxies and children. Within our limited data, it appears the EQ-5D-Y
might be useful for measuring the quality of life in these children.
Predictors of lower HRQoL scores, according to self-report, included
the age of 8 - 12 years and oral chelation. Parental proxy-report
predictors of lower scores were primary school education for children,
secondary school parental proxy education, UC healthcare payment, and
transfusion dependency. Overall, HRQoL scores were higher from our
institution's report ten years ago; this may be due to better
management guidelines as well as a better standard of care, including
access to more specialists. Further long-term research needs to take
place, especially to improve the quality of life for TDT
patients.
Acknowledgments
The
authors wish to thank the MAPI Research Institute and the EuroQoL for
allowing the Use of the PedsQL and the EQ-5D-Y instruments. We would
also express our gratitude to all patients and their parents/guardians
for their participation, Associate Professor Dr. Wallee Satayasai and
Dr. Tasama Pusongchai for recruiting participants and their valuable
support, and Professor Dr. Paskorn Sritipsukho for his contribution to
the statistical analysis consultation. We would like to thank the
Center of Excellence in Applied Epidemiology for supporting. The
English language editing was done by Debra Kim Liwiski, international
instructor, Clinical Research Center, Faculty of Medicine, Thammasat
University. The authors gratefully acknowledge the financial support
provided by Faculty of Medicine, Thammasat University, contract:
K.10/2562.
References
- Weatherall DJ, Clegg JB, eds. The Thalassaemia Syndromes. 4th ed. Oxford: Blackwell Science; 2001. https://doi.org/10.1002/9780470696705
- Weatherall
DJ. The inherited diseases of hemoglobin are an emerging global health
burden. Blood. 2010;115(22):4331-6.
https://doi.org/10.1182/blood-2010-01-251348 PMid:20233970
PMCid:PMC2881491
- Taher AT, Weatherall DJ, Cappellini MD. Thalassaemia. Lancet. 2018;391(10116):155-67. https://doi.org/10.1016/S0140-6736(17)31822-6
- Chaibunruang
A, Sornkayasit K, Chewasateanchai M, Sanugul P, Fucharoen G, Fucharoen
S. Prevalence of Thalassemia among Newborns: A Re-visited after 20
Years of a Prevention and Control Program in Northeast Thailand.
Mediterr J Hematol Infect Dis. 2018; 10(1): e2018054. https://doi.org/10.4084/mjhid.2018.054 PMid:30210747 PMCid:PMC6131105
- Fucharoen
S, Winichagoon P. Thalassemia in Southeast Asia: problems and strategy
for prevention and control. Southeast Asian J Trop Med Public Health.
1992;23:647-55.
- Cappellini MD, Cohen A,
Porter J, Taher A, Viprakasit V, editors. Guidelines for the management
of transfusion dependent thalassaemia (TDT). 3rd edition. Nicosia
(Cyprus): Thalassaemia International Federation; 2014.
- Taher
A, Vichinsky E, Musallam K, Cappellini MD, Viprakasit V, editors.
Guidelines for the management of non-transfusion dependent thalassaemia
(NTDT). Nicosia (Cyprus): Thalassaemia International Federation; 2013.
- Varni
JW, Limbers CA. The pediatric quality of life inventory: measuring
pediatric health-related quality of life from the perspective of
children and their parents. Pediatr Clin North Am. 2009;56(4):843-63. https://doi.org/10.1016/j.pcl.2009.05.016 PMid:19660631
- Matza
LS, Swensen AR, Flood EM, Secnik K, Leidy NK. Assessment of
health-related quality of life in children: a review of conceptual,
methodological, and regulatory issues. Value Health. 2004;7(1):79-92. https://doi.org/10.1111/j.1524-4733.2004.71273.x PMid:14720133
- Thavorncharoensap
M, Torcharus K, Nuchprayoon I, Riewpaiboon A, Indaratna K, Ubol BO.
Factors affecting health-related quality of life in Thai children with
thalassemia. BMC Blood Disord. 2010;10:1-10. https://doi.org/10.1186/1471-2326-10-1 PMid:20180983 PMCid:PMC2836992
- Pakbaz
Z, Treadwell M, Yamashita R, Quirolo K, Foote D, Quill L, Singer T,
Vichinsky EP. Quality of life in patients with thalassemia intermedia
compared to thalassemia major. Ann N Y Acad Sci. 2005;1054:457-61. https://doi.org/10.1196/annals.1345.059 PMid:16339697
- Varni
JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the
Pediatric Quality of Life Inventory version 4.0 generic core scales in
healthy and patient populations. Med Care. 2001 Aug;39(8):800-12. https://doi.org/10.1097/00005650-200108000-00006 PMid:11468499
- Sritipsukho
P, Wisai M, Thavorncharoensap M. Reliability and validity of the Thai
version of the Pediatric Quality of Life Inventory 4.0. Qual Life Res.
2013;22(3):551-7. https://doi.org/10.1007/s11136-012-0190-y PMid:22552603
- Wille
N, Badia X, Bonsel G, Burstrom K, Cavrini G, Devlin N, et al.
Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual
Life Res. 2010; 19(6): 875-886. https://doi.org/10.1007/s11136-010-9648-y PMid:20405245 PMCid:PMC2892611
- Boonchooduang
N, Louthrenoo O, Choeyprasert W, Charoenkwan P. Health-related quality
of life in adolescents with thalassemia. Pediatr Hematol Oncol.
2015;32(5):341-8. https://doi.org/10.3109/08880018.2015.1033795 PMid:26086564
- Surapolchai
P, Satayasai W, Sinlapamongkolkul P, Udomsubpayakul U. Biopsychosocial
predictors of health-related quality of life in children with
thalassemia in Thammasat University Hospital. J Med Assoc Thai. 2010;93
Suppl 7:S65-75.
- Mettananda S, Pathiraja
H, Peiris R, Bandara D, Silva U, Mettananda C. Health related quality
of life among children with transfusion dependent β-thalassaemia major
and haemoglobin E β-thalassaemia in Sri Lanka: a case control study.
Health Qual Life Outcomes. 2019; 17: 137. https://doi.org/10.1186/s12955-019-1207-9 PMid:31395066 PMCid:PMC6686351
- Adam
S, Afifi H, Thomas M, Magdy P, El-Kamah G. Quality of life outcomes in
a pediatric thalassemia population in Egypt. Hemoglobin.
2017;41(1):16-20. https://doi.org/10.1080/03630269.2017.1312434 PMid:28440111
- World
Health Organization. WHO Anthro for personal computers, version 3.2.2,
2011: Software for assessing growth and development of the world's
children. Geneva: WHO, 2010. Available at: https://www.who.int/childgrowth/software/en/. Accessed: January 30, 2020.
- World
Health Organization. WHO AnthroPlus for personal computers manual:
software for assessing growth of the world's children and adolescents.
Geneva: WHO; 2009. Available at: https://www.who.int/growthref/tools/en/. Accessed: January 30, 2020.
- EuroQol Group. EQ-5D-Y User Guide.: Basic information on how to use the EQ-5D-Y instrument. Available at: http://www.euroqol.org/fileadmin/user_upload/Documenten/PDF/Folders_Flyers/EQ-5D-Y_User_Guide_v1.0_2014.pdf. Accessed: May 5, 2020.
- Seyedifar
M, Dorkoosh FA, Hamidieh AA, Naderi M, Karami H, Karimi M, Fadaiyrayeny
M, Musavi M, Safaei S, Ahmadian-Attari MM, Hadjibabaie M, Cheraghali
AM, Akbari Sari A. Health-related quality of life and health utility
values in beta thalassemia major patients receiving different types of
iron chelators in Iran. Int J Hematol Oncol Stem Cell Res.
2016;10(4):224-31.
- Shaligram D, Girimaji
SC, Chaturvedi SK. Psychological problems and quality of life in
children with thalassemia. Indian J Pediatr. 2007;74(8):727-30. https://doi.org/10.1007/s12098-007-0127-6 PMid:17785893
- Burström
K, Bartonek A, Broström EW, Sun S, Egmar C. EQ-5D-Y as a health-related
quality of life measure in children and adolescents with functional
disability in Sweden: testing feasibility and validity. Acta Paediatr.
2014;103(4):426-35. https://doi.org/10.1111/apa.12557 PMid:24761459
- Kreimeier
S, Greiner W. EQ-5D-Y as a health-related quality of life instrument
for children and adolescents: The instrument's characteristics,
development, current Use, and challenges of developing its value set.
Value Health. 2019;22(1):31-37. https://doi.org/10.1016/j.jval.2018.11.001 PMid:30661631
- Noyes
J, Edwards RT. EQ-5D for the assessment of health-related quality of
life and resource allocation in children: a systematic methodological
review. Value Health. 2011;14(8):1117-29. https://doi.org/10.1016/j.jval.2011.07.011 PMid:22152182
- Scott
D, Ferguson GD, Jelsma J. The Use of the EQ-5D-Y health related quality
of life outcome measure in children in the Western Cape, South Africa:
psychometric properties, feasibility and usefulness - a longitudinal,
analytical study. Health Qual Life Outcomes. 2017;15(1):12. https://doi.org/10.1186/s12955-017-0590-3 PMid:28103872 PMCid:PMC5248508
- Eidt-Koch
D, Mittendorf T, Greiner W. Cross-sectional validity of the EQ-5D-Y as
a generic health outcome instrument in children and adolescents with
cystic fibrosis in Germany. BMC Pediatr. 2009; 9: 55. https://doi.org/10.1186/1471-2431-9-55 PMid:19715563 PMCid:PMC2753333
- Mayoral
K, Rajmil L, Murillo M, Garin O, Pont A, Alonso J, Bel J, Perez J,
Corripio R, Carreras G, Herrero J, Mengibar JM, Rodriguez-Arjona D,
Ulrike Ravens-Sieberer U, Raat H, Serra-Sutton V, Ferre Mr. Measurement
properties of the online EuroQol-5D-Youth instrument in children and
adolescents with type 1 diabetes mellitus: questionnaire study. Med
Internet Res. 2019; 21(11): e14947. https://doi.org/10.2196/14947 PMid:31714252 PMCid:PMC6880238
- Hsu
CN, Lin HW, Pickard AS, Tain YL. EQ-5D-Y for the assessment of
health-related quality of life among Taiwanese youth with
mild-to-moderate chronic kidney disease. Int J Qual Health Care.
2018;30(4):298-305. https://doi.org/10.1093/intqhc/mzy011 PMid:29447362
- Varni
JW, Limbers CA, Burwinkle TM. How young can children reliably and
validly self-report their health-related quality of life? An analysis
of 8,591 children across age subgroups with the PedsQL™ 4.0 Generic
Core Scales. Health Qual Life Outcomes. 2007;5: 1. https://doi.org/10.1186/1477-7525-5-1 PMid:17201920 PMCid:PMC1769360
- Mikael
NA, Al-Allawi NA. Factors affecting quality of life in children and
adolescents with thalassemia in Iraqi Kurdistan. Saudi Med J.
2018;39(8):799-807 https://doi.org/10.15537/smj.2018.8.23315 PMid:30106418 PMCid:PMC6194984
- Caocci
G, Efficace F, Ciotti F, Roncarolo MG, Vacca A, Piras E, Littera R,
Markous RSD, Collins GS, Ciceri F, Mandelli F, Marktel S, Nasa GL.
Health related quality of life in Middle Eastern children with
beta-thalassemia. BMC Blood Disord. 2012;12:6. https://doi.org/10.1186/1471-2326-12-6 PMid:22726530 PMCid:PMC3496588
- Ismail
A, Campbell MJ, Ibrahim HM, Jones GL. Health related quality of life in
Malaysian children with thalassaemia. Health Qual Life Outcomes.
2006;4:39. https://doi.org/10.1186/1477-7525-4-39 PMid:16813662 PMCid:PMC1538578
- Elalfy
MS, Massoud W, Elsherif NH, Labib JH, Elalfy OM, Elaasar S, von
Mackensen S. A new tool for the assessment of satisfaction with iron
chelation therapy (ICT-Sat) for patients with β-thalassemia major.
Pediatr Blood Cancer. 2012;58(6):910-5. https://doi.org/10.1002/pbc.23413 PMid:22232075
- Abdul-Zahra
HA, Hassan MK, Ahmed BA. Health-related quality of life in children and
adolescents with β-thalassemia major on different iron chelators in
Basra, Iraq. J Pediatr Hematol Oncol. 2016;38(7):503-11. https://doi.org/10.1097/MPH.0000000000000663 PMid:27606437
- Goulas
V, Kourakli-Symeonidis A, Camoutsis C. Comparative Effects of Three
Iron Chelation Therapies on the Quality of Life of Greek Patients with
Homozygous Transfusion-Dependent Beta-Thalassemia. ISRN Hematol. 2012;
2012: 139862. https://doi.org/10.5402/2012/139862 PMid:23316378 PMCid:PMC3534333
Supplementary Table
 |
Supplementary Table 1.
Correlations between PedsQL and EQ-5D-Y dimensions and VAS among child
self-reports and parent proxy-reports. |
[TOP]