Zied Hajjej, Kalthoum Ben Mahmoud, Aicha Rebai, Hedi Gharsallah, Iheb Labbene and Mustapha Ferjani.
Université de Tunis El
manar, Faculté de Médecine de tunis, Department of Anesthesiology and
Critical Care Medicine ,LR12DN01, Military Hospital of Tunis, Tunisia,
1008 Montfleury, Tunis-Tunisia.
Correspondence to Zied
Hajjej. Université de Tunis El manar, Faculté de Médecine de tunis,
Department of Anesthesiology and Critical Care Medicine, LR12DN01,
Military Hospital of Tunis, Tunisia, 1008 Montfleury, Tunis-Tunisia.
Tel. +21671-391-133; Fax +216-71-391-099. E-mail:
hajjej_zied@hotmail.com ORCID identifier : 0000-0003-2812-9802
Published: September 1, 2021
Received: April 19, 2021
Accepted: August 7, 2021
Mediterr J Hematol Infect Dis 2021, 13(1): e2021040 DOI
10.4084/MJHID.2021.052
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background: Since
they were first published in 2016, Sepsis-3 definitions have not been
universally accepted. Rather, they have become a source of controversy
because the clinical and laboratory parameters used had been derived
mainly from patients hospitalized in Intensive Care Units (ICU) in the
United States.
Purpose: The
aim of this study was to evaluate the performance of the Sepsis‑3
definitions for the prediction of ICU-mortality in a Tunisian ICU
population as compared to the 2003 Consensus Definitions (Sepsis-2
definitions)
Method: The
study, conducted in an 18-bed medical-surgical ICU at the Military
Hospital of Tunis (Tunisia), was retrospective in nature. From
January 2012 to January 2016, all patients admitted to the ICU for
sepsis, severe sepsis, or septic shock as defined according to the 2003
Consensus Definitions (Sepsis-2 consensus) were eligible for this
study. The new Sepsis-3 definition was then used to classify the
included patients. The primary area of interest was ICU mortality,
defined as death before ICU discharge
Results: A
total of 1080 patients were included during the recruitment period.
When Sepsis-2 definitions were used, there was a difference in
mortality only between septic shock and sepsis patients. Sepsis-3
definitions show that mortality increased from 16% among
no-dysfunction-infected patients to 30% among patients with qSOFA ≥ 2
and 44% and 46% for sepsis or septic shock patients, respectively.
Conclusions:
Sepsis-3 definitions were better than sepsis-2 definitions at
stratifying mortality among septic patients admitted to an ICU of a
middle-income country (Tunisia).
|
Introduction
Sepsis
is the major health threat among all the infectious pathologies, having
the biggest impact in terms of mortality before or after the era of
antibiotics, especially among critically ill patients.[1]
The first definition of sepsis, provided in 1991 and published in 1992,
revolved around the systemic inflammatory response syndrome (SIRS)
criteria.[2] However, many have noted the limitations
of the SIRS criteria and the need for improvement, which led to a
second definition in 2003.[3] However, this latter
definition has not changed the first classification. In 2016, an
international consensus task force published the Sepsis-3
definition,[4] recognizing sepsis as more complex than infection and
inflammation and defining it as a “life-threatening organ dysfunction
due to a dysregulated host response to infection”. In this new
definition (Sepsis 3), the host response resulting in organ failure
from an infection is stressed.
In contrast, the inflammation stage
known as SIRS in the previous definitions « Sepsis 2 » is removed.
Accordingly, the Sequential Organ Failure Assessment (SOFA) score is
now crucial for classifying sepsis. So, in providing early bedside
evaluation of a patient for the possibility of sepsis, the quick SOFA
(qSOFA) score was used.
It should be noted that sepsis-3
definitions are not universally accepted. Rather, they have become a
source of controversy. Because clinical and laboratory parameters used
for the development of these definitions were derived mainly from
patients hospitalized in Intensive Care Units (ICU) in the United
States, the primary study’s endpoint analysis was mortality. However,
the presence of organ dysfunction should also be part of this analysis.
The Sepsis-3 definitions Task Force clearly points out the need to
validate the newly proposed definition using databases of non-US
patients. The authors highlight in particular the need to validate the
utility of the qSOFA score.
Tunisia is a developing country with
limited healthcare resources. A more clearly defined strategy is
therefore needed for admitting very severely ill patients to Intensive
care units. Currently, in our intensive care unit, patients admitted
for suspected infection are classified according to sepsis-2
definitions, mainly using SIRS criteria.
The main aim of this
study was to evaluate the performance of the Sepsis‑3 definitions for
the prediction of ICU mortality in a Tunisian ICU population compared
to 2003 Consensus Definitions (Sepsis-2 definitions). The study's
secondary objective was to compare the performance of qSOFA and the
SIRS criteria for the early prediction of ICU mortality.
Materials and Methods
Patients and Study design.
The study was a retrospective descriptive study conducted in an 18-bed
medical-surgical ICU at the Military Hospital of Tunis (Tunisia).
From
January 2012 to January 2016, all patients admitted to the ICU were
eligible for this study. Inclusion criteria were as follows: age >18
years, and an admission diagnosis of sepsis, severe sepsis or septic
shock as defined by the 2003 Consensus Definitions (Sepsis-2
consensus). In addition, patients with incomplete data in their records
or those hospitalized for less than 48 h were excluded (patients who
passed away within 48 h were not excluded).
The study had been
reviewed and approved by the Institutional Ethics Authorities. However,
informed consent was not deemed necessary because of the retrospective
and observational design of the study.
Data collection. Data
were collected using standardized forms. The following information was
retrieved: gender, age, Acute Physiology and Chronic Health Evaluation
(APACHE) II score, Sequential Organ Failure Assessment (SOFA) score,
reasons for hospitalization, etiological diagnosis, worst and best
vital signs during the first ICU day, comorbidities, ICU length of stay
(LOS), highest lactate level of the first day, source of infection,
causal organisms, use of antimicrobials and clinical ICU outcomes. The
SOFA score was determined at the time of ICU admission. In addition,
laboratory variables were retrieved from the database specific to
laboratory data.
Sepsis and Reclassification definitions.
Patients in our database were primarily classified using Sepsis-2
definitions. According to previously published consensus, sepsis,
severe sepsis, and septic shock categories were used.[3] The new Sepsis-3 definition was secondarily used.[4]
The points used for definitions were those collected at admission to the ICU.
We
calculated the quick Sequential Organ Failure Assessment (qSOFA) score
by assigning patients 1 point for each of the following criteria:
systolic blood pressure less than or equal to 100 mmHg, a respiratory
rate greater than or equal to 22 breaths/min, or altered mental status
documented by the physician, using the most abnormal value during the
first 24 hours of admission.
Regarding reclassification, patients
defined as either sepsis according to Sepsis-3 and/or severe sepsis
using Sepsis-2 definitions were considered together as severe cases.
Among these severe cases, those defined as sepsis by the Sepsis-3
definitions and as uncomplicated sepsis by the Sepsis-2 definitions
were considered reclassified by the Sepsis-2 definitions. The clinical
cases defined as infection by the Sepsis-3 definitions and as severe
sepsis by the Sepsis-2 definitions were considered reclassified by the
Sepsis-3.
Study endpoint. The primary study endpoint was the ICU mortality, defined as death before ICU discharge.
Data statistical Analysis.
For each patient, we primarily calculated the qSOFA score. We
subsequently calculated the sensitivity and specificity of the qSOFA
score greater than or equal to 2 and SIRS of the previous definitions
of sepsis and severe sepsis for ICU mortality. Statistical analysis was
carried out using SPSS v.20.0 (SPSS, Inc., Chicago, IL, USA.).
Continuous variables are expressed as mean ± standard deviation, while
categorical variables are expressed with absolute and relative
frequencies. The normality assumption of continuous variables was
evaluated using the Kolmogorov Smirnov criterion.
Parametric
continuous variables were compared among groups using the t-test;
nonparametric variables were compared using the Mann-Whitney test. The
Chi-squared test was used to compare categorical variables among the
groups.
To assess the performances of the qSOFA to predict ICU
mortality, we calculated diagnostic performances (sensitivity,
specificity) for a qSOFA score of 2 or higher. We constructed a
receiver operating characteristic (ROC) curve and calculated the
corresponding area under the ROC curve (AUROC). The performance of
qSOFA was compared to that of SIRS, mainly at least for 2 elements. The
DeLong test was used to compare the AUCs of the two criteria.
All statistical analyses were 2-tailed, and a P value less than 0.05 was required for statistical significance.
Results
Study population.
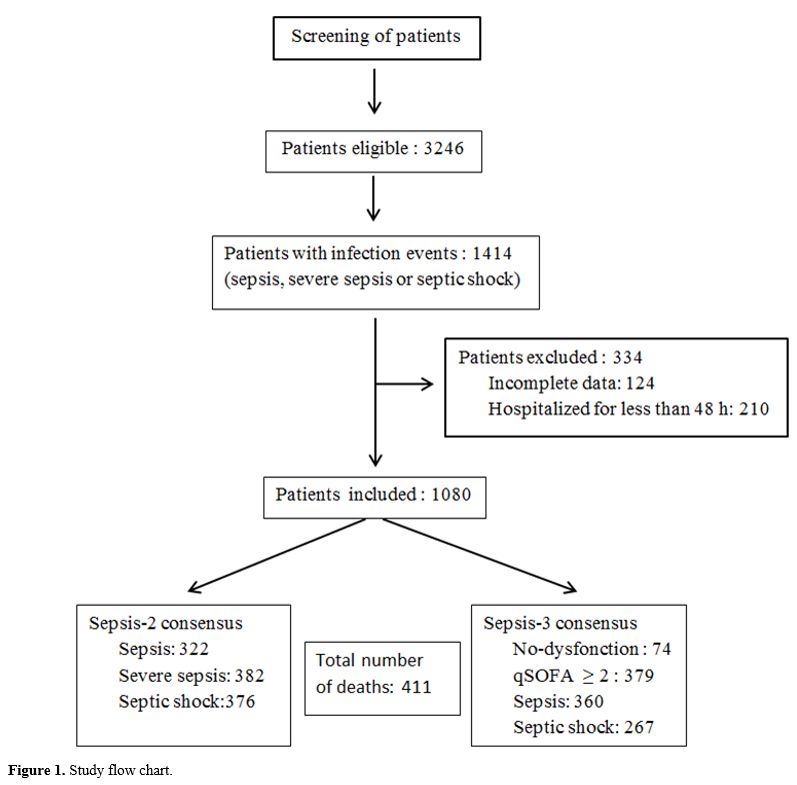
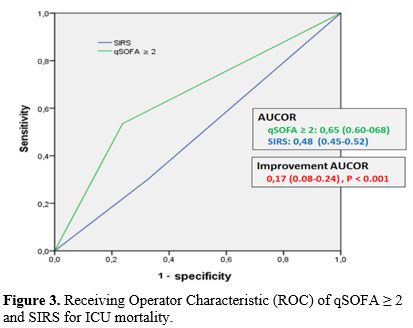
Out of the 3246 participants who enrolled between 2012 and 2016, we
included 1080 individuals whose follow-up information was available (Figure 1).
 |
Figure
1. Study flow chart.
|
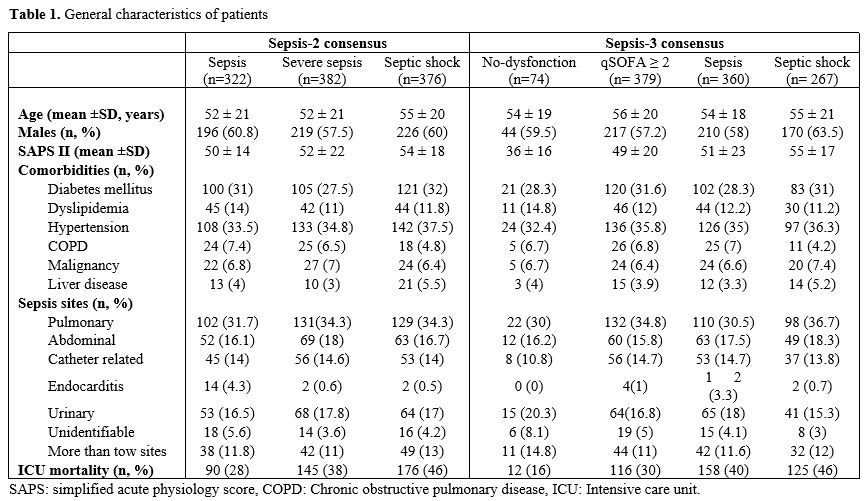
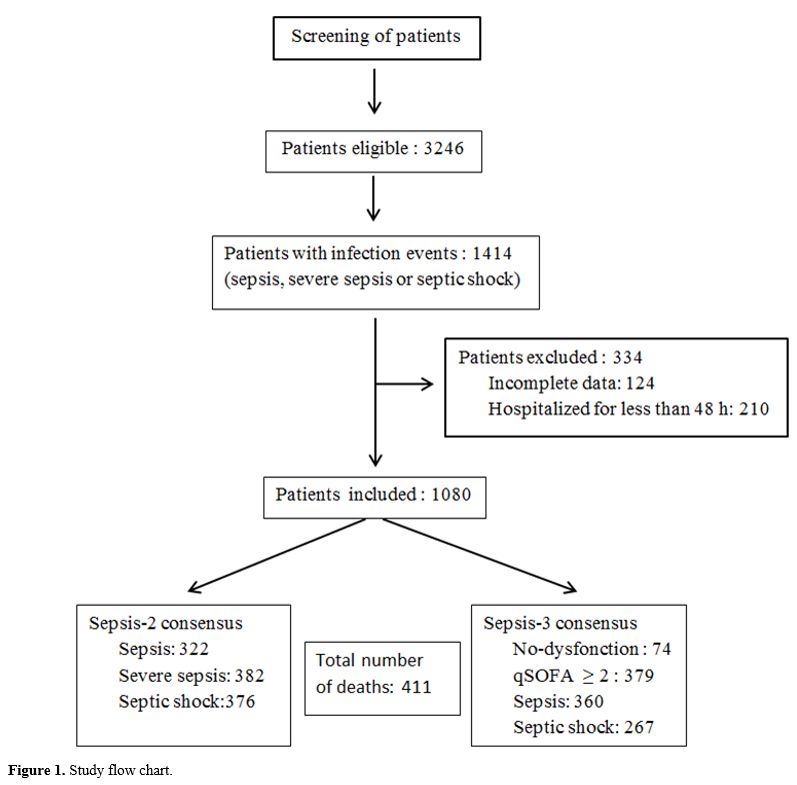
Patients’ characteristics. The general characteristics of patients and clinical outcomes, source of infection, and comorbidities are given in Table 1.
The
most common comorbid conditions were diabetes and hypertension. The
most frequent infectious site was the respiratory site, followed by the
urinary and abdominal tract sites. ICU mortality was 38%.
 |
Table
1. General characteristics of patients
|
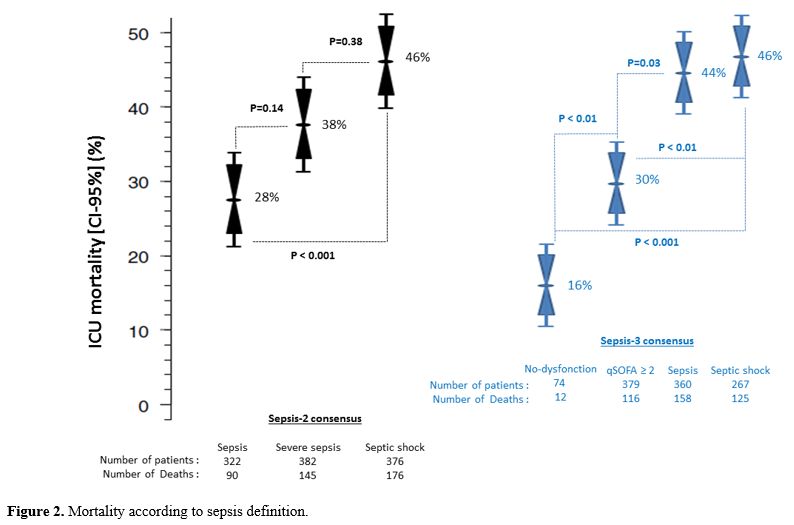
Performance of Sepsis-3 definitions.
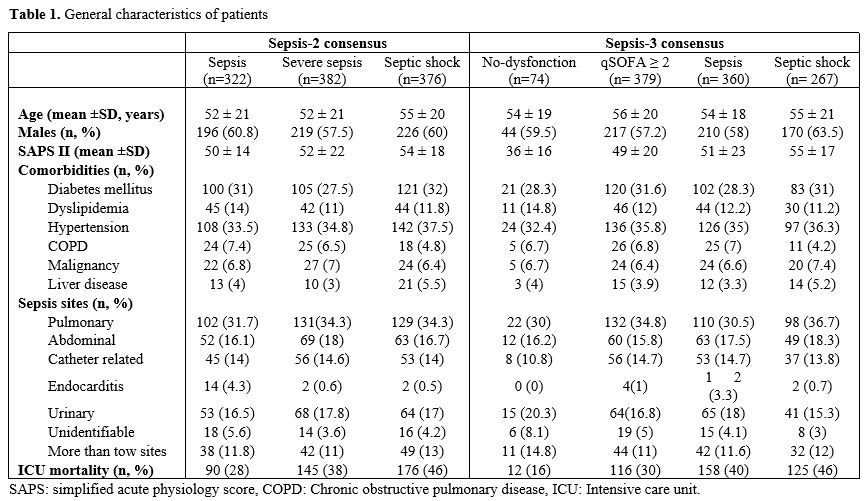
When the Sepsis-2 definitions were used, there was a difference in
mortality only among septic shock and sepsis patients (46 and 28%,
respectively). However, there is no difference in mortality among
sepsis and septic shock categories. Sepsis- 3 criteria clearly
categorized septic patients according to a spectrum of severity, since
mortality increased from 16% in no-dysfunction-infected patients to 30,
and 44% for qSOFA ≥ 2 and sepsis patients categories, respectively (Figure 2).
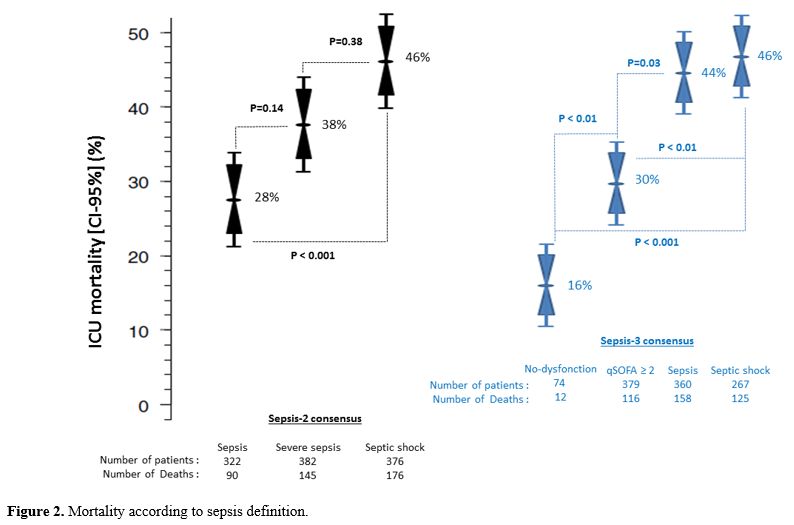 |
Figure 2. Mortality according to sepsis definition.
|
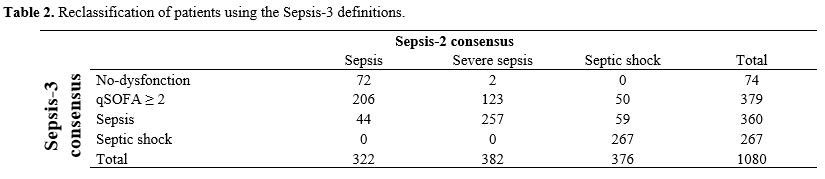
Reclassification of the patients.
When the new Sepsis-3 definitions were used, 71% of the patients
defined by the Sepsis-2 consensus as patients with septic shock were
also classified by the Sepsis-3 definitions as septic shock patients (Table 2).
The reclassification of cases by the Sepsis-2 definitions occurred
among 390 out of 1080 cases (36%). Using the Sepsis-3 definitions, this
occurred among 74 cases (7%) (p =0.001).
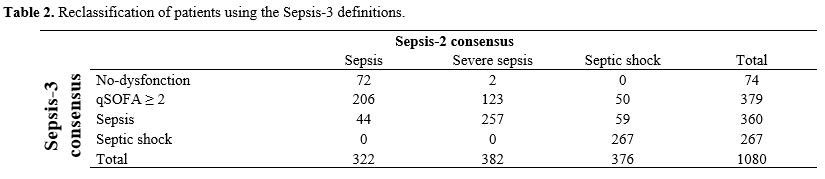 |
Table
2. Reclassification of patients using the Sepsis-3 definitions.
|
Performance of the qSOFA.
The sensitivity and specificity of qSOFA ≥ 2 to predict ICU mortality
were 53.5% and 76.2%, respectively. The qSOFA performed better than
SIRS in predicting in-hospital mortality, with an area under the
receiver operating curve (AUROC) of 0.65 (95% CI, 0.60-0.68) vs 0.48
(95% CI, 0.45-0.52) for SIRS (P < 0.001; Improvement AUROC, 0.17;
95% CI, 0.08-0.24) (Figure 3).
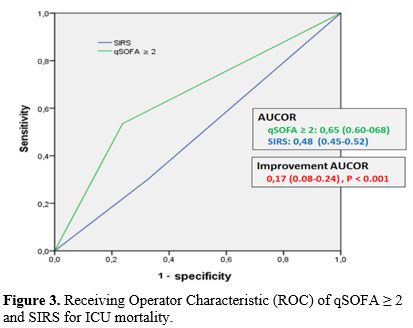 |
Figure 3. Receiving Operator Characteristic (ROC) of qSOFA ≥ 2 and SIRS for ICU mortality.
|
Discussion
When
the sepsis 2 definitions were used in our study, there was a difference
in mortality only among septic shock and sepsis patients. On the other
hand, sepsis 3 definitions show that mortality increased from 16% among
no-dysfunction infected patients to 30% among patients with qSOFA ≥ 2
and 44% or 46% for sepsis or septic shock patients, respectively.
Therefore, sepsis-3 was better than sepsis 2 at stratifying mortality
among septic patients admitted to an ICU in a developing country. The
validity of sepsis definitions based on SIRS criteria has recently been
extensively questioned. This is because 90% of the patients admitted to
an ICU meet the SIRS criteria.[5,6]
On the other
hand, some patients who suffer from an infectious disease and new
organs’ failure do not meet 2 SIRS criteria and therefore do not
achieve previous sepsis definitions.[7] More
importantly, the categories of sepsis, severe sepsis, and septic shock
indicate an actual spectrum of severity why representing different
outcome categories.[8] Thus, the present study
emphasizes a lack of accuracy of Sepsis-2 definitions of sepsis, severe
sepsis, and septic shock in stratifying patients’ mortality risk.
Additionally, our data demonstrate that sepsis-3 definitions of
infection without organ dysfunction, qSOFA ≥ 2, sepsis, and septic
shock clearly represent a progressive stratification of mortality risk.
The
two studies carried out in the emergency department and intensive care
units will be reported here. An International prospective cohort study
was conducted in France, Spain, Belgium, and Switzerland between May
and June 2016.[9] For 4 weeks in the 30 participating
emergency departments, consecutive patients who visited the emergency
departments with suspected infection were included. The aim of the
study was to prospectively validate qSOFA as a mortality predictor and
compare the performances of the new sepsis criteria to the previous
ones. Out of the 1088 patients screened, 879 were included in the
analysis. Overall in-hospital mortality was 8%: 3% for patients with a
qSOFA score lower than 2 vs. 24% for those with qSOFA score of 2 or
higher (absolute difference, 21%; 95%CI, 15%-26%). The qSOFA performed
better than both SIRS and severe sepsis in predicting in-hospital
mortality, with an area under the receiver operating curve (AUROC) of
0.80 (95%CI, 0.74-0.85) vs 0.65 (95%CI, 0.59-0.70) for both SIRS and
severe sepsis (P < .001; incremental AUROC, 0.15; 95%CI, 0.09-0.22).
The hazard ratio of qSOFA score for death was 6.2 (95%CI, 3.8-10.3) vs.
3.5 (95%CI, 2.2-5.5) for severe sepsis. It was concluded that among the
patients admitted to the emergency department with suspected infection,
the use of qSOFA resulted in greater prognostic accuracy for
in-hospital mortality than did either SIRS or severe sepsis. These
findings support the Third International Consensus Definitions for
Sepsis and Septic Shock (Sepsis-3) criteria in the emergency department
setting.
Comparatively, the validity of these new definitions has
also been tested among patients admitted to intensive care. A
retrospective cohort analysis of 184 875 patients with an
infection-related primary admission diagnosis in 182 Australian and New
Zealand intensive care units (ICUs) from 2000 through 2015 was carried
out. The main aim was to assess the discriminatory capacities of an
increase in SOFA score by 2 or more points, 2 or more SIRS criteria, or
a qSOFA score of 2 or more points for outcomes among patients with
suspected infection. The primary outcome was in-hospital mortality.
SOFA score ≥2 was much more discriminating (AUROC 0,753) than the SIRS
criteria (AUROC 0.589) and the qSOFA score (AUROC 0.607) for the
criterion of the primary outcome (p <0.001). The conclusion was that
among adults with suspected infection admitted to an ICU, an increase
in SOFA score of 2 or more had greater prognostic accuracy for
in-hospital mortality than SIRS criteria or the qSOFA score. These
findings suggest that SIRS criteria and qSOFA may have limited utility
for predicting mortality in an ICU setting.[10]
The
data from these studies, including ours, can encourage the adoption of
these new prognostic tools. Nevertheless, several questions remain
unanswered regarding the news definitions: [11-14]
(a) The inclusion of patients from the United States and Europe and not
from economically developing countries; (b) The focus on adult patients
without including pediatric patients; (c) The changes in stages of
sepsis, making comparisons with prior research difficult; (d) The term
“organ dysfunction” used in the new definition is still unclear, since
organs may have more than one function. Organ dysfunction may emerge
for multiple reasons other than sepsis, making it difficult to
distinguish between sepsis-related organ dysfunction. In the same way,
when the infection is not certain, and organ dysfunction is there, it
is difficult to exclude a sepsis diagnosis; and (e)There was no clear
emphasis on the added benefit of lactate for patients with SOFA scores
<2, possibly because of lactate values lack in the derivation (about
60%) and validation cohorts (about 90%). Interestingly, lactate was not
retained in the novel qSOFA during model construction. However, the
authors state that for a qSOFA score of 1, high lactate values
characterized a population with a similar risk to patients with a qSOFA
score of 2.
Based on our study, misclassification of cases by the
Sepsis-2 definitions occurred among 390 out of 1080 cases (36%). Using
the Sepsis-3 definitions, this occurred among 74 cases (7%) (p =0.001).
In the study published in 2017 by Giamarellos-Bourboulis E et al,
misclassification of severe cases by the 1991 definition occurred in
734 out of 2172 severe cases (33.8%). Using the Sepsis-3 definitions,
this occurred among 128 out of 2172 severe cases (5.9%) (p <0.0001
between the 1991 and Sepsis-3 definitions).[15] The introduction of Sepsis-3 definitions limited the misclassification of severe cases.
Our
study has not been designed to evaluate Sepsis-2 or Sepsis-3 as a
screening tool, as only patients admitted to ICU were included.
Nevertheless, the role of sepsis-2 criteria in the identification of
septic patients is undeniable. However, its role in the stratification
of severity can be questioned, as demonstrated by our data. As a
result, our study clearly shows a better discriminant performance of
Sepsis-3 in predicting mortality in ICU.
The main strengths of our
study were its large sample size and the detailed health information
about the enrolled participants. As far as we know, this is the first
study dealing with the validation of sepsis 3 definitions among
patients from a middle-income country. Despite these strengths, our
findings must be interpreted in light of several limitations. First,
the retrospective character of this study makes it difficult to
elucidate known confounders that could have biased the outcome
measures. Second, this was a single-center study, and our results may
not be generalizable to other centers since there is a wide variation
in outcomes when comparing different settings. Third, the validity of
Sepsis-3 criteria in this study was assessed based on ICU mortality.
Although ICU mortality is not the most appropriate endpoint to be
evaluated, it reflects the care provided to septic patients before and
after their admission to ICU. Fourth, we did not follow up discharged
patients and only focused on in-hospital mortality.
Conclusions
Two
important findings from our study should be emphasized: (a) Sepsis-3
definitions were better than sepsis-2 definitions at stratifying
mortality, and (b) The rate of misclassification of severe patients is
lower using the Sepsis-3 definitions compared with sepsis-2 definitions.
Acknowledgments
The
authors are thankful to the doctors and nurses in the Intensive Care
Unit who provided care for the patients included in the study.
References
- Gaieski DF, Edwards JM, Kallan MJ, Carr BG.
Benchmarking the incidence and mortality of severe sepsis in the United
States. Crit Care Med. 2013;41:1167-1174. https://doi.org/10.1097/CCM.0b013e31827c09f8
- Bone
RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM,
Sibbald WJ .Definitions for sepsis and organ failure and guidelines for
the use of innovative therapies in sepsis. The ACCP/SCCM Consensus
Conference Committee. American College of Chest Physicians/Society of
Critical Care Medicine. Chest. 1992;101:1644-55. https://doi.org/10.1378/chest.101.6.1644
- Levy
M, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/
ESICM/ ACCP/ ATS/ SIS international sepsis definitions conference.
Intensive Care Med. 2003;29:530e8. https://doi.org/10.1007/s00134-003-1662-x
- Singer
M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al.
The third international consensus definitions for sepsis and septic
shock (Sepsis-3). JAMA. 2016;315:801-810. https://doi.org/10.1001/jama.2016.0287
- Sprung
CL, Sakr Y, Vincent JL, Le Gall JR, Reinhart K, Ranieri VM, et al. An
evaluation of systemic inflammatory response syndrome signs in the
Sepsis Occurrence In Acutely Ill Patients (SOAP) study. Intensive Care
Med. 2006; 32:421-427. https://doi.org/10.1007/s00134-005-0039-8
- Lai
NA, Kruger P. The predictive ability of a weighted systemic
inflammatory response syndrome score for microbiologically confirmed
infection in hospitalized patients with suspected sepsis. Crit Care
Resusc. 2011; 13:146-150.
- Kaukonen KM,
Bailey M, Pilcher D, Cooper DJ, Bellomo R. Systemic inflammatory
response syndrome criteria in defining severe sepsis. N Engl J Med
2015;372:1629-1638. https://doi.org/10.1056/NEJMoa1415236
- Deutschman CS. Imprecise medicine: the limitations of sepsis-3. Crit Care Med. 2016;44:857-858. https://doi.org/10.1097/CCM.0000000000001834
- Freund
Y, Lemachatti N, Krastinova E et al. Prognostic Accuracy of Sepsis-3
Criteria for In-Hospital Mortality Among Patients With Suspected
Infection Presenting to the Emergency Department. JAMA.
2017;317:301-308. https://doi.org/10.1001/jama.2016.20329
- Raith
EP, Udy AA, Bailey M, McGloughlin S et al. Prognostic Accuracy of the
SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality
Among Adults With Suspected Infection Admitted to the Intensive Care
Unit. JAMA. 2017 ; 317 :290-300. https://doi.org/10.1001/jama.2016.20328
- Charles Sprung and Konrad Reinhart .Definitions for Sepsis and Septic Shock . JAMA. 2016 ; 316:456. https://doi.org/10.1001/jama.2016.6377
- Kleinpell
R M. Schorr C. Robert S .The New Sepsis Definitions : Implications for
Critical Care Practitioners. AJCC. 2016 ; 25:457-464. https://doi.org/10.4037/ajcc2016574
- Abraham
E.New Definitions for Sepsis and Septic Shock: Continuing Evolution but
With Much Still to Be Done. JAMA. 2016 ; 315:757-759. https://doi.org/10.1001/jama.2016.0290
- Fethi G, Mustapha K A, Ismail C, Anand K. Changing definitions of Sepsis. Turk J Anaesthesiol Reanim. 2017 ; 45:129-138. https://doi.org/10.5152/TJAR.2017.93753
- Giamarellos-Bourboulis
E, Tsaganos T, Tsangaris I, Lada M, Routsi C, Sinapidis Det
al.Validation of the new Sepsis-3 definitions: proposal for improvement
in early risk identification. Clin Microbiol Infect. 2017;23 :104-109. https://doi.org/10.1016/j.cmi.2016.11.003
[TOP]