Sickle cell
disease (SCD) is a group of hereditary red cell disorders determining a
multisystem disease and clinical manifestations of variable severity.
Patients with compound heterozygosity for HbS and β+-thalassaemia
mutation generally present a mild-moderate form of the disease;
however, they seem to be more subjected to fat embolism syndrome (FES).[1] This is a rare and devastating
complication of SCD resulting from massive bone marrow necrosis and is
associated with multiorgan dysfunction and high mortality. In this
letter, we report the case of a drug-resistant nonconvulsive status
epilepticus (NCSE), probably triggered by a cerebral fat embolism
(CFE), in a HbS/β⁺-thalassaemia patient.
A Caucasian 61-year-old woman with HbS/β+-thalassaemia (βS/β+-IVS-I-6;
α+832 G>Aα/αα) presented to the Emergency Department (ED) with
severe precordial chest pain, dyspnoea, oxygen desaturation, and a
normal chest x-ray. Diagnosis of SCD was made during childhood but,
until the age of 50, she had only a few uncomplicated vaso-occlusive
crises (VOCs). Two years before this episode, neurological and
cardiological studies had been performed following a suspected
transient ischemic attack with negative results, except for the
presence of a patent foramen ovale (PFO), resulting in right-left shunt
without surgical indications. Thus, she had started Hydroxyurea (8.6
mg/kg/d, maximum tolerated dose due to thrombocytopenia at higher
dosage), and prophylaxis with acetylsalicylic acid (100 mg/d). At the
ED, acute chest syndrome (ACS) associated with VOC was suspected.
Intravenous rehydration, low-flow oxygen, opioid analgesia, and top-up
transfusion were initiated, and she was admitted. Unfortunately, due to
poor suitable vascular access, eritroexchange (EEX) transfusion therapy
was delayed over 24 hours. The following day, dyspnoea, oxygen
saturation, and mental status worsened (Glasgow Coma Scale, GCS, 11:
E4, V2, M5). Electrocardiogram (ECG) showed minor alterations, and
Doppler ultrasonography of the lower limbs was not evocative for deep
venous thrombosis. Brain-Computer Tomography (CT) was unremarkable, and
naloxone, administered suspecting an opioid intoxication, showed no
benefits. Blood tests reported a drop in platelets and leukocytes count
and increased inflammatory and haemolytic markers, coagulation and
liver function tests, cardiac enzyme, and N-terminal prohormone of
brain natriuretic peptide. Microbiological analyses were negative but,
due to a diffuse bilateral parenchymal infiltrate at the chest X-ray,
empirical antibiotic therapy with piperacillin/tazobactam was started.
Despite adequate EEX transfusions (target Hb 10-11 g/dl and HbS
<30%) being finally established, she became unresponsive (GCS 8:
E2, V2, M4), requiring intubation for airway protection. Urgent brain
and neck CT angiography was negative for haemorrhages and acute
vascular occlusions. Continuous Electroencephalogram (EEG) monitoring
showed recurrent epileptiform discharges and triphasic waves in the
temporal-central regions bilaterally consistent with NCSE; therapy with
benzodiazepine, levetiracetam, and valproic acid was started. Cerebral
spinal fluid (CSF) analyses for viral and bacterial infections resulted
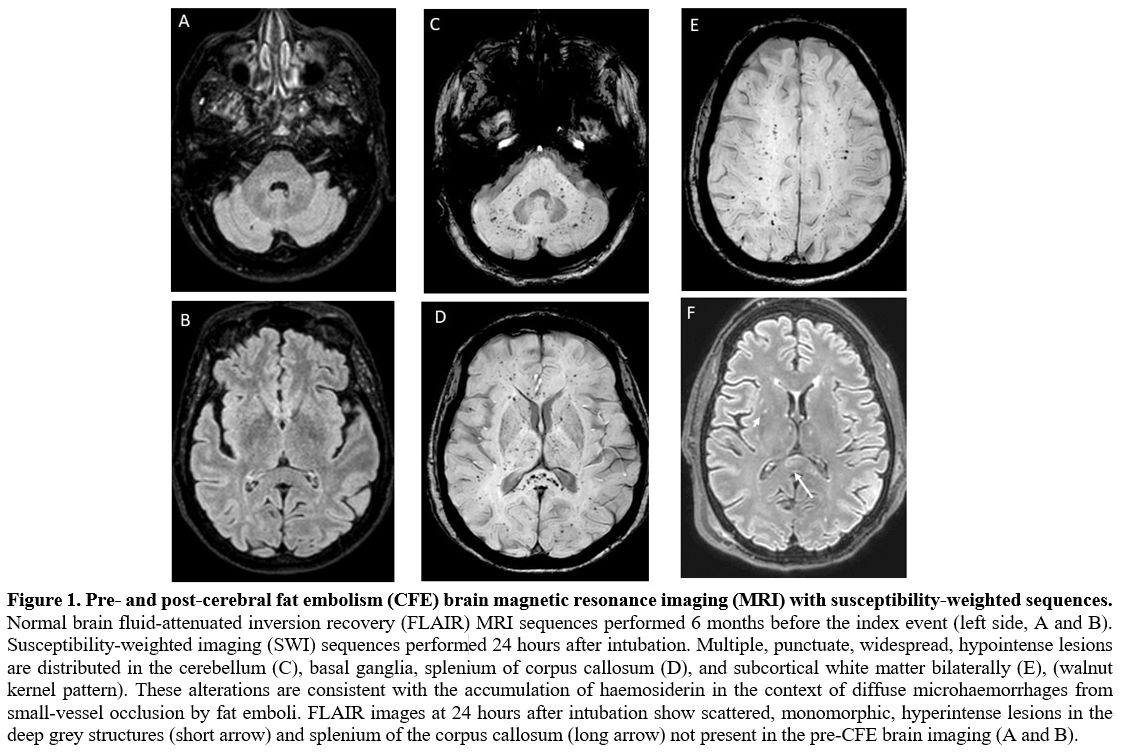
negative. Brain magnetic resonance imaging (MRI) showed widespread,
non-confluent areas of ischemia in multiple anterior and posterior
vascular distributions with microhaemorrhages. These alterations
detected with susceptibility-weighted imaging (SWI), specific MRI
sequences sensible to compounds distorting the local magnetic field
(such as iron from haemoglobin), were consistent with a “starfield
appearance” with a “walnut kernel microbleed” pattern" (Figure 1).
Transthoracic as well as transesophageal echocardiography (TEE) were
negative for ventricular dysfunction, reduced ejection fraction,
valvular vegetations, or intracardiac thrombi, but confirmed the
presence of a PFO. Prolonged ECG monitoring did not
record arrhythmia. Given the negative results of the diagnostic work-up
for alternative embolic sources and the specific MRI findings, CFE was
suspected. The persistence of the NCSE prompted the initiation of
add-on therapy with lacosamide and propofol, but only after
administering thiopentone, seizure control was achieved. Antiepileptic
therapy was progressively tapered until discontinuation and the patient
continued levetiracetam as maintenance therapy. At discharge,
acetylsalicylic acid was reintroduced while Hydroxyurea was
definitively replaced by regular EEX sessions. After six months, she
was seizure-free and showed full physical recovery at the follow-up
visit. Considering her clinical history, the cerebral lesions, and the
right-left shunt severity, the PFO was closed.
Fat embolism
syndrome is a rare complication of SCD. Recently, Tsitsikas et al.[2] identified 87 cases reported in the
literature. This syndrome seems to affect mainly mild forms of SCD and
mortality is highly variable from 33% to 66% depending on the
timeliness and the type of transfusion regimen established.
Pathophysiological mechanisms causing massive bone marrow necrosis
resulting in systemic fat embolism in sickle cell patients are not
completely understood. Sickling red blood cells during a VOC could
result in bone marrow necrosis and subsequent release of fat emboli
into the venous circulation.[3] Fat
globules primarily embolize the lungs, leading to ACS, and thereafter
can enter the arterial circulation through two mechanisms. First, small
fat globules can pass through lung capillaries and reach arterial
blood; second, they can cross a right-left shunt through a PFO
(paradoxical embolism).[4] Thus,
although not necessary for FES, PFO may represent an additional risk
for CFE in SCD patients and its closure may be considered. An
additional pathogenic mechanism of FES includes the hydrolyzation of
fat emboli into circulating free fatty acids (by phospholipase A2),
inducing tissue injury by a secondary production of inflammatory
cytokines.[2]
Typical clinical presentations of FES include pain of unusual severity,
fever, respiratory distress, and altered mental status with or without
other organ involvements.[5] A
definitive diagnosis of FES requires histological confirmation of bone
marrow necrosis or demonstration of fat globules in different organs.[6] However, clinical tools – such as
Gurd and Wilson criteria and Shonfeld Fat Embolism Index – represent
valid approaches to diagnose FES in SCD.[7]
Particularly, this diagnosis should be considered when
leukoerythroblastosis, drop in haemoglobin and platelet count,
increased LDH, C reactive protein, ferritin, and markers of organ
failure are detected.[8] In
addition, brain imaging supports the diagnosis of CFE when the typical
“starfield pattern” on MRI with SWI is detected.[9]
Of note, given the low sensitivity of brain CT in the acute phase of
CFE,[9] MRI with SWI or gradient
echo is superior in the differential diagnosis.
Although the lack of histological data does not allow a definitive
diagnosis of FES, as in our case, the association between acute
respiratory and neurologic symptoms in a patient with SCD, the specific
neuroradiological pattern on brain imaging, as well as the negative
work-up for other embolic sources, should lead to consider this
diagnosis.
Eritroexchange in FES can be lifesaving and data from the literature[2] indicate that it should be started as
soon as FES is suspected of limiting morbidity and mortality.
The institution of a regular EEX regimen after recovery is debated;
however, it is recommended in case of neurological sequelae.[2]
Seizures are a possible neurologic complication of SCD, but status
epilepticus in SCD patients is anecdotal.[10]
Its diagnosis depends on a high level of suspicion and the use of
electrodiagnostic monitoring. Prolonged status epilepticus is
associated with high mortality and requires supportive care,
antiepileptic drugs, sedation, and the management of the causative
condition.