Materials and methods
Study setting.
Patients included in this study were from the Kurdistan Region,
Northern Iraq. The region borders on Turkey and Iran, which both have
COVID-19 epidemics. This region, which comprises four cities: Erbil,
Duhok Sulaymaniyah, and Halabja, has a total population of
5,816,000. A COVID center has been established in each city for the
management and treatment of confirmed cases. As a national program, all
data regarding COVID-19 are published and updated daily through the
COVID-19 information center, a Regional Government of Kurdistan website.
Patients. Patients were defined as any individual with a positive SARS-CoV-2 polymerase chain reaction (PCR) test result regardless of the presence of symptoms. The PCR test was conducted in duplicate. A suspected patient was defined as an individual with acute respiratory illness who had either traveled to an area with person-to-person transmission of SARS-CoV-2 or had close contact with a confirmed case within 14 days before symptom onset. Individuals who returned from abroad or been in contact with confirmed cases were quarantined.
Quarantine was defined as confining individuals in a dedicated facility. In quarantine, patients were examined clinically for signs and symptoms of COVID-19. Patients were tested by PCR at the beginning and the end of the quarantine period. On discharge from hospital or quarantine centers, they were instructed to remain in quarantine in their homes for a further14 days.
Treatment. All patients received two doses of oral hydroxychloroquine 400 mg on the first day, then 200 mg twice a day, and 75 mg oral oseltamivir twice a day for the duration of their stay in the COVID center. Some patients were prescribed antibiotics or other medications as needed. Recovery was defined as the disappearance of symptoms with negative SARS-CoV-2 reverse transcription (RT)-PCR results. Patients admitted to COVID centers were tested using RT-PCR twice a week. If the test was negative, it was repeated after 24 hours. Patients were considered cured when two RT-PCR results on two consecutive days were negative. The significance of differences between confirmed, recovered, and death cases were determined by Chi-square and Fisher’s exact tests. P values of < 0.05 were considered statistically significant.
Ethical approval was obtained from the ethics committee in the College of Medicine, University of Zakho.
Patients. Patients were defined as any individual with a positive SARS-CoV-2 polymerase chain reaction (PCR) test result regardless of the presence of symptoms. The PCR test was conducted in duplicate. A suspected patient was defined as an individual with acute respiratory illness who had either traveled to an area with person-to-person transmission of SARS-CoV-2 or had close contact with a confirmed case within 14 days before symptom onset. Individuals who returned from abroad or been in contact with confirmed cases were quarantined.
Quarantine was defined as confining individuals in a dedicated facility. In quarantine, patients were examined clinically for signs and symptoms of COVID-19. Patients were tested by PCR at the beginning and the end of the quarantine period. On discharge from hospital or quarantine centers, they were instructed to remain in quarantine in their homes for a further14 days.
Treatment. All patients received two doses of oral hydroxychloroquine 400 mg on the first day, then 200 mg twice a day, and 75 mg oral oseltamivir twice a day for the duration of their stay in the COVID center. Some patients were prescribed antibiotics or other medications as needed. Recovery was defined as the disappearance of symptoms with negative SARS-CoV-2 reverse transcription (RT)-PCR results. Patients admitted to COVID centers were tested using RT-PCR twice a week. If the test was negative, it was repeated after 24 hours. Patients were considered cured when two RT-PCR results on two consecutive days were negative. The significance of differences between confirmed, recovered, and death cases were determined by Chi-square and Fisher’s exact tests. P values of < 0.05 were considered statistically significant.
Ethical approval was obtained from the ethics committee in the College of Medicine, University of Zakho.
Results
Patients.
In the Kurdistan Region, 64591 people were tested for SARS-CoV-2 using
RT-PCR up to May 21, of whom 452 (0.7%) were positive. The patient
characteristics are shown in Table 1.
The majority of cases were diagnosed in two cities: Erbil and
Sulaymaniyah (Of the patients, 49.1% were male, and 88.9% were below
the age of 60 years (Table 1).
The majority (80%) were asymptomatic. The most common symptoms were
fever, dry cough, and shortness of breath. The time to recovery ranged
from 7 to 32 days. The criteria for severity of COVID-19 were defined
according to The Official Chinese Government Guide to Diagnosing and
Treating the Novel Coronavirus (7th version).[2]
Case Distribution. Following the diagnosis of the first case on March 1, 2020, there was a steady increase in the number of cases. The highest rate of infection was recorded in Erbil (Table 2). The highest number of patients was recorded (44 patients) on April 6, 2020. These patients were interviewed, and it was discovered that they had all attended a funeral, which was forbidden under the social distancing rules that were in place. Case tracing led to the diagnosis of 129 funeral-related cases in Erbil city.
Case fatality and recovery rates. Five of the confirmed cases (1.1%) died. Four of them had ischemic heart disease and hypertension. One patient had diabetes and chronic renal insufficiency. All five patients were over 60 years old and had a history of diabetes or ischemic heart diseases. The case fatality rate increased significantly with age (p=0.001) but not with sex (p=0.68) (Table 2). Meanwhile, 385/452 (85.18%) recovered. No association was found between age or sex and the recovery rate (Table 3).
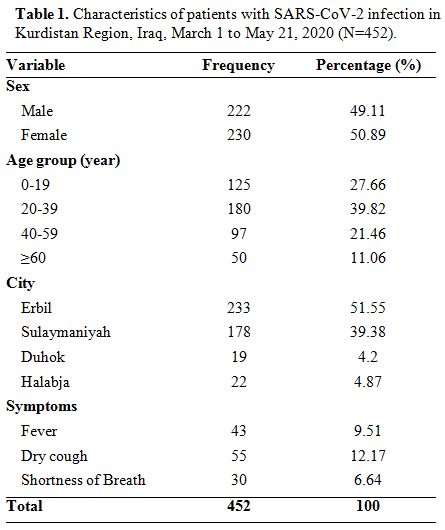 |
Table 1. Characteristics of patients with SARS-CoV-2 infection in Kurdistan Region, Iraq, March 1 to May 21, 2020 (N=452). |
Case Distribution. Following the diagnosis of the first case on March 1, 2020, there was a steady increase in the number of cases. The highest rate of infection was recorded in Erbil (Table 2). The highest number of patients was recorded (44 patients) on April 6, 2020. These patients were interviewed, and it was discovered that they had all attended a funeral, which was forbidden under the social distancing rules that were in place. Case tracing led to the diagnosis of 129 funeral-related cases in Erbil city.
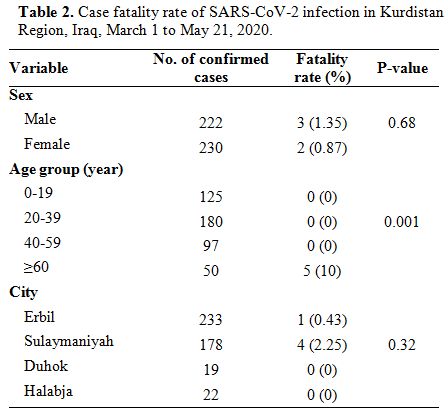 |
Table 2. Case fatality rate of SARS-CoV-2 infection in Kurdistan Region, Iraq, March 1 to May 21, 2020. |
Case fatality and recovery rates. Five of the confirmed cases (1.1%) died. Four of them had ischemic heart disease and hypertension. One patient had diabetes and chronic renal insufficiency. All five patients were over 60 years old and had a history of diabetes or ischemic heart diseases. The case fatality rate increased significantly with age (p=0.001) but not with sex (p=0.68) (Table 2). Meanwhile, 385/452 (85.18%) recovered. No association was found between age or sex and the recovery rate (Table 3).
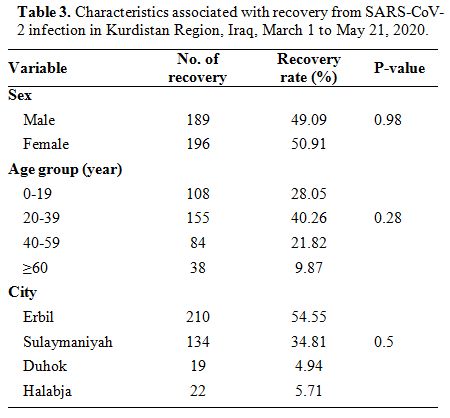 |
Table 3. Characteristics associated with recovery from SARS-CoV-2 infection in Kurdistan Region, Iraq, March 1 to May 21, 2020. |
Discussion
In
the Kurdistan Region of Iraq, 452 cases of SARS-CoV-2 infection were
recorded between March 1 and May 21, 2020, and the highest incidence
was in Erbil city. The higher rate might be related to Erbil’s
location. The capital city shares a border with the Islamic Republic of
Iran, the epicenter of infection in the Middle East.
It has previously been reported that the incidence of both SARS-CoV and SARS-CoV-2 infections is higher in males than in females.[3,4] However, in this study, their number did not differ according to sex. This is difficult to explain and might be due to the relatively small number of infected patients. More studies are needed to determine the reason for sex-related differences in the incidence of infection.
During the study period, five patients died because of the infection. All of them had comorbidities, such as ischemic heart disease and diabetes in agreement with a study conducted in China, where cardiovascular diseases, diabetes millets, chronic obstructive pulmonary diseases, hypertension, and cancers were found as the main risk factors for death.[5] Previous studies found that the case fatality rate increases with age, particularly in patients older than 60 years.[6] In agreement with this, we found a significant association between age and case fatality rate, and all the patients who died were older than 60 years old. Case fatality rates vary according to country; for example, case fatality rates of 4%, 4–8%, and 1.2% have been reported in China,[7] Italy,[8] and Germany,[9] respectively. In our study, the case fatality rate was 1.1%, while the recovery rate was 85%. The low case fatality rate and high cure rate in the Kurdistan Region may be partially attributable to the early diagnosis of the infection and the early initiation of treatment. The majority of cases were young or middle-aged adults. If a higher proportion of the infections had occurred among older adults, such as in Italy, the fatality rate would probably have been higher.
Notably, the Kurdistan Region imposed physical distancing and health-education programs sooner than some other countries and some other parts of Iraq, and that may have played a role in the low case fatality rate. The case fatality rate in Kurdistan may increase as the epidemic progresses. Early pharmaceutical intervention may also have played a role in the high recovery rate. However, this should be interpreted with caution as our study did not test drug efficacy.
The most common clinical features associated with the infection have been reported to be fever, dry cough, shortness of breath, rhinitis, and hemoptysis.[10] In our study, the most common symptoms were fever (9.5%), dry cough (12%), and mild shortness of breath (6.5%); however, most patients were either asymptomatic or had mild symptoms. None of the patients in our study required mechanical ventilation.
It has been shown that strict social distancing helped control the outbreak in this region.[11,12] The highest number of patients was recorded in Erbil city on April 6. Interviewing those patients revealed that all attended a prohibited funeral. Tracing the persons attending the funeral resulted in the identification of 129 people who had become infected. Consequently, state-imposed community-wide containment was declared, including a state-imposed curfew, and which controlled the spread of the infection, and the number of cases declined.
One of the limitations of our study was that centers used different definitions for the duration of recovery. In some centers, the length was calculated from the first positive PCR of the diagnosis to the first negative PCR of the recovery. In contrast, other centers used different approaches, such as the duration of hospital admission. Therefore, the calculation of the time to recovery and its relationship to age and sex could not be assessed.
To conclude, a majority of the patients diagnosed with COVID-19 were in Erbil city and were asymptomatic. Most patients recovered without complications. The case fatality rate was low and increased with age. Comprehensive research is needed to investigate regional variation in virus strains, the role of host genetic factors, and immune responses in different populations
It has previously been reported that the incidence of both SARS-CoV and SARS-CoV-2 infections is higher in males than in females.[3,4] However, in this study, their number did not differ according to sex. This is difficult to explain and might be due to the relatively small number of infected patients. More studies are needed to determine the reason for sex-related differences in the incidence of infection.
During the study period, five patients died because of the infection. All of them had comorbidities, such as ischemic heart disease and diabetes in agreement with a study conducted in China, where cardiovascular diseases, diabetes millets, chronic obstructive pulmonary diseases, hypertension, and cancers were found as the main risk factors for death.[5] Previous studies found that the case fatality rate increases with age, particularly in patients older than 60 years.[6] In agreement with this, we found a significant association between age and case fatality rate, and all the patients who died were older than 60 years old. Case fatality rates vary according to country; for example, case fatality rates of 4%, 4–8%, and 1.2% have been reported in China,[7] Italy,[8] and Germany,[9] respectively. In our study, the case fatality rate was 1.1%, while the recovery rate was 85%. The low case fatality rate and high cure rate in the Kurdistan Region may be partially attributable to the early diagnosis of the infection and the early initiation of treatment. The majority of cases were young or middle-aged adults. If a higher proportion of the infections had occurred among older adults, such as in Italy, the fatality rate would probably have been higher.
Notably, the Kurdistan Region imposed physical distancing and health-education programs sooner than some other countries and some other parts of Iraq, and that may have played a role in the low case fatality rate. The case fatality rate in Kurdistan may increase as the epidemic progresses. Early pharmaceutical intervention may also have played a role in the high recovery rate. However, this should be interpreted with caution as our study did not test drug efficacy.
The most common clinical features associated with the infection have been reported to be fever, dry cough, shortness of breath, rhinitis, and hemoptysis.[10] In our study, the most common symptoms were fever (9.5%), dry cough (12%), and mild shortness of breath (6.5%); however, most patients were either asymptomatic or had mild symptoms. None of the patients in our study required mechanical ventilation.
It has been shown that strict social distancing helped control the outbreak in this region.[11,12] The highest number of patients was recorded in Erbil city on April 6. Interviewing those patients revealed that all attended a prohibited funeral. Tracing the persons attending the funeral resulted in the identification of 129 people who had become infected. Consequently, state-imposed community-wide containment was declared, including a state-imposed curfew, and which controlled the spread of the infection, and the number of cases declined.
One of the limitations of our study was that centers used different definitions for the duration of recovery. In some centers, the length was calculated from the first positive PCR of the diagnosis to the first negative PCR of the recovery. In contrast, other centers used different approaches, such as the duration of hospital admission. Therefore, the calculation of the time to recovery and its relationship to age and sex could not be assessed.
To conclude, a majority of the patients diagnosed with COVID-19 were in Erbil city and were asymptomatic. Most patients recovered without complications. The case fatality rate was low and increased with age. Comprehensive research is needed to investigate regional variation in virus strains, the role of host genetic factors, and immune responses in different populations
Acknowledgments
We
thank all healthcare workers in the COVID centers of the Kurdistan
Region. We are grateful for the data provided for this paper thanks to
daily updates from the Ministry of Health and the Directorate of Health
via websites and related media. These data are part of a national
program to combat the outbreak and update regularly.
References
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao
X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao
GF, Tan W. A Novel Coronavirus from Patients with Pneumonia in China,
2019. The New England journal of medicine 2020;382(8):727-733. https://doi.org/10.1056/NEJMoa2001017 PMid:31978945 PMCid:PMC7092803
- National
Health Commission & State Administration of Traditional Chinese
Medicine. Diagnosis and Treatment Protocol for Novel Coronavirus
Pneumonia (Trial Version 7). 2020 [updated 2020; cited 2020 14/March];
Available from: http://busan.china-consulate.org/chn/zt/4/P020200310548447287942.pdf
- Kolifarhood
G, Aghaali M, Mozafar Saadati H, Taherpour N, Rahimi S, Izadi N,
Hashemi Nazari SS. Epidemiological and Clinical Aspects of COVID-19; a
Narrative Review. Arch Acad Emerg Med 2020;8(1):e41-e41.
- Channappanavar
R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, Perlman S. Sex-Based
Differences in Susceptibility to Severe Acute Respiratory Syndrome
Coronavirus Infection. J Immunol 2017;198(10):4046-4053. https://doi.org/10.4049/jimmunol.1601896 PMid:28373583 PMCid:PMC5450662
- Huang
C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng
Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H,
Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical
features of patients infected with 2019 novel coronavirus in Wuhan,
China. The Lancet 2020;395(10223):497-506. https://doi.org/10.1016/S0140-6736(20)30183-5
- Khafaie
MA, Rahim F. Cross-Country Comparison of Case Fatality Rates of
COVID-19/SARS-COV-2. Osong Public Health Res Perspect 2020;11(2):74-80.
https://doi.org/10.24171/j.phrp.2020.11.2.03 PMid:32257772 PMCid:PMC7104689
- Wu
Z, McGoogan JM. Characteristics of and Important Lessons From the
Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a
Report of 72 314 Cases From the Chinese Center for Disease Control and
Prevention. JAMA 2020;323(13):1239-1242. https://doi.org/10.1001/jama.2020.2648 PMid:32091533
- Fanelli
D, Piazza F. Analysis and forecast of COVID-19 spreading in China,
Italy and France. Chaos, Solitons & Fractals 2020;134:109761. https://doi.org/10.1016/j.chaos.2020.109761 PMid:32308258 PMCid:PMC7156225
- Stafford N. Covid-19: Why Germany's case fatality rate seems so low. BMJ 2020;369:m1395. https://doi.org/10.1136/bmj.m1395 PMid:32265194
- Adhikari
SP, Meng S, Wu Y-J, Mao Y-P, Ye R-X, Wang Q-Z, Sun C, Sylvia S, Rozelle
S, Raat H, Zhou H. Epidemiology, causes, clinical manifestation and
diagnosis, prevention and control of coronavirus disease (COVID-19)
during the early outbreak period: a scoping review. Infectious Diseases
of Poverty 2020;9(1):29. https://doi.org/10.1186/s40249-020-00646-x PMid:32183901 PMCid:PMC7079521
- Hussein
NR, Naqid IA, Saleem ZSM, Musa DH, Ibrahim N. The Impact of Breaching
Lockdown on the Spread of COVID-19 in Kurdistan Region, Iraq. Avicenna
J Clin Microbiol Infect 2020;7(1):34-35.
- Hussein
N. The Impact of COVID-19 Pandemic on the Elimination of Viral
Hepatitis in Duhok City, Kurdistan Region of Iraq. Hepat Mon
2020;20(5):e104643. https://doi.org/10.5812/hepatmon.104643