Gianmarco Lugli1,10,*, Matteo Maria Ottaviani2,10,*, Annarita Botta1,10,*, Guido Ascione3,10, Alessandro Bruschi4,10, Federico Cagnazzo5, Lorenzo Zammarchi1,6, Paola Romagnani7,8 and Tommaso Portaluri9,10.
1 Department of Experimental and Clinical Medicine, University of Florence, Florence, Italy.
2 Department of Neurosurgery, University Politecnica delle Marche, Ancona, Italy.
3 Department of Cardiac Surgery, IRCCS San Raffaele Hospital, Vita-Salute San Raffaele University, Milan, Italy.
4 Rizzoli Orthopaedic Institute, University of Bologna, Bologna, Italy.
5
Department of Neuroradiology, Hôpital Gui de Chauliac, Montpellier
University Medical Center, 80, Avenue Augustin Fliche, Montpellier,
France.
6 Unit of Infectious and Tropical Disease, University Hospital Careggi, Florence, Italy.
7 Nephrology and Dialysis Unit, Department of Pediatrics, Meyer Children's University Hospital, Florence, Italy.
8 Department of Biomedical Experimental and Clinical Sciences "Mario Serio," University of Florence, Florence, Italy.
9 IN Srl, Udine, Italy.
10 CEST Centre for Excellence and Transdisciplinary Studies, Turin, Italy.
* These authors contributed equally to this work.
Correspondence to:
Annarita Botta. Department of Experimental and Clinical Medicine,
Infectious and Tropical Disease Unit, Careggi University Hospital,
University of Florence. E-mail:
annarita.botta@unifi.it
Published: January 1, 2022
Received: October 18, 2021
Accepted: December 16, 2021
Mediterr J Hematol Infect Dis 2022, 14(1): e2022012 DOI
10.4084/MJHID.2022.012
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background:
Italy has been one of the countries most affected by the SARS-CoV-2
pandemic, and the regional healthcare system has had to quickly adapt
its organization to meet the needs of infected patients. This has led
to a drastic change in the routine management of non-communicable
diseases with a potential long-term impact on patient health care.
Therefore, we investigated the management of non-COVID-19 patients
across all medical specialities in Italy.
Methods:
A PRISMA guideline-based systematic review of the literature was
performed using PubMed, Embase, and Scopus, restricting the search to
the main outbreak period in Italy (from February 20 to June 25 2020).
We selected articles in English or Italian that detailed changes in the
Italian hospital care for non-COVID-19 patients due to the pandemic.
Our keywords included all medical specialities combined with our
geographical focus (Italy) and COVID-19.
Results:
Of the 4643 potentially eligible studies identified by the search, 247
were included. A decrease in the management of emergencies in non-COVID
patients was found together with an increase in mortality. Similarly,
non-deferrable conditions met a tendency toward decreased diagnosis.
All specialities have been affected by the re-organization of
healthcare provision in the hub-and-spoke system and have benefited
from telemedicine.
Conclusions:
Our work highlights the changes in the Italian public healthcare system
to tackle the developing health crisis due to the COVID-19 pandemic.The
findings of our review may be useful to analyse future directions for
the healthcare system in the case of new pandemic scenarios.
|
Introduction
Since
the first case of the novel coronavirus (COVID-19) was reported in
Wuhan, China, in December 2019, a viral infection spread at an alarming
rate worldwide. On January 30, 2020, the World Health Organization
(WHO) described COVID-19 as a Public Health Emergency of International
Concern, and by March 11, 2020, it was officially declared a pandemic.[1]
Italy was the first European country to be affected by COVID-19, with
the first case being diagnosed on February 20 in a man living in the
province of Lodi (NorthWest Italy).[2] The epidemic
went on to affect all regions in Italy, with higher incidence rates in
the north. The peak of the COVID-19 epidemic in Italy was reached in
the last week of March, with over 5500 new cases per day.
Since
then, there has been a gradual decline due to strict containment
measures that shaped the Italian lockdown phase. However, especially
during the first phase of the epidemic, the outbreak put the Italian
National Health System (Servizio Sanitario Nazionale, SSN) under
unprecedented pressure.
In an attempt to direct the available
resources at counteracting and limiting the effects of the pandemic,
deferrable and non-urgent medical activities were suspended. On the
other hand, patients with life-threatening conditions, such as
myocardial infarction and stroke, or chronic conditions, such as
diabetes, retained the right to their medical needs being met.
In
these circumstances, several medical domains have been constrained by
different resource allocations with unpredictable long-term
consequences on patient health care.[3-5]
Here,
we present a systematic review of the literature, which illustrates the
direct and indirect effects of the COVID-19 pandemic on the management
of non-COVID patients across all medical specialities.
Methods
This systematic review was performed in accordance with PRISMA guidelines.[6]
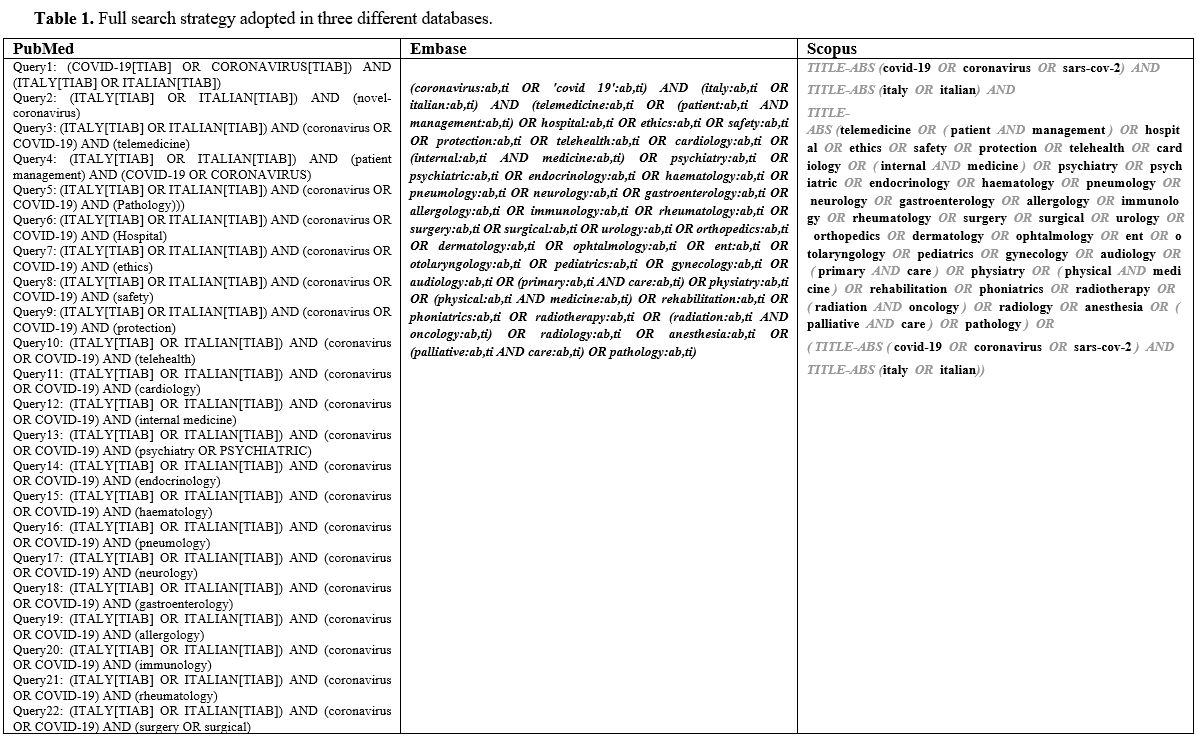
The search was conducted on June 25 2020, on three databases: PubMed,
Embase, and Scopus, without any date restriction. All the keywords were
investigated within the title and abstract in both "AND" and "OR"
combinations. Our keywords included all medical specialities (and
potential synonyms) combined with our geographical focus (Italy or
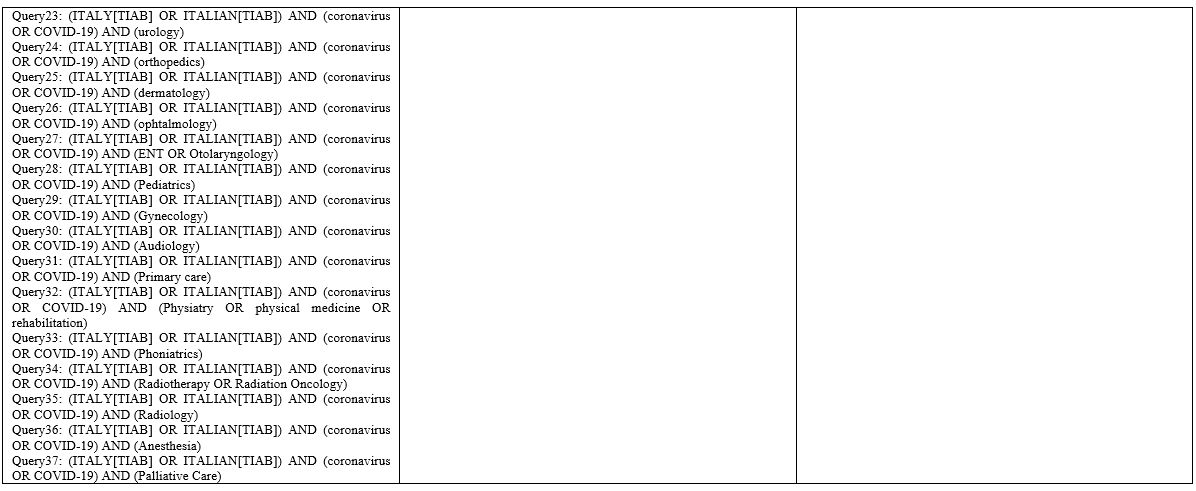
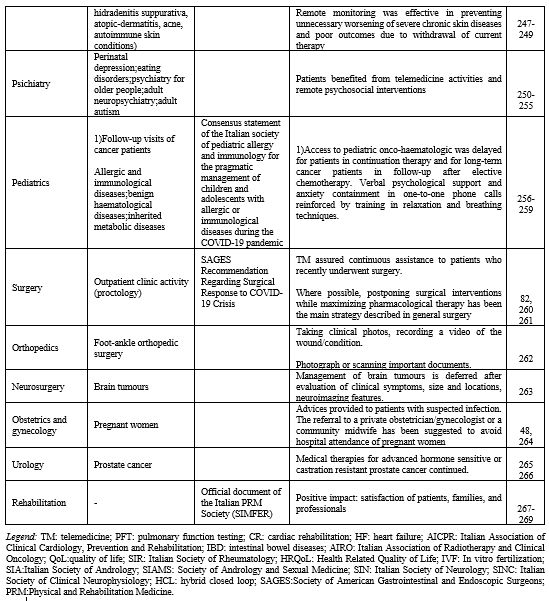
Italian) and COVID-19. The full search strategy is reported in Supplementary Material Table 1. Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Selection of the Studies. The
literature search returned original papers published between 1979 and
2020 – especially for the keyword "coronavirus". Since our focus was
the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
and the first positive case in Italy was detected on February 20, the
literature search was restricted to the period from February 20 to June
25 2020. The databases were queried via an R script on their respective
APIs, checked and cleaned for duplicates (via title, DOI and/or
database id), and exported into Excel.
In the second stage,
studies were selected based on their titles and abstracts: each study
was independently evaluated by three different raters (AnB, GA, GL).
When there was a lack of agreement among the screeners, ensemble
majority voting was used for the final decision. The full texts of the
selected papers were thus analyzed by two reviewers in terms of
relevance and inclusion/exclusion criteria (MMO and GA). When these
reviewers disagreed over the inclusion or exclusion of a paper, a third
reviewer was responsible for the final decision (GL). In addition, the
reference lists of selected papers were reviewed in order to find
pertinent studies not identified during the initial search.
Inclusion and Exclusion Criteria.
The simultaneous co-occurrence of the following characteristics was
considered for the inclusion of articles: (i) articles focusing on the
SARS-CoV-2 infection/COVID-19 disease; (ii) articles focusing on the
impact on patients based in Italy or on the Italian hospital
organization; (iii) articles detailing COVID-19-associated changes in
the Italian hospital care for non-COVID-19 patients. All the
investigated articles were published in English or Italian.
Type of Studies.
Original papers, editorials, comments, research letters, case series,
and studies focusing on non-COVID patients in Italy were included.
Data Extraction and Quality Assessment.
Data were extracted from the papers by one of the investigators (TP)
and were subsequently checked for accuracy by other reviewers (GL,
AnB). Disagreements regarding data extraction among reviewers were
solved by consensus. Extracted data included: type of medical specialty
involved (surgical, medical, or public health), geographical location
(north, south, centre or nationwide), type of patients
(COVID/non-COVID), type of study (article or research
letter/comment/editorial). Unfortunately, no quality assessment was
possible as over 32% of entries were not articles but consisted of
comments, research letters, opinions or editorials – for which no
quality guidelines are available.
Investigated Outcomes.
This systematic review investigated the impact of the COVID-19 pandemic
on patients' healthcare provision and hospital organization in Italy
since the day the country was put in lockdown.[7] Our
primary goal was to identify potential short-term and long-term effects
on the health of non-COVID patients. Our secondary goals were to
identify: (i) organizational and/or clinical settings and decisions
that were particularly effective (or counterproductive) during the
pandemic; and (ii) similarities and differences across medical
specialities and regional areas.
Results
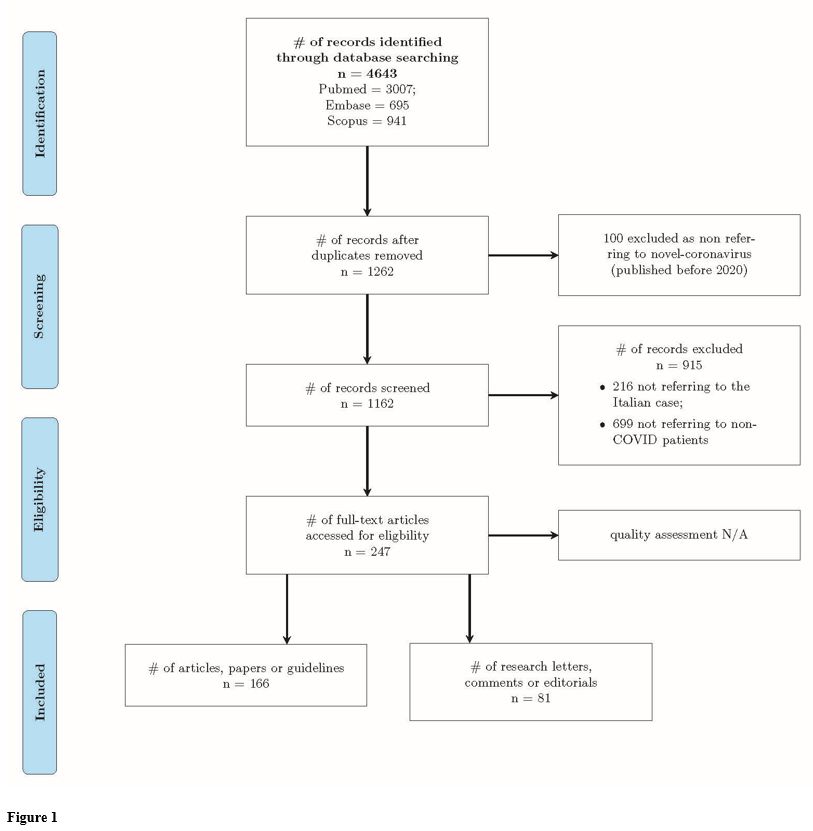
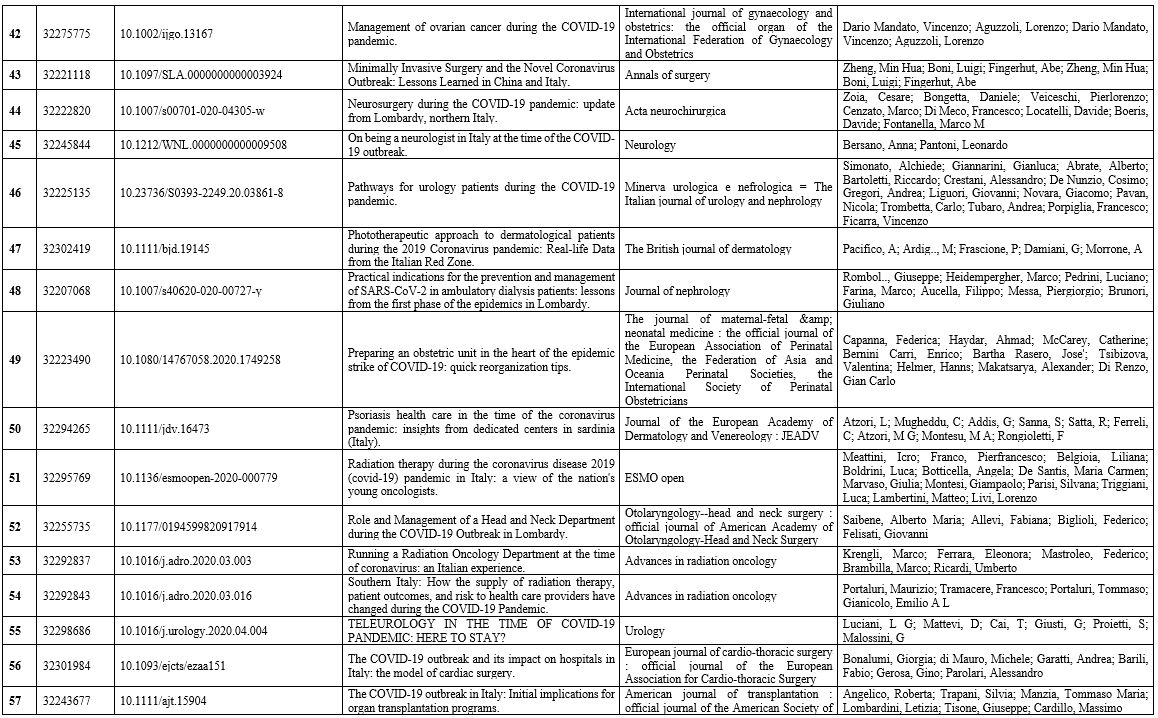
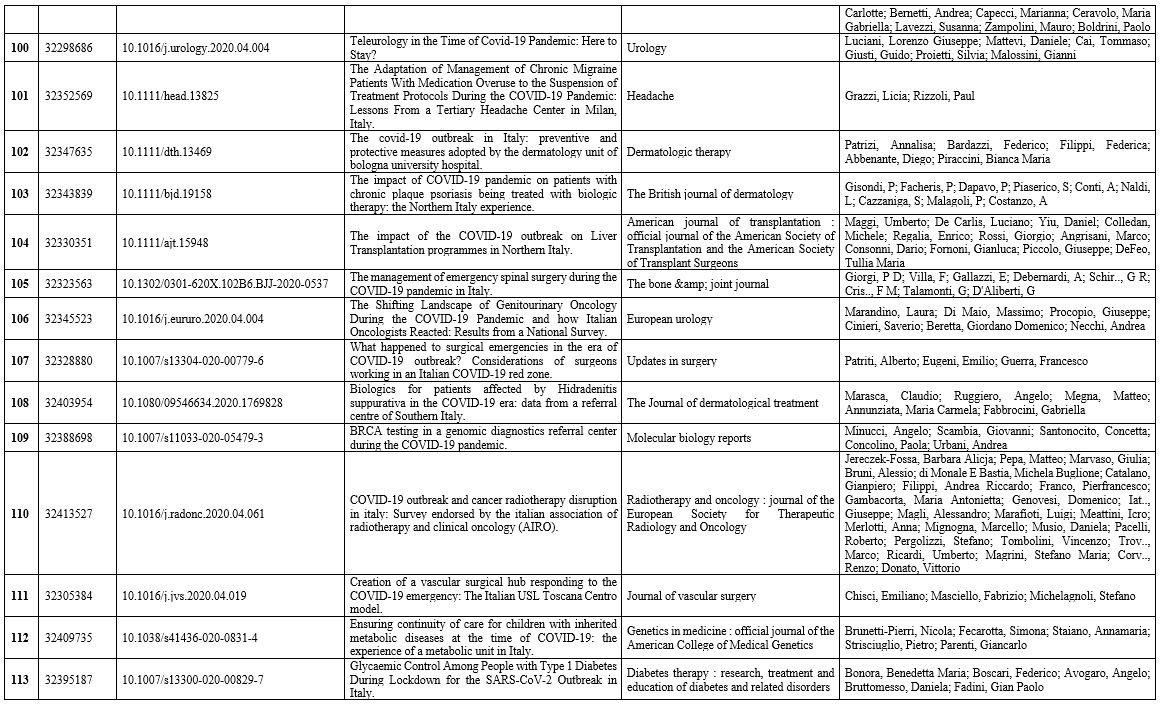
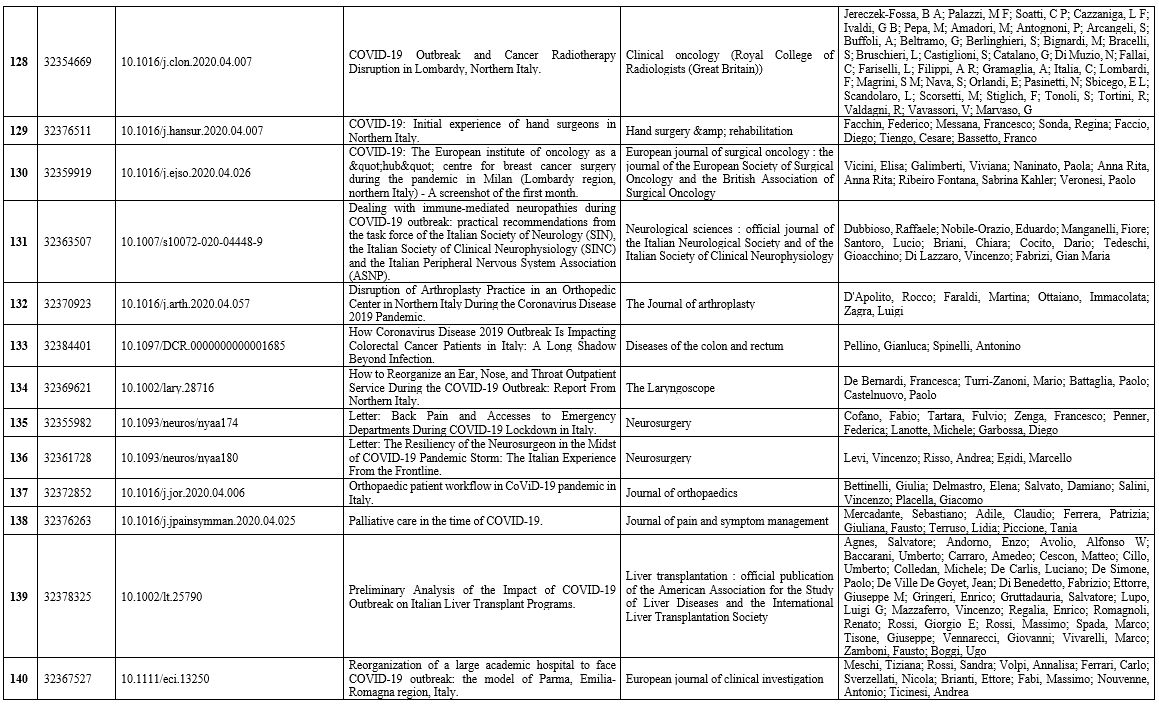
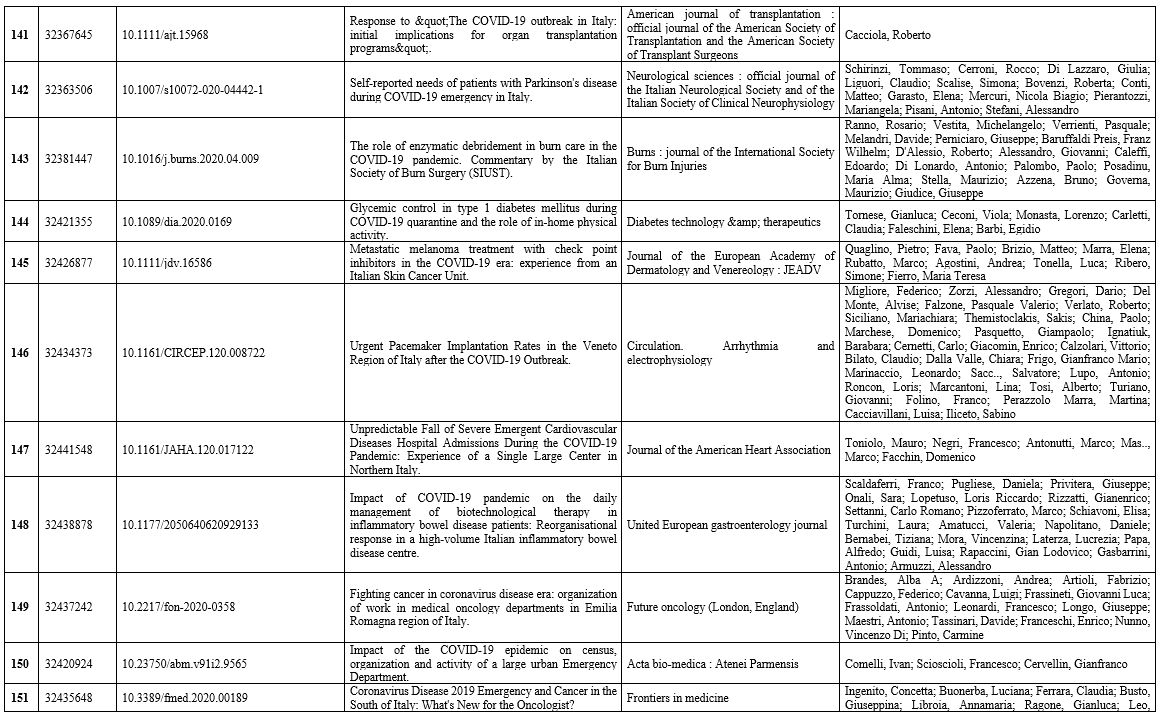
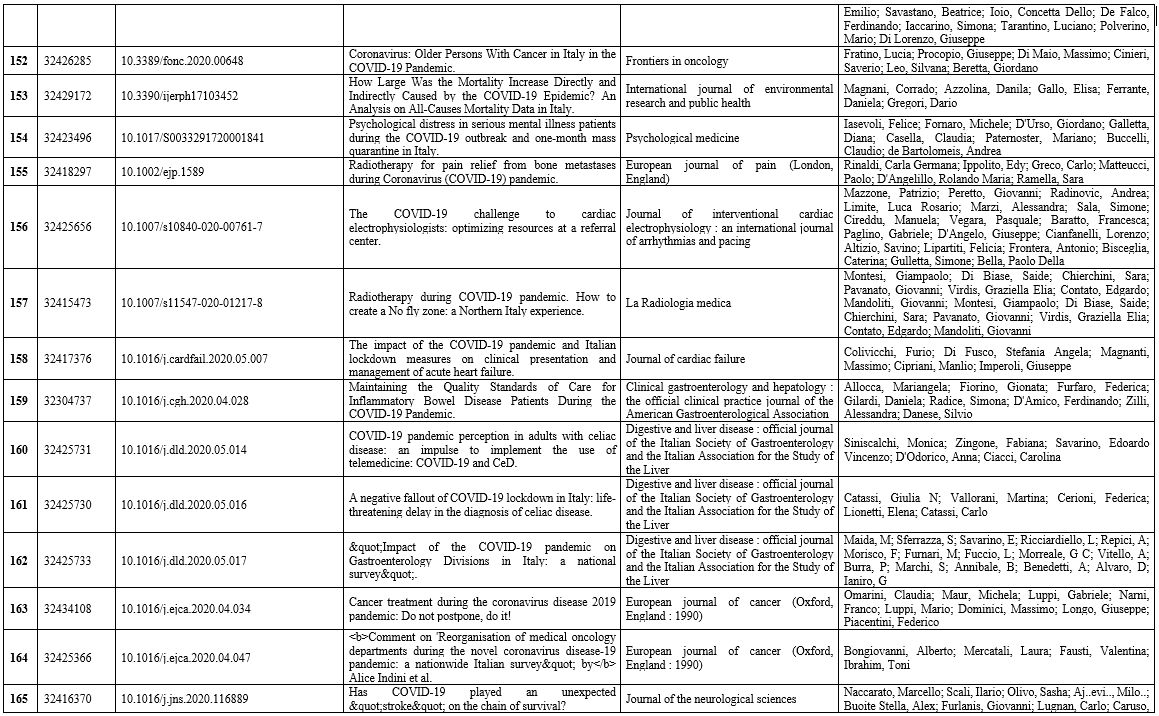
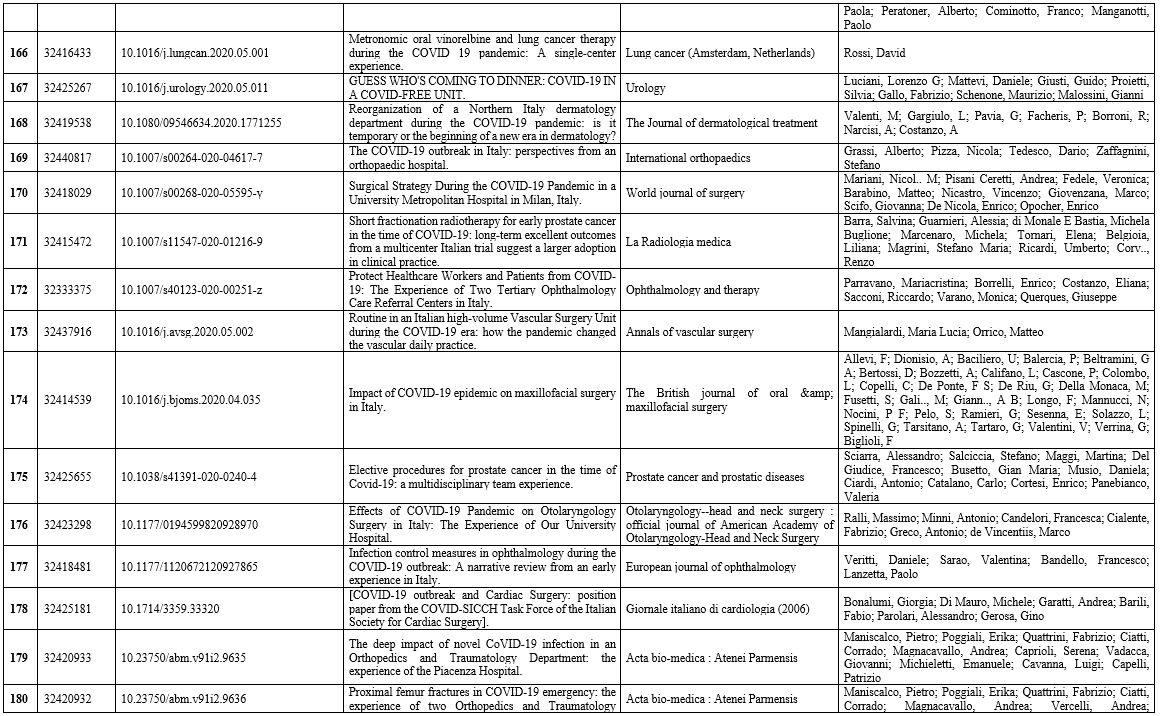
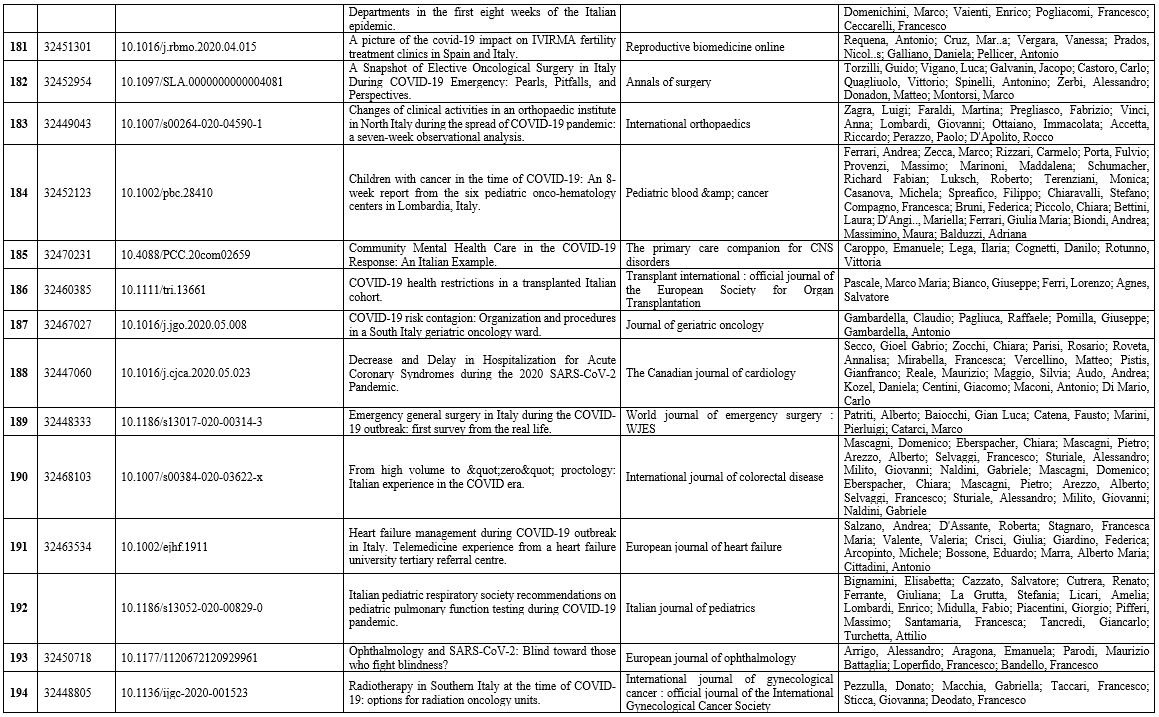
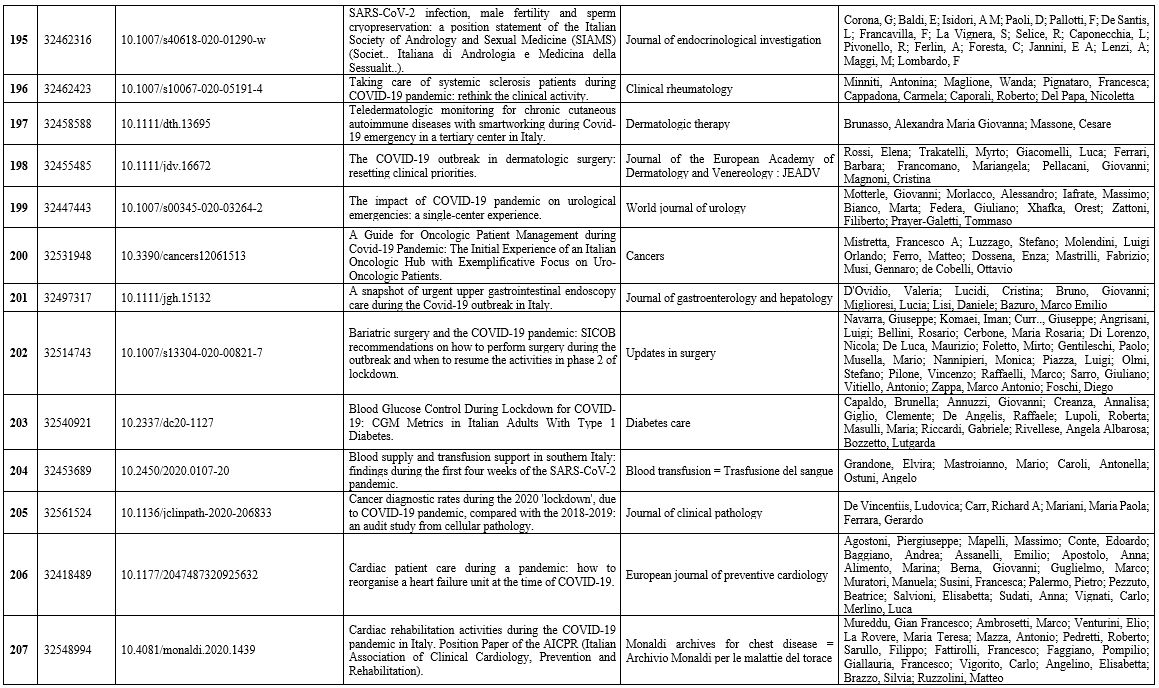
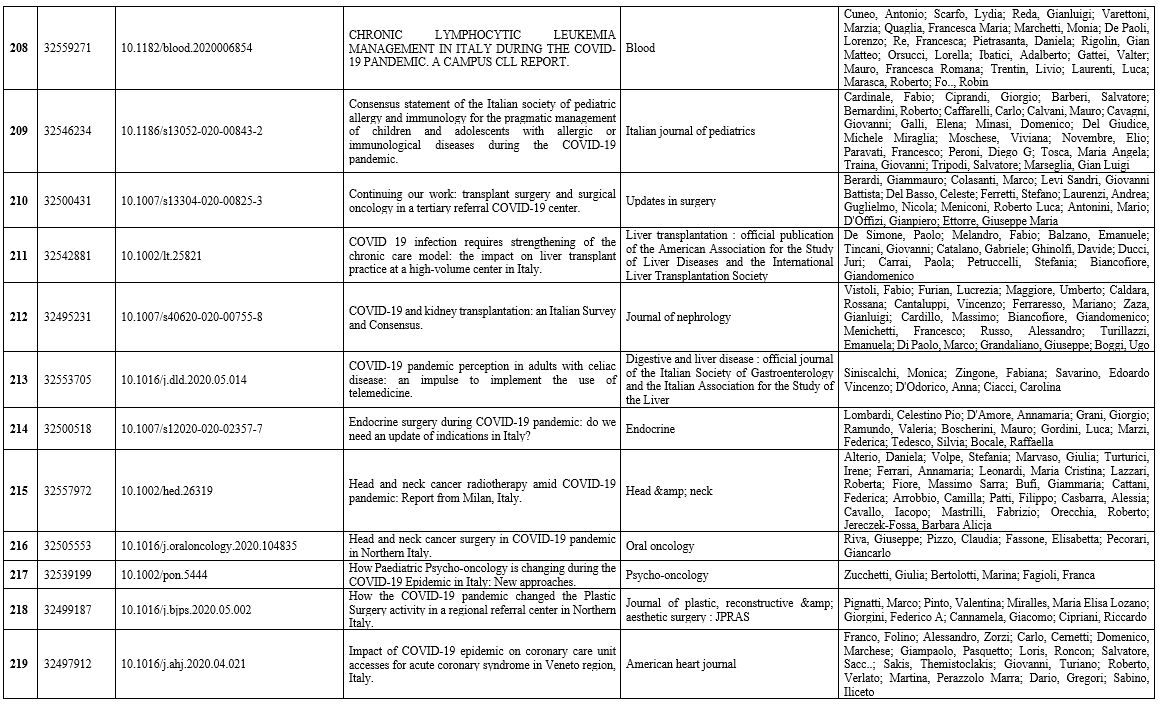
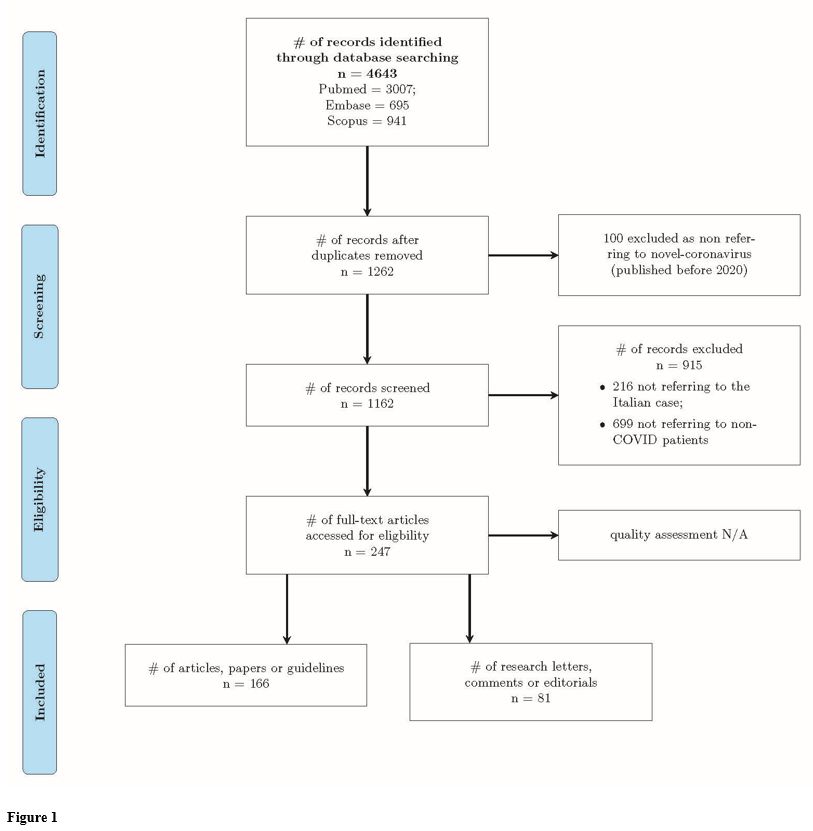
The results are shown in Figure 1.
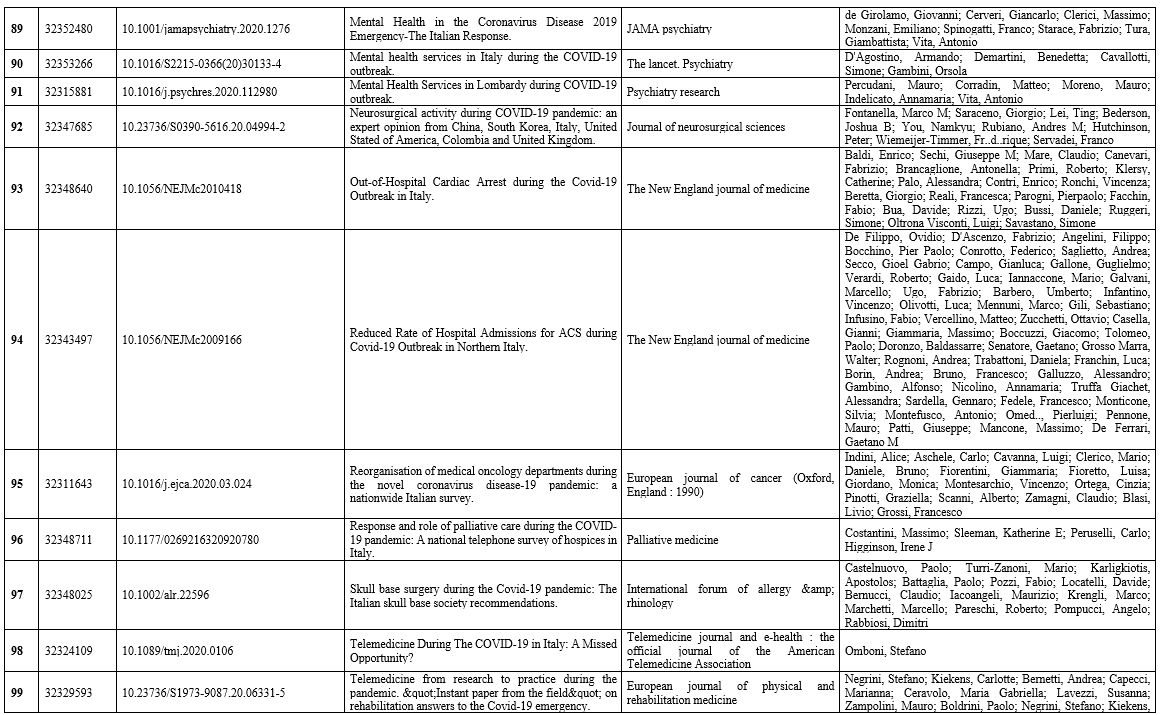
After searching the databases, we identified 4643 papers from three
different databases. Database merges and the removal of duplicates
resulted in 1262 records, of which 100 were immediately removed as they
were not related to COVID-19 (articles published before the pandemic in
Italy). A total of 1162 records were then screened: 166 were removed as
not relevant to Italy; 534 were removed as they referred to COVID-19
patients rather than non-COVID-19 patients. A total of 247 were deemed
eligible, of which 81 consisted of comments/letters/opinions/editorials.
Oncology
and radiotherapy were the most represented category (47 papers),
followed by surgery (24 for general surgery, 9 for neurosurgery, 2 for
cardio-surgery, 2 for vascular surgery, and 3 other types), cardiology
(19), and dermatology 14. There was one paper each for rheumatology and
microbiology.
 |
Figure
1
|
Overall,
133 papers were related to clinical disciplines, 89 to surgery, and 24
to services. In terms of geographical distribution, many papers
provided general recommendations without a specific geographical
identification (75). Lombardy was the most represented region (72),
followed by Lazio (21) and Emilia Romagna (15). In the south, Campania
was the most represented region (11), followed by Puglia (4). Marche,
Piedmont and Friuli Venezia Giulia had 7 papers each, Tuscany and
Veneto 9 each. Overall, 73 were general/nationwide, 105 pertained to
northern regions, 54 to central regions, and 15 to southern regions and
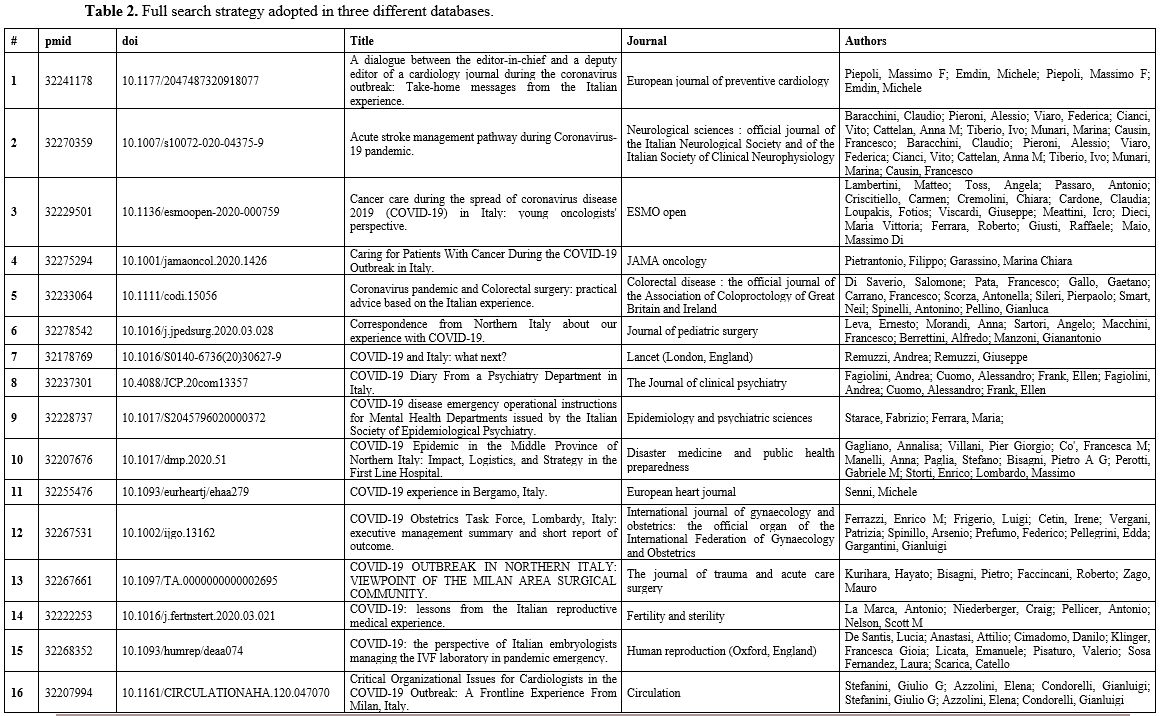
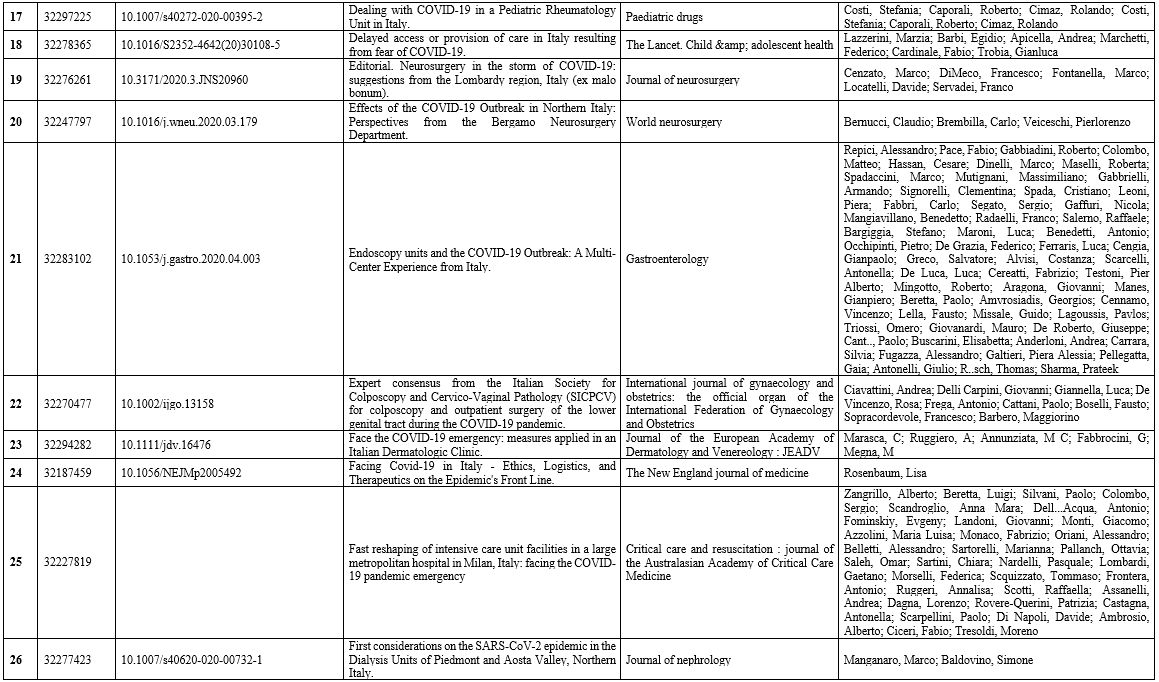
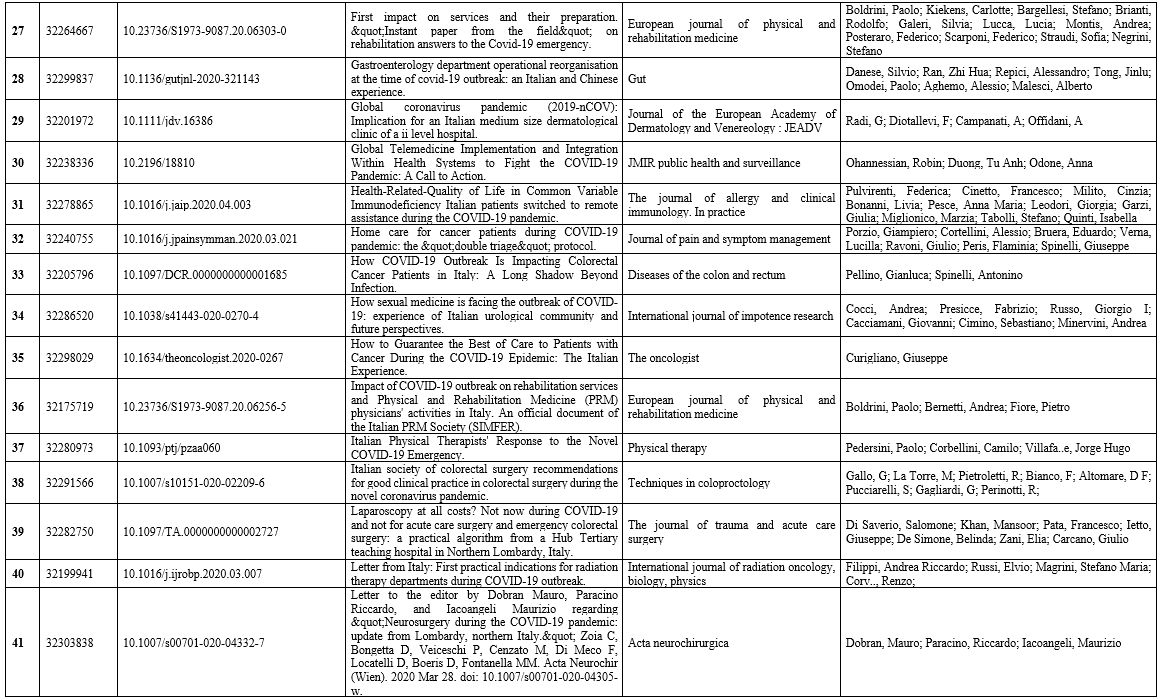
islands. The studies included are reported in Supplementary Material Table 2.
Management of Emergencies. In general, non-COVID patients admitted to emergency departments (ED) decreased and remained well below the standard levels.[8-11]
The youngest age classes declined dramatically, while the oldest age
classes progressively increased, remaining considerably above the
standard rate of the local ED.[12]
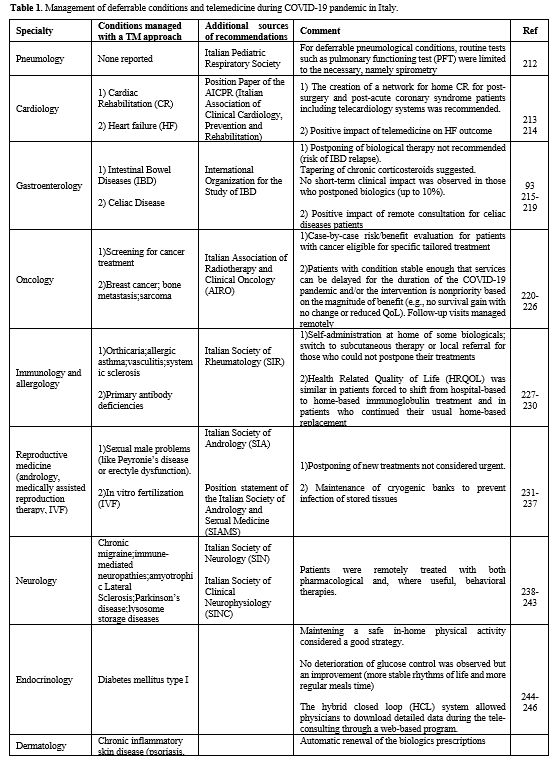
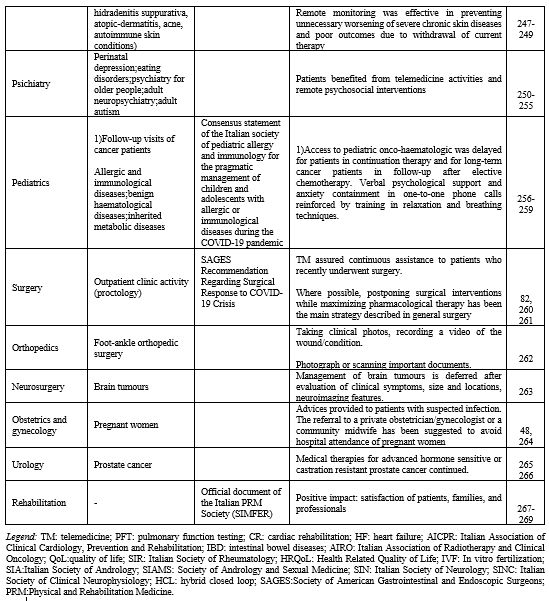
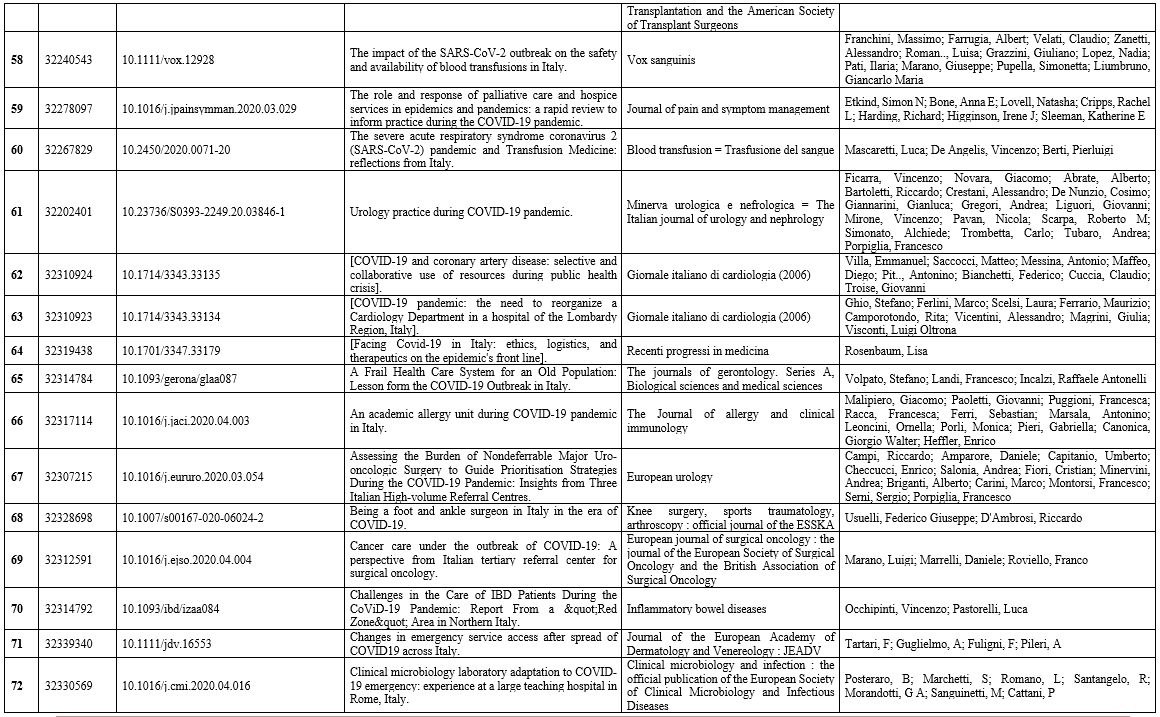
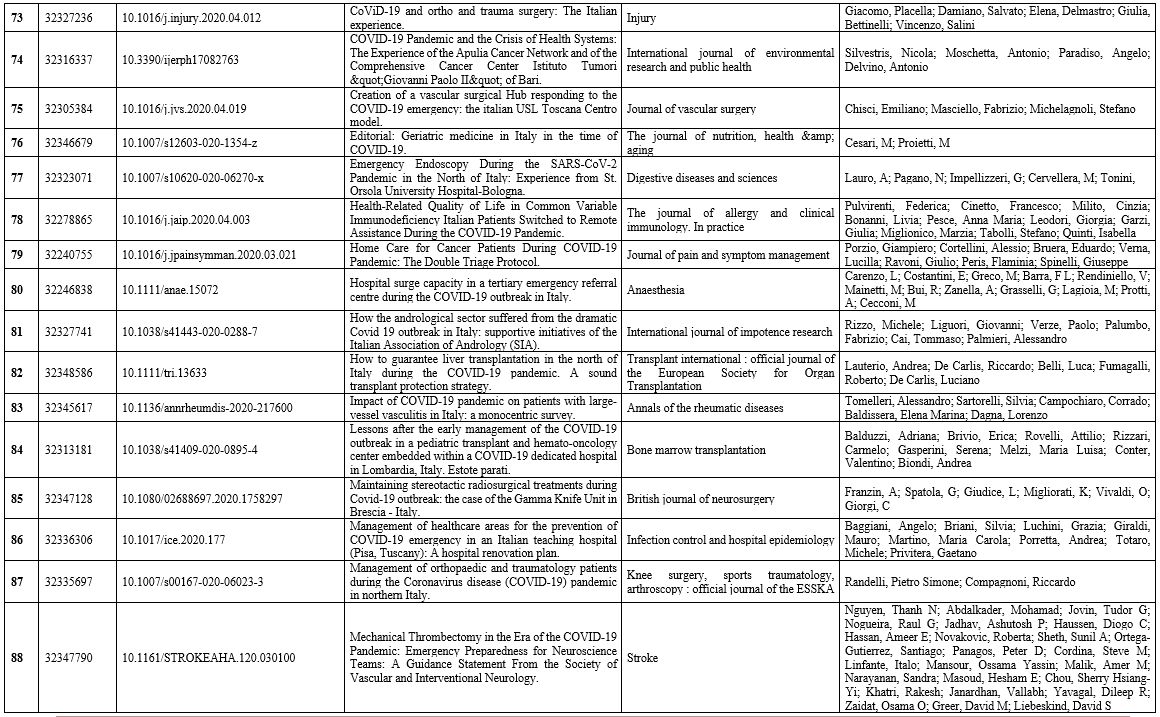
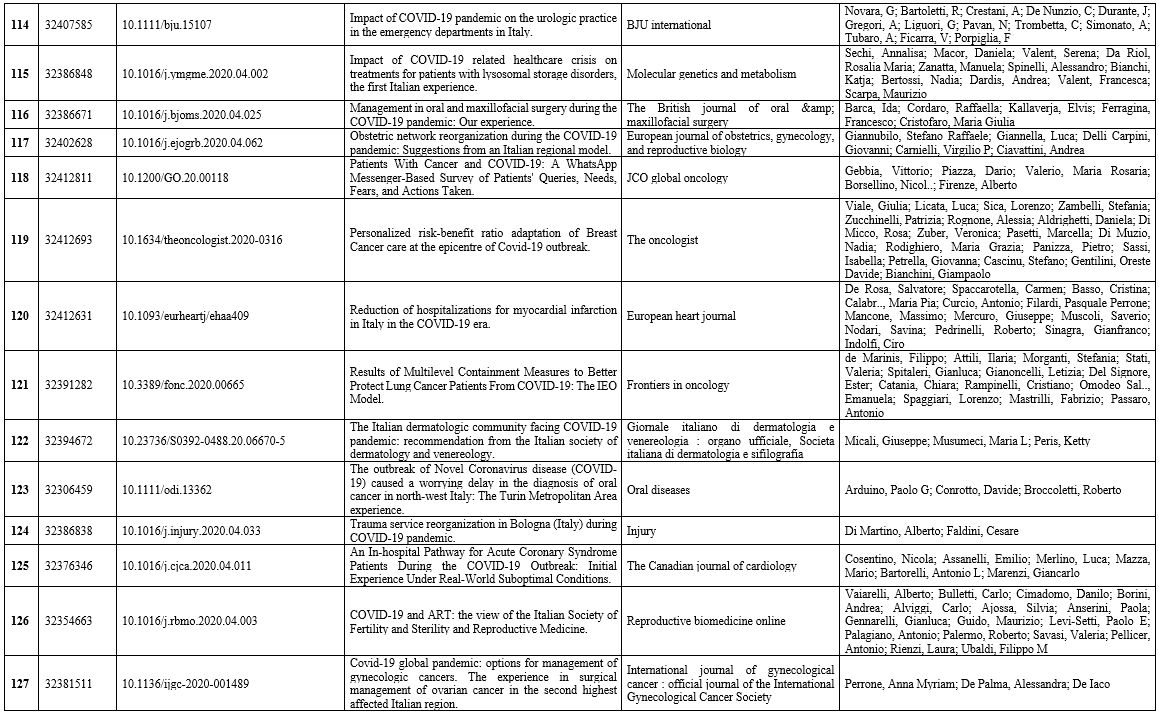
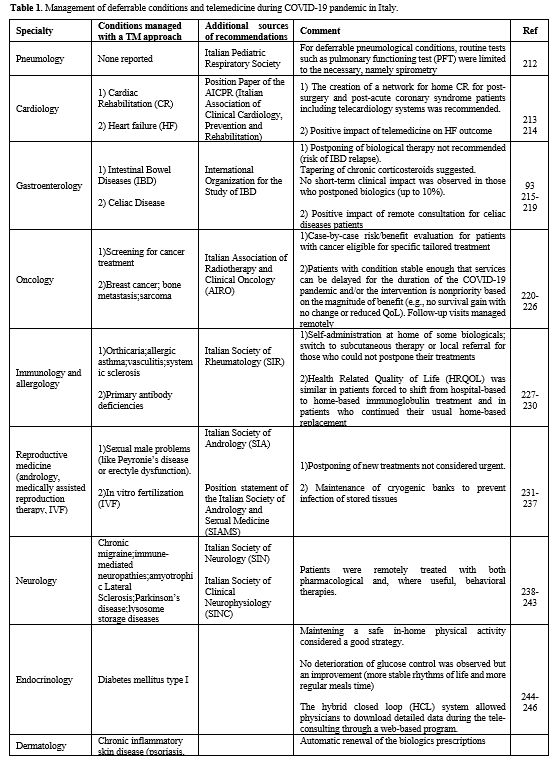
Table 1 shows
the most relevant data regarding cardiovascular emergencies, including
stroke. In northern Italy, the emergency gradually took over most
cardiology intensive care units (ICUs).[13] As
expected, the net effect of this re-organization was a significant
reduction in sites and staff committed to the treatment of
cardiovascular diseases. [14-18] Comparing
out-of-hospital cardiac arrests in the same period of the previous
year, Baldi et al. found that the median arrival time of the emergency
medical service was three minutes longer in 2020, and the proportion of
patients who received cardiopulmonary resuscitation from bystanders was
15.6% lower. Among patients in whom resuscitation was attempted by
emergency medical services, the incidence of out-of-hospital death was
14.9% higher in 2020 than in 2019.[9] This finding was
confirmed by additional studies highlighting an unpredictable decrease
in acute coronary syndrome-related hospitalization in high-volume
centres[10,19,20-21] and pacemaker implantation during the weeks following the COVID-19 outbreak.[21-25]
 |
Table
1. Management of deferrable conditions and telemedicine during COVID-19 pandemic in Italy. |
 |
|
Of note, one study showed a 49% reduction in acute heart failure admission to the hospital.[26]
The patients admitted had longer door-to-balloon and symptoms to PCI
times, higher hs-cTnI levels at presentation, lower residual left
ventricular function at discharge, and higher predicted late
cardiovascular mortality on the GRACE score.19
Two studies[11,27] also reported fewer patients with minor strokes and transient ischemic
attacks (TIAs), longer onset-to-door and door-to-treatment times for
major strokes, and reduced transfers from spokes centres. As a result,
the number of patients who underwent intravenous thrombolysis or
bridging therapy (combined intravenous and thrombectomy) decreased by
− 26% and −30%, respectively.
In addition, as a consequence of
the reduction in the patient eligibility for bridging therapy, the
number of primary thrombectomies (performed with all the necessary
personal protective equipment owing to the risk of infection)[28] increased by 41%. Most of these patients had very serious strokes that would have benefited from early diagnoses.[11]
The decrease in hospital admissions, confirmed by a survey across multiple countries, including Italy,[29,30] resulted in increased door-to-needle times and missed therapeutic windows for patients suffering from severe strokes.[31]
The
reduction in available Intensive Care Units (ICU) beds, massively
dedicated to COVID-19 patients with acute respiratory failure, and the
fear of infection resulted in the shrinkage of surgical activities in
all fields[32-36] and a reduction in urgent endoscopic procedures in COVID-free hospitals.[37]
Each
sub-speciality defined various non- deferrable surgical procedures that
had to be guaranteed, causing a drop in consultations requested by
emergency departments, as in the case of urgent urology.[38]
The surgical community also faced a shortage of blood components
derived from fewer donations due to lockdown and fear of infection.[39]
To compensate for the initial fall (−10%) in blood donations in the
first week of March, the government promoted a national media campaign
on the importance and safety of blood donation as a priority to
maintain basic healthcare services for non-COVID patients.[40] No blood-transmitted SARS-CoV-2 infection has been reported to date.[41]
Children's emergency departments also showed a substantial decrease in visits,[42]
and that might reflect the scarcity of resources or the reluctance of
parents and health care workers to expose children to the risk of viral
infection in a healthcare setting, in addition to lower rates of acute
infections and trauma.[43] However, this phenomenon
has been detrimental to the health of non-COVID child patients: 12
cases of delayed access to hospital care were reported during the week
of March 23–27 across five hospitals of an Italian Children's Hospital
Research Network. Half of the children were admitted to an ICU, and
four died, highlighting the high risk of delaying access to hospital
care.[44] As a result, life-threatening conditions
(i.e. abdominal pain, severe ketoacidosis) seemed to be more frequent,
requiring, in some cases, an aggressive approach.[43]
The same phenomenon affected dermatology.[45]
Tartari et al. compared two different weeks, before and after the
outbreak of the COVID-19 pandemic in Italy, showing a decrease in
unjustified referrals (93% reduction) in dermatological emergency
services.[46]
Despite medical care for
emergencies and urgent treatments being continuously provided
throughout the pandemic, the lack of personnel, resources, and ICUs
beds and the patients' fear of being infected in hospital affected
patient management and substantially delayed the provision of ordinary
medical activities. These initial data seem to show a decrease in
emergencies and an increase in mortality.
Management of Non-Deferrable Conditions:
the Hub-and-Spoke System. To tackle the massive impact of the overflow
of SARS-CoV-2 infected patients, hospitals in Italy had to undergo a
significant re-organization.[47-52] In order to
manage conditions needing non-deferrable treatment while avoiding the
risk of infection, hub-and-spoke centres were created and widely used
throughout the country.[48,53-56]
In the hub-and-spoke model, the main campus or hub supplies the most
intensive medical services, while satellite campuses or spokes offer
more limited services at sites distributed across the neighbouring
area.[57]
Neurological surgery was particularly
affected by the ICU re-organization, as it often requires a period of
intensive monitoring in ICUs.[22,58-60]
All the cases of elective neurological surgery were deferred, while
urgent neurosurgical pathologies (above all traumas) and non-deferrable
tumour cases were transferred to hubs.[27,29-33,61-63]
Some
minimal activities were still performed at spoke centres, only for
critical cases or when specific tools were required (i.e. gamma knife
treatment of neoplastic lesions).[64-67]
This
provided an unprecedented opportunity for transversal collaboration
among different teams, representing real innovation in such a
competitive setting.[56,62]
A
hub-and-spoke system was also organized for vascular surgery and
cardiac surgery units. All elective surgery was reduced, and urgent
surgery (including aortic aneurysms, valvular diseases or severe
coronary diseases) was performed only in hub centres, preferring the
endovascular to the open surgical approach whenever possible.[68-70] A transcatheter approach was generally preferred, as it usually does not require an ICU bed or a ventilator.[69]
The limitation of all non-urgent surgical activities also applied to general surgery[71-76] and obstetrics.[76,77] In highly-infected areas (such as Lombardy), hub centres were created[78] to treat only advanced symptomatic tumours,[78-80] while elective oncological surgery procedures continued to be performed in less-affected regions.[78,81] This was an important issue for oncological patients, especially the older ones.[82-85]
Many
possible ways of minimizing the risks were proposed: to postpone
treatments or elective surgery for stable cancer in endemic areas,
provide patients with greater personal protection, and offer more
intensive surveillance or treatment.[86-88] For example, neoadjuvant treatments were recommended or increased to defer surgical admission for as long as possible.[78,81,89-90]
For other medical conditions requiring surgery under particular
circumstances, such as relapse of inflammatory bowel disease, dedicated
hubs were identified.[91-93]
Interestingly, a tendency toward treatments to reduce hospitalization was also found in medical oncology.[94,95]
Some regions such as Tuscany created home care protocols to avoid exposure to hospital settings.[96] Oncological care delivery and cancer diagnosis[97-99]
were dramatically reduced by the SARS-CoV-2 outbreak, even though
suboptimal care and treatments may result in worse cancer‐related
outcomes. Oncologists were thus asked to preserve patients' continuum
of care while adopting mitigation strategies to reduce the likelihood
of infection in all cancer patients.[100-109]
Arduino et al. described a worrying delay in diagnosing oral cancer in northwest Italy during the Covid pandemic.[110] Moreover, the cessation of elective activities, screening programs,[111]
and the drastic reduction in services regarding breast cancer
restricted evaluations to only clinical observations of palpable
lesions with the elevated risk of missing new diagnoses.[112]
Although not requiring a structural re-organization, palliative care
was forced to find a new balance between family member visits and
patients' needs.[113-116]
In orthopaedics, the
re-organization led to the identification of poly-specialist major
trauma centres and specialistic referral centres for minor trauma or
non-deferrable orthopaedic surgeries (i.e. septic arthritis or
malignant tumours).[117-124] There was a reduction
in the number of proximal femur fractures in two centres, as well as a
reduction in hip and knee arthroplasties.[125,126]
A
similar re-organization was also carried out for plastic surgery: only
post-traumatic, oncological and burn treatments were guaranteed.[127-129] A new approach based on enzymatic debridement was proposed for burns to reduce the need for burn surgery.[130]
In
urology, only urgent, non-deferrable procedures (colicky flank pain,
gross hematuria and acute urinary retention) were authorized after
careful multidisciplinary evaluation, which led to a drop in urological
surgical activities.[131-136] Whenever possible,
alternative treatments not requiring general anaesthesia (i.e.
radiotherapy for genitourinary cancers) were suggested as preferable.[131,133,137]
Oral
and maxillofacial surgery, otolaryngology, and ophthalmology also
suspended all non-urgent treatments, especially considering healthcare
workers' high risk of infection while manipulating the upper airways
and eyes.[138-145] Only the treatment of trauma, malignant neoplasms, and severe infections was guaranteed.[139,146-149]
In the context of radiotherapy, all follow-up visits involved a phone call in advance in order to postpone non-urgent cases.[150-153]
The initial consultations of patients needing treatment for malignant
tumours were conducted as normal, as were certain treatments such as
bone metastases radiotherapy.[154-157] Specific approaches, such as short fractionated radiotherapy, were suggested.[158]
All
non-urgent and deferrable radiation treatments were delayed, while
therapies for patients with better prognoses (benign and functional
diseases) were postponed.[159,160]
Dermatology departments were also involved in an extensive re-organization.[161-162]
Dermatological anti-neoplastic treatments were provided in the
dermatology clinics of many centres, such as Bologna, Naples, Modena
and Ancona, which also maintained urgent dermatological procedures and
consultations required by other hospital wards.[163-166]
As awareness of the severity of the COVID-19 increased, some patients
were concerned about continuing their medications; however, all centres
followed specific recommendations and advised patients not to suspend
these drugs without consultation.[167-170]
Lastly,
microbiology labs underwent unprecedentedly high workloads with the
increasing number of samples (swabs or serological tests) to analyze
for the identification of Sar-Cov-2 infection. An extensive
re-organization of the microbiology lab activities thus also occurred.
In a large teaching hospital in Rome, the introduction of night shifts
and the creation of a dedicated team significantly improved the number
of samples processed without interfering with the daily laboratory
routines.[171]
Replacement Therapies: Dialysis and Transplantation.
Dialysis units experienced a profound change in their management with
the introduction of COVID-19 isolation rooms and the identification of
dedicated healthcare professionals.[172,173] Rombolà et al. proposed three actions to be taken in order to dialyze
non-COVID patients safely: hygiene measures, the use of PPE to protect
patients and the healthcare team, and the protection of the dialysis
ward with an isolated area for testing patients suspected of infection.[174]
In general, all transplant programs were profoundly affected by the pandemic.[175-177]
First of all, the wall-to-wall screening of donors and recipients was
established to identify positive patients who would not be able to
donate or receive blood, in view of the high mortality rates COVID-19
in immunocompromised patients.[177-180] Secondly,
the widespread reduction in available ICU beds led to an estimated 15%
drop in transplants compared with the last five years' average, such as
liver transplantations.[177,181]
transplantation was thus suggested only in true end-stage organ
failure, preferring conservative treatments (maximizing pharmacological
therapy) in all other patients.[181-184]
Management of Deferrable Conditions and Telemedicine. The management of chronic conditions also suffered.[185]
Cesari et al. found that the integration of care services collapsed:
admissions to post-acute/long-term care facilities were reduced, and
several person-tailored interventions were suspended – e.g., physical
therapists for mobilization.[183] Lasevoli et al.
reinforced the view that the current pandemic has had dramatic
consequences for the mental health of serious psychiatric patients.[186]
All this inevitably led to a drastic reduction and a substantial
re-organization of the clinical activity in many specialities (Table 1),
postponing elective treatments and switching to telemedicine (TM) for
consultation or not to leave vulnerable high-need patients without
proper follow-up.[187-188]
The implementation
of TM occurred in different ways and to varying degrees depending on
the specific centre and specialty. An online questionnaire administered
to the 176 Directors of Italian Radiation Oncology Departments revealed
that to guarantee the continuity of care, in 78 centres (62.4%)
activated telematic consultations for RT treatments.[152]
A similar survey for RT centres in the Lombardy region revealed that
84% of RT facilities cancelled out-patient follow-up visits, 68%
activated telematic consultation and 30% adopted working from home
solutions.[153] Another survey administered to 122
medical oncology departments homogeneously distributed on the national
territory revealed that in 72% of cases, alternative ways to get in
touch with patients had been used, like telephonic interviews with the
interpretation of laboratory and radiologic examination reports.
According to Pietrantonio et al., WhatsApp turned out to be adequate to
give a rapid answer to most queries from oncologic patients.[105]
Brunasso et al. started a teledermatology service in smart working
using phone calls and e-mails by which they could monitor almost 94% of
their patients.[189] In a Department of Urology in Northern Italy, 55% of cases were screened undergoing telephone consultation.[190]
TM
has been shown to have beneficial impacts on heart failure outcomes in
a comparative analysis between 2020 and 2019 by Salzano et al.[191]
Finally, TM positively impacted patients' life as documented by a
survey in which 85% of patients were satisfied with the remote
interview modality and the reduction of economic and time costs related
to going to the clinic. Most of those subjects (90%) expressed their
willingness to continue to be included in remote evaluation programs.[192] Almost all specialities benefited from TM during the pandemic. The results are summarized in Table 1.
Discussion
On March 11 2020, the World Health Organisation (WHO) declared the COVID-19 pandemic.[1]
However, Italy was already in lockdown, with decrees limiting mobility
and strengthening the National Health System. On March 9, 2020, most
outpatient services were temporarily suspended, except for a few
treatments that were considered urgent and non-deferrable.[7]
Clinical support for early isolation, treatment, and, where needed,
intensive care of COVID-19 patients (or suspect cases) became the
priority, with a massive allocation of dedicated resources.
A
large increase in all-cause mortality was revealed during the epidemic,
greater than the number of deaths attributed to COVID-19 cases. The
possible causes of this increase include a large number of severe
undiagnosed COVID-19 cases, reduced access to health services due to
the disruption of normal working processes, or the fear of
contamination of sick patients affected by other diseases and possibly
other factors.[8]
We provided a snapshot, across
all medical specialities, of how the provision of treatments to
non-COVID patients in Italy has been impacted by the shortage of
resources imposed by the pandemic.
Measures put in place to
mitigate the outbreak, such as social distancing and confinement,
contributed to discouraging access to the emergency department (E.D.)
all over the country and those conditions requiring urgent care. As a
result, there was a significant decrease in overall E.D. admissions and
a substantial reduction in all-speciality surgical consultations.[9-11]
More studies are needed to confirm these data and to evaluate the
impact on death rates; however, recent reports from other countries
seem to confirm this trend.[193,194] Cardiovascular emergencies paid significant tolls with a significant delay in time-sensitive emergency operations.[9-19]
More recent evidence, consistent with our results, showed a significant
decrease in the mean number of endovascular therapies per hospital
performed before and after COVID-19 confinement along with a
significant increase in mean stroke onset-to groin puncture time.[195] A delayed presentation of STEMI patients that may lead to worsened prognosis and unnecessary deaths has also been observed.[196]
Moreover, an additional study confirmed that more in-hospital
cardiovascular deaths occurred in March 2020 compared with March 2019,
a finding due to late hospital presentations and consequent greater
disease severity that affected eligibility and outcome of
cardiovascular procedures[197]
As stated
before, the hospitalisation system was remodelled to allocate
appropriate resources to manage patients with COVID-19; consequently,
hubs were identified for specialised medical activities. Hub-and-spoke
centres represented an important change in care provision, especially
in the most affected regions, involving almost all specialities.
However, data on the efficacy of this reorganisation, measured in terms
of health outcomes (such as mortality), are lacking. To date, only a
few reports suggest a tendency toward a decrease in diagnosis for
non-deferrable conditions despite the hub-and-spoke organisation.[98,100,111]
Cautious and evidence-based studies are needed to properly assess the
overall impact of this model on measurable outcomes. Nevertheless, the
hub-and-spoke system seems to be a valid model, at least, in the
management of ischemic emergencies.[198]
A
pandemic is a dynamic scenario, requiring reorganisation and
flexibility of healthcare delivery. T.M., which consists of
distributing health-related services and information via
telecommunication technologies, proved a pragmatic approach to managing
deferrable conditions during the COVID-19 pandemic in Italy. Moreover,
TM allows for more flexibility on the side of both the clinician and
the patient, as consultations can easily be rescheduled, and meetings
can be held from home.[199] Notably, when looking at
the world scenario, T.M. is thought to play an important role in
delivering digital health to the general population.[200]
Almost
all specialities benefited from T.M. during the pandemic, with
short-term results particularly encouraging in some cases. The pandemic
has generally demonstrated that information technologies should be more
promoted independently from this specific context.[153] However, a longer follow-up is needed to assess the efficacy of these measures on common health outcomes.[199-201]
Avoiding face-to-face contact via T.M. has been one of the most
effective measures to limit the spread of SARS-Cov-2 infection,
although many issues have been raised, such as privacy management and
the lack of clear guidelines.[202-206] We strongly
encourage overcoming these limitations to promote further the multiple
opportunities of T.M. in tune with its pivotal role during the second
phase of the COVID-19 pandemic in Italy.[207] T.M.
has deeply influenced non-COVID patient care, enabling the remote
diagnosis and monitoring of patients and allowing clinical data sharing
between patients and physicians.[208,209]
One
limitation of this systematic review is the heterogeneity in
publication type, which prevented the execution of a meta-analysis to
summarise the findings together with a quality assessment. Another
important issue is the potential underreporting, although the studies
covered the whole country's experiences. Finally, while also providing
a snapshot of the first modification during the pandemic, this work
does not include more recent Italian studies.
Our work thus
suggests that a public health crisis has resulted from the pandemic, a
concern raised in other countries too, such as France and Denmark;
indeed, a danish study demonstrated that mortality rates for patients
admitted to hospitals with non-covid-19 diseases (such as respiratory
disease, cancer, pneumonia and sepsis) were higher.[210,211] More
detailed, nationwide population-based cohort studies are needed to
assess whether emergency management benefited from the reorganisation
adopted and evaluate hospital admissions and mortality rates for
non-covid patients. Nevertheless, the system and telemedicine
undoubtedly played – and continue to play – a crucial role in dealing
with non-deferrable and deferrable conditions, respectively.
Contributions
T.P.
and G.L. conceived and designed the study. T.P. collected the data.
G.L, M.M.O, An.B, G.A., Al.B. analysed and selected the data. F.C. and
T.P. supervised data analysis. G.L, M.M.O., An.B, G.A., Al.B., T.P.,
wrote the manuscript. M.M.O. and An.B. revised and edited the
manuscript. L.Z. and P.R. revised the final version of the manuscript.
Funding
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf
and declare: the work was supported by the Center for Excellence and
Transdisciplinary Studies (CEST) and C.R.T. Foundation, Turin. The
funder of the study had no role in the study design, data collection,
data analysis, data interpretation, or writing the report; no financial
relationships with any organisations that might have an interest in the
submitted work; no other relationships or activities that could appear
to have influenced the submitted work. All authors had full access to
all study data and had final responsibility for the decision to submit
for publication. The authors are thankful to Professor Paolo Vineis for
his critical assistance in writing the paper.
References
- WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed June 20, 2020).
- Livingston E, Bucher K. Coronavirus Disease 2019 (COVID-19) in Italy. JAMA 2020; 323: 1335.
- Portnoy J, Waller M, Elliott T. Telemedicine in the Era of COVID-19. J allergy Clin Immunol Pract 2020; 8: 1489–91.
- Acheson RM. The definition and identification of need for health care. J Epidemiol Community Health 1978; 32: 10–5.
- Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet 2020; 395: 1225–8.
- Moher
D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred Reporting
Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement.
PLOS Med 2009; 6: e1000097.
- *** ATTO COMPLETO ***. https://www.gazzettaufficiale.it/atto/vediMenuHTML?atto.dataPubblicazioneGazzetta=2020-03-09&atto.codiceRedazionale=20A01558&tipoSerie=serie_generale&tipoVigenza=originario (accessed June 20, 2020).
- Magnani
C, Azzolina D, Gallo E, Ferrante D, Gregori D. How Large Was the
Mortality Increase Directly and Indirectly Caused by the COVID-19
Epidemic? An Analysis on All-Causes Mortality Data in Italy. Int J
Environ Res Public Health 2020; 17. HTTP://DX.DOI.ORG/10.3390/ijerph17103452
- Baldi
E, Sechi GM, Mare C, et al. Out-of-Hospital Cardiac Arrest during the
Covid-19 Outbreak in Italy. N Engl J Med 2020; published online April. HTTP://DX.DOI.ORG/10.1056/NEJMc2010418
- De
Filippo O, D’Ascenzo F, Angelini F, et al. Reduced Rate of Hospital
Admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J
Med 2020; NEJMc2009166.
- Baracchini C,
Pieroni A, Viaro F, et al. Acute stroke management pathway during
Coronavirus-19 pandemic. Neurol Sci 2020; 41: 1003–5.
- Comelli
I, Scioscioli F, Cervellin G. Impact of the COVID-19 epidemic on
census, organization and activity of a large urban Emergency
Department. Acta Biomed 2020; 91: 45–9.
- Senni M. COVID-19 experience in Bergamo, Italy. Eur Heart J 2020; 41: 1783–4.
- Cosentino
N, Assanelli E, Merlino L, Mazza M, Bartorelli AL, Marenzi G. An
In-hospital Pathway for Acute Coronary Syndrome Patients During the
COVID-19 Outbreak: Initial Experience Under Real-World Suboptimal
Conditions. Can J Cardiol 2020; 36: 961–4.
- Stefanini
GG, Azzolini E, Condorelli G. Critical Organizational Issues for
Cardiologists in the COVID-19 Outbreak: A Frontline Experience from
Milan, Italy. Circulation 2020; 1597–9.
- Agostoni
P, Mapelli M, Conte E, et al. Cardiac patient care during a pandemic:
how to reorganise a heart failure unit at the time of COVID-19.
Eur J Prev Cardiol 2020; 2047487320925632.
- Piepoli
MF, Emdin M. A dialogue between the editor-in-chief and a deputy editor
of a cardiology journal during the coronavirus outbreak: Take-home
messages from the Italian experience. Eur J Prev Cardiol 2020; 27:
790–2.
- Mazzone P, Peretto G, Radinovic A, et
al. The COVID-19 challenge to cardiac electrophysiologists: optimizing
resources at a referral center. J Interv Card
Electrophysiol an Int J Arrhythm pacing 2020; : 1–7.
- Secco
GG, Zocchi C, Parisi R, et al. Decrease and Delay in Hospitalization
for Acute Coronary Syndromes During the 2020 SARS-CoV-2 Pandemic.
Can J Cardiol 2020; published online May. HTTP://DX.DOI.ORG/10.1016/j.cjca.2020.05.023
- Franco
F, Alessandro Z, Carlo C, et al. Impact of COVID-19 epidemic on
coronary care unit accesses for acute coronary syndrome in Veneto
region, Italy. Am Heart J 2020; 226: 26–8.
- Mauro
T, Francesco N, Marco A, Marco M, Domenico F. Unpredictable Fall of
Severe Emergent Cardiovascular Diseases Hospital Admissions During the
COVID‐19 Pandemic: Experience of a Single Large Center in Northern
Italy. J Am Heart Assoc 2020; 0: e017122.
- Cenzato
M, DiMeco F, Fontanella M, Locatelli D, Servadei F. Editorial.
Neurosurgery in the storm of COVID-19: suggestions from the Lombardy
region, Italy (ex malo bonum). J. Neurosurg. 2020; 1–2.
- Federico
M, Alessandro Z, Dario G, et al. Urgent Pacemaker Implantation Rates in
the Veneto Region of Italy After the COVID-19 Outbreak. Circ Arrhythmia
Electrophysiol 2020; 13: e008722.
- Migliore F,
Zorzi A, Gregori D, et al. Urgent Pacemaker Implantation Rates in the
Veneto Region of Italy After the COVID-19 Outbreak. Circ.
Arrhythm. Electrophysiol. 2020; 13: e008722.
- De
Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations
for myocardial infarction in Italy in the COVID-19 era. Eur Heart J
2020; 41. HTTP://DX.DOI.ORG/10.1093/eurheartj/ehaa409
- Colivicchi
F, Di Fusco SA, Magnanti M, Cipriani M, Imperoli G. The Impact of the
Coronavirus Disease-2019 Pandemic and Italian Lockdown Measures
on Clinical Presentation and Management of Acute Heart Failure.
J. Card. Fail. 2020; published online May. HTTP://DX.DOI.ORG/10.1016/j.cardfail.2020.05.007
- Naccarato
M, Scali I, Olivo S, et al. Has COVID-19 played an unexpected “stroke”
on the chain of survival? J Neurol Sci 2020; 414: 116889.
- Nguyen
TN, Abdalkader M, Jovin TG, et al. Mechanical Thrombectomy in the Era
of the COVID-19 Pandemic: Emergency Preparedness for Neuroscience
Teams: A Guidance Statement from the Society of Vascular and
Interventional Neurology. Stroke 2020; 1896–901.
- Bersano
A, Kraemer M, Touzé E, et al. Stroke care during the Covid-19 pandemic:
Experience from three large European countries. Eur J Neurol 2020; n/a.
HTTP://DX.DOI.ORG/10.1111/ene.14375
- Cofano
F, Tartara F, Zenga F, Penner F, Lanotte M, Garbossa D. Letter: Back
Pain and Accesses to Emergency Departments During COVID-19 Lockdown
in Italy. Neurosurgery 2020; published online May. HTTP://DX.DOI.ORG/10.1093/neuros/nyaa174
- Markus HS, Brainin M. COVID-19 and stroke—A global World Stroke Organization perspective. Int J Stroke 2020; 15: 361–4.
- Patriti
A, Eugeni E, Guerra F. What happened to surgical emergencies in the era
of COVID-19 outbreak? Considerations of surgeons working in an
Italian COVID-19 red zone. Updates Surg. 2020; 1–2.
- Lauro
A, Pagano N, Impellizzeri G, Cervellera M, Tonini V. Emergency
Endoscopy During the SARS-CoV-2 Pandemic in the North of Italy:
Experience from St. Orsola University Hospital-Bologna. Dig Dis
Sci 2020; 65: 1559–61.
- Zheng MH, Boni L,
Fingerhut A. Minimally Invasive Surgery and the Novel Coronavirus
Outbreak: Lessons Learned in China and Italy. Ann Surg 2020; 272:
e5–6.
- Leva E, Morandi A, Sartori A, Macchini
F, Berrettini A, Manzoni G. Correspondence from Northern Italy about
our experience with COVID-19. J Pediatr Surg 2020; 55: 985–6.
- Patriti
A, Baiocchi GL, Catena F, Marini P, Catarci M, FACS on behalf of the
Associazione Chirurghi Ospedalieri Italiani (ACOI). Emergency general
surgery in Italy during the COVID-19 outbreak: first survey from the
real life. World J Emerg Surg 2020; 15: 36.
- D’Ovidio
V, Lucidi C, Bruno G, Miglioresi L, Lisi D, Bazuro ME. A snapshot of
urgent upper gastrointestinal endoscopy care during the Covid-19
outbreak in Italy. J Gastroenterol Hepatol 2020; published online June.
HTTP://DX.DOI.ORG/10.1111/jgh.15132
- Motterle
G, Morlacco A, Iafrate M, et al. The impact of COVID-19 pandemic on
urological emergencies: a single-center experience. World J Urol
2020; : 1–5.
- Grandone E, Mastroianno M, Caroli
A, Ostuni A. Blood supply and transfusion support in southern Italy:
findings during the first four weeks of the SARS-CoV-2 pandemic.
Blood Transfus 2020; 18: 230–2.
- Mascaretti L,
De Angelis V, Berti P. The severe acute respiratory syndrome
coronavirus 2 (SARS-CoV-2) pandemic and Transfusion Medicine:
reflections from Italy. Blood Transfus. 2020; 18: 77–8.
- Franchini
M, Farrugia A, Velati C, et al. The impact of the SARS-CoV-2 outbreak
on the safety and availability of blood transfusions in Italy. Vox Sang
2020; published online April. HTTP://DX.DOI.ORG/10.1111/vox.12928
- Pata
D, Gatto A, Buonsenso D, Chiaretti A. A COVID-19 outbreak’s lesson:
Best use of the paediatric emergency department. Acta Paediatr; n/a. HTTP://DX.DOI.ORG/10.1111/apa.15386
- Cognigni
M. An Italian paediatric department at the time of Coronavirus: a
resident’s point of view. Arch. Dis. Child. 2020; published online
April. HTTP://DX.DOI.ORG/10.1136/archdischild-2020-319299
- Lazzerini
M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed
access or provision of care in Italy resulting from fear of COVID-19.
Lancet. Child Adolesc. Heal. 2020; 4: e10--e11.
- Giacalone
S, Bortoluzzi P, Nazzaro G. Which are the “emergent” dermatologic
practices during COVID-19 pandemic? Report from the lockdown in Milan,
Italy. Int J Dermatol; n/a. HTTP://DX.DOI.ORG/10.1111/ijd.15005
- Tartari
F, Guglielmo A, Fuligni F, Pileri A. Changes in emergency service
access after spread of COVID-19 across Italy. J. Eur. Acad. Dermatol.
Venereol. 2020; published online April. HTTP://DX.DOI.ORG/10.1111/jdv.16553
- Gagliano
A, Villani PG, Cò FM, et al. 2019-ncov’s epidemic in middle province of
northern Italy: Impact, logistic & strategy in the first line
hospital. Disaster Med Public Health Prep 2020; 1–5.
- Ferrazzi
EM, Frigerio L, Cetin I, et al. COVID-19 Obstetrics Task Force,
Lombardy, Italy: Executive management summary and short report of
outcome. Int J Gynaecol Obstet Off organ Int Fed Gynaecol Obstet
2020; 149: 377–8.
- Baggiani A, Briani S,
Luchini G, et al. Management of healthcare areas for the prevention of
COVID-19 emergency in an Italian teaching hospital (Pisa,
Tuscany): A hospital renovation plan. Infect Control Hosp Epidemiol
2020; 1–6.
- Carenzo L, Costantini E, Greco M,
et al. Hospital surge capacity in a tertiary emergency referral centre
during the COVID-19 outbreak in Italy. Anaesthesia 2020; 75:
928–34.
- Meschi T, Rossi S, Volpi A, et al.
Reorganization of a large academic hospital to face COVID-19 outbreak:
The model of Parma, Emilia-Romagna region, Italy. Eur. J. Clin.
Invest. 2020; 50: e13250.
- Mariani NM, Pisani
Ceretti A, Fedele V, et al. Surgical Strategy During the COVID-19
Pandemic in a University Metropolitan Hospital in Milan, Italy.
World J Surg 2020; 1–6.
- Ghio S, Ferlini M,
Scelsi L, et al. La pandemia COVID-19: Riorganizzazione della
Cardiologia in un ospedale della Regione Lombardia. G Ital Cardiol
2020; 21: 358–9.
- Villa E, Saccocci M, Messina
A, et al. COVID-19 e coronaropatia: Uso selettivo e collaborativo delle
risorse durante le crisi sanitarie. G Ital Cardiol 2020; 21: 360–3.
- Chisci
E, Masciello F, Michelagnoli S. The Italian USL Toscana Centro model of
a vascular hub responding to the COVID-19 emergency. J Vasc Surg 2020;
72: 8–11.
- Zangrillo A, Beretta L, Silvani P,
et al. Fast reshaping of intensive care unit facilities in a large
metropolitan hospital in Milan, Italy: facing the COVID-19 pandemic
emergency. Crit Care Resusc 2020; published online April.
- Elrod
JK, Fortenberry JLJ. The hub-and-spoke organization design revisited: a
lifeline for rural hospitals. BMC Health Serv Res 2017; 17: 795.
- Zoia
C, Bongetta D, Veiceschi P, et al. Neurosurgery during the COVID-19
pandemic: update from Lombardy, northern Italy. Acta Neurochir (Wien)
2020; 162: 1221–2.
- Fontanella MM, Maria L De,
Zanin L, et al. Neurosurgical Practice During the Severe Acute
Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Pandemic: A Worldwide
Survey. World Neurosurg 2020; 2: 1–9.
- Fontanella
MM, Saraceno G, Lei T, et al. Neurosurgical activity during COVID-19
pandemic: an expert opinion from China, South Korea, Italy, United
Stated of America, Colombia and United Kingdom. J Neurosurg Sci 2020. HTTP://DX.DOI.ORG/10.23736/S0390-5616.20.04994-2
- Bernucci
C, Brembilla C, Veiceschi P. Effects of the COVID-19 Outbreak in
Northern Italy: Perspectives from the Bergamo Neurosurgery Department.
World Neurosurg 2020; 137: 465--468.e1.
- Dobran
M, Paracino R, Iacoangeli M. Letter to the editor by Dobran Mauro,
Paracino Riccardo, and Iacoangeli Maurizio regarding ‘Neurosurgery
during the COVID-19 pandemic: update from Lombardy, northern Italy.’
Zoia C, Bongetta D, Veiceschi P, Cenzato M, Di Meco F, Locatelli D,
Boeris D, Fo. Acta Neurochir. (Wien). 2020; 162: 1223–4.
- Giorgi
PD, Villa F, Gallazzi E, et al. The management of emergency spinal
surgery during the COVID-19 pandemic in Italy. Bone Joint J 2020;
102-B: 671–6.
- Levi V, Risso A, Egidi M.
Letter : The Resiliency of the Neurosurgeon in the Midst of COVID-19
Pandemic Storm : The Italian Experience From the Frontline. 2020; 0:
2019–20.
- Castelnuovo P, Turri-Zanoni M,
Karligkiotis A, et al. Skull-base surgery during the COVID-19 pandemic:
the Italian Skull Base Society recommendations. Int Forum Allergy
Rhinol 2020; published online April. HTTP://DX.DOI.ORG/10.1002/alr.22596
- Mazzatenta
D, Zoli M, Cavallo MA, et al. Remodulation of neurosurgical activities
in an Italian region (Emilia-Romagna) under COVID- 19 emergency:
maintaining the standard of care during the crisis. J Neurosurg Sci
2020. HTTP://DX.DOI.ORG/10.23736/s0390-5616.20.05018-3
- Franzin
A, Spatola G, Giudice L, Migliorati K, Vivaldi O, Giorgi C. Maintaining
stereotactic radiosurgical treatments during Covid-19 outbreak: the
case of the Gamma Knife Unit in Brescia - Italy. Br. J. Neurosurg.
2020; 1–2.
- Mangialardi ML, Orrico M,
Mangialardi N. Routine in an Italian High-Volume Vascular Surgery Unit
during the COVID-19 Era: How the Pandemic Changed the Vascular
Daily Practice. Ann. Vasc. Surg. 2020; 66: 6–7.
- Bonalumi
G, di Mauro M, Garatti A, et al. The COVID-19 outbreak and its impact
on hospitals in Italy: the model of cardiac surgery. Eur J Cardiothorac
Surg 2020; 57: 1025–8.
- Bonalumi G, Di Mauro M,
Garatti A, Barili F, Parolari A, Gerosa G. [COVID-19 outbreak and
Cardiac Surgery: position paper from the COVID-SICCH Task Force
of the Italian Society for Cardiac Surgery]. G Ital Cardiol (Rome)
2020; 21: 396–400.
- Kurihara H, Bisagni P,
Faccincani R, Zago M. COVID-19 outbreak in Northern Italy: Viewpoint of
the Milan area surgical community. J Trauma Acute Care Surg 2020; 88:
719–24.
- Duci M, Antoniello LM, Trovalusci E,
Tognon C, Gamba P. Pediatric endoscopic procedures during the COVID-19
pandemic: an Italian center experience. Pediatr Surg Int 2020; 36:
853–4.
- Torzilli G, Vigano L, Galvanin J, et
al. A Snapshot of Elective Oncological Surgery in Italy During COVID-19
Emergency: Pearls, Pitfalls, and Perspectives. Ann Surg 2020;
published online May. HTTP://DX.DOI.ORG/10.1097/SLA.0000000000004081
- Navarra
G, Komaei I, Currò G, et al. Bariatric surgery and the COVID-19
pandemic: SICOB recommendations on how to perform surgery during
the outbreak and when to resume the activities in phase 2 of lockdown.
Updates Surg 2020; : 1–10.
- Repici A, Maselli
R, Colombo M, et al. Coronavirus (COVID-19) outbreak: what the
department of endoscopy should know. Gastrointest Endosc 2020; 1–6.
- Capanna
F, Haydar A, McCarey C, et al. Preparing an obstetric unit in the heart
of the epidemic strike of COVID-19: quick reorganization tips. J
Matern neonatal Med Off J Eur Assoc Perinat Med Fed Asia
Ocean Perinat Soc Int Soc Perinat Obstet 2020; 1–7.
- Giannubilo
SR, Giannella L, Delli Carpini G, Carnielli VP, Ciavattini A. Obstetric
network reorganization during the COVID-19 pandemic: Suggestions from
an Italian regional model. Eur. J. Obstet. Gynecol. Reprod. Biol.
2020; 249: 103–5.
- Di Saverio S, Pata F, Gallo
G, et al. Coronavirus pandemic and colorectal surgery: practical advice
based on the Italian experience. Colorectal Dis 2020; 22: 625–34.
- Di
Saverio S, Khan M, Pata F, et al. Laparoscopy at all costs? Not now
during COVID-19 outbreak and not for acute care surgery and emergency
colorectal surgery: A practical algorithm from a hub tertiary teaching
hospital in Northern Lombardy, Italy. J Trauma Acute Care Surg 2020;
88: 715–8.
- Vicini E, Galimberti V, Naninato P,
Vento AR, Ribeiro Fontana SK, Veronesi P. COVID-19: The European
institute of oncology as a ‘hub’ centre for breast cancer surgery
during the pandemic in Milan (Lombardy region, northern Italy) - A
screenshot of the first month. Eur. J. Surg. Oncol. J. Eur.
Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2020; 46: 1180–1.
- Gallo
G, La Torre M, Pietroletti R, et al. Italian society of colorectal
surgery recommendations for good clinical practice in colorectal
surgery during the novel coronavirus pandemic. Tech Coloproctol 2020;
24: 501–5.
- Ingenito C, Buonerba L, Ferrara C,
et al. Coronavirus Disease 2019 Emergency and Cancer in the South of
Italy: What’s New for the Oncologist? Front Med 2020; 7: 189.
- Fratino
L, Procopio G, Di Maio M, Cinieri S, Leo S, Beretta G. Coronavirus:
Older Persons With Cancer in Italy in the COVID-19 Pandemic. Front
Oncol 2020; 10: 648.
- Marano L, Marrelli D,
Roviello F. Cancer care under the outbreak of COVID-19: A perspective
from Italian tertiary referral center for surgical oncology. Eur.
J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg.
Oncol. 2020; 46: 1184–5.
- Lombardi CP, D’Amore
A, Grani G, et al. Endocrine surgery during COVID-19 pandemic: do we
need an update of indications in Italy? Endocrine 2020; 68: 485–8.
- Lambertini
M, Toss A, Passaro A, et al. Cancer care during the spread of
coronavirus disease 2019 (COVID-19) in Italy: Young oncologists’
perspective. ESMO Open 2020; 5. HTTP://DX.DOI.ORG/10.1136/esmoopen-2020-000759
- Quaglino
P, Fava P, Brizio M, et al. Metastatic melanoma treatment with
checkpoint inhibitors in the COVID-19 era: experience from an
Italian Skin Cancer Unit. J Eur Acad Dermatol Venereol 2020; published
online May. HTTP://DX.DOI.ORG/10.1111/jdv.16586
- Pietrantonio F, Garassino MC. Caring for Patients With Cancer During the COVID-19 Outbreak in Italy. JAMA Oncol 2020; 6: 821–2.
- Mandato VD, Aguzzoli L. Management of ovarian cancer during the COVID-19 pandemic. Int J Gynecol Obstet 2020; 149: 382–3.
- Perrone
A, Palma A, De Iaco P. COVID-19 global pandemic: options for management
of gynecologic cancers. The experience in surgical management of
ovarian cancer in the second highest affected Italian region. Int J
Gynecol Cancer 2020; 30: ijgc-2020.
- Allocca M,
Fiorino G, Furfaro F, et al. Maintaining the Quality Standards of Care
for Inflammatory Bowel Disease Patients During the COVID-19
Pandemic. Clin Gastroenterol Hepatol Off Clin Pract J Am
Gastroenterol Assoc 2020; 18: 1882–3.
- Occhipinti
V, Pastorelli L. Challenges in the Care of IBD Patients During the
CoViD-19 Pandemic: Report From a “Red Zone” Area in Northern Italy.
Inflamm Bowel Dis 2020; 26: 793–6.
- Maida M,
Sferrazza S, Savarino E, et al. ‘Impact of the COVID-19 pandemic on
Gastroenterology Divisions in Italy: a national survey’. Dig
liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study
Liver 2020; published online May. HTTP://DX.DOI.ORG/10.1016/j.dld.2020.05.017
- Rossi
D. Metronomic oral vinorelbine and lung cancer therapy during the COVID
19 pandemic: A single-center experience. Lung Cancer 2020; 145:
83–4.
- de Marinis F, Attili I, Morganti S, et
al. Results of Multilevel Containment Measures to Better Protect Lung
Cancer Patients From COVID-19: The IEO Model. Front Oncol 2020;
10: 665.
- Porzio G, Cortellini A, Bruera E, et
al. Home Care for Cancer Patients During COVID-19 Pandemic: The Double
Triage Protocol. J Pain Symptom Manage 2020; 60: e5-7.
- De
Vincentiis L, Carr RA, Mariani MP, Ferrara G. Cancer diagnostic rates
during the 2020 ‘lockdown’, due to COVID-19 pandemic, compared
with the 2018-2019: an audit study from cellular pathology. J Clin
Pathol 2020; published online June. HTTP://DX.DOI.ORG/10.1136/jclinpath-2020-206833
- Cuneo
A, Scarfo L, Reda G, et al. CHRONIC LYMPHOCYTIC LEUKEMIA MANAGEMENT IN
ITALY DURING THE COVID-19 PANDEMIC. A CAMPUS CLL REPORT. Blood 2020;
published online June 19. HTTP://DX.DOI.ORG/10.1182/blood.2020006854
- Ferrari
A, Zecca M, Rizzari C, et al. Children with cancer in the time of
COVID-19: An 8-week report from the six pediatric onco-hematology
centers in Lombardia, Italy. Pediatr. Blood Cancer. 2020; e28410.
- Bongiovanni
A, Mercatali L, Fausti V, Ibrahim T. Comment on ‘Reorganisation of
medical oncology departments during the novel coronavirus
disease-19 pandemic: A nationwide Italian survey’ by Alice Indini et
al. Eur. J. Cancer. 2020; 134: 3–5.
- Brandes
AA, Ardizzoni A, Artioli F, et al. Fighting cancer in coronavirus
disease era: organization of work in medical oncology departments
in Emilia Romagna region of Italy. Future Oncol 2020; published online
May. HTTP://DX.DOI.ORG/10.2217/fon-2020-0358
- Tagliamento
M, Spagnolo F, Poggio F, et al. Italian survey on managing immune
checkpoint inhibitors in oncology during COVID-19 outbreak. Eur J Clin
Invest 2020; n/a: e13315.
- Mistretta FA,
Luzzago S, Molendini LO, et al. A Guide for Oncologic Patient
Management during Covid-19 Pandemic: The Initial Experience of an
Italian Oncologic Hub with Exemplificative Focus on Uro-Oncologic
Patients. Cancers (Basel) 2020; 12. HTTP://DX.DOI.ORG/10.3390/cancers12061513
- Omarini
C, Maur M, Luppi G, et al. Cancer treatment during the coronavirus
disease 2019 pandemic: Do not postpone, do it! Eur J Cancer 2020;
133: 29–32.
- Pietrantonio F, Morano F, Niger
M, et al. Systemic Treatment of Patients With Gastrointestinal Cancers
During the COVID-19 Outbreak: COVID-19-adapted Recommendations of the
National Cancer Institute of Milan. Clin Colorectal Cancer 2020. HTTP://DX.DOI.ORG/10.1016/j.clcc.2020.05.004
- Pellino
G, Spinelli A. How coronavirus disease 2019 outbreak is impacting
colorectal cancer patients in Italy: A long shadow beyond infection.
Dis Colon Rectum 2020; 63: 720–2.
- Marandino
L, Di Maio M, Procopio G, Cinieri S, Beretta GD, Necchi A. The Shifting
Landscape of Genitourinary Oncology During the COVID-19 Pandemic
and how Italian Oncologists Reacted: Results from a National
Survey. Eur. Urol. 2020; published online April. HTTP://DX.DOI.ORG/10.1016/j.eururo.2020.04.004
- Indini
A, Aschele C, Cavanna L, et al. Reorganisation of medical oncology
departments during the novel coronavirus disease-19 pandemic: a
nationwide Italian survey. Eur J Cancer 2020; 132: 17–23.
- Silvestris
N, Moschetta A, Paradiso A, Delvino A. COVID-19 Pandemic and the Crisis
of Health Systems: The Experience of the Apulia Cancer Network
and of the Comprehensive Cancer Center Istituto Tumori ‘Giovanni Paolo
II’ of Bari. Int J Environ Res Public Health 2020; 17. HTTP://DX.DOI.ORG/10.3390/ijerph17082763
- Arduino
PG, Conrotto D, Broccoletti R. The outbreak of Novel Coronavirus
disease (COVID-19) caused a worrying delay in the diagnosis of
oral cancer in north-west Italy: The Turin Metropolitan Area
experience. Oral Dis. 2020; published online April. HTTP://DX.DOI.ORG/10.1111/odi.13362
- Minucci
A, Scambia G, Santonocito C, Concolino P, Urbani A. BRCA testing in a
genomic diagnostics referral center during the COVID-19 pandemic. Mol
Biol Rep 2020; 1–4.
- Vanni G, Pellicciaro
M, Materazzo M, Palombi L, Buonomo OC. Breast Cancer Diagnosis in
Coronavirus-Era: Alert From Italy. Front Oncol 2020; 10: 938.
- Mercadante S, Adile C, Ferrera P, Giuliana F. Palliative Care in the Time of COVID-19. J Pain Symptom Manage 2020; : 4–5.
- Etkind
SN, Bone AE, Lovell N, et al. The Role and Response of Palliative Care
and Hospice Services in Epidemics and Pandemics: A Rapid Review
to Inform Practice During the COVID-19 Pandemic. J Pain Symptom Manage
2020; 60: e31-40.
- Costantini M, Sleeman KE,
Peruselli C, Higginson IJ. Response and role of palliative care during
the COVID-19 pandemic: A national telephone survey of hospices in
Italy. Palliat Med 2020; 269216320920780.
- Lazzarin
P, Avagnina I, Divisic A, Agosto C, Giacomelli L, Benini F. Management
strategies adopted by a pediatric palliative care network in northern
Italy during the COVID-19 pandemic. Acta Paediatr 2020; n/a. HTTP://DX.DOI.ORG/10.1111/apa.15411
- Zagra
L, Faraldi M, Pregliasco F, et al. Changes of clinical activities in an
orthopaedic institute in North Italy during the spread of COVID-19
pandemic: a seven-week observational analysis. Int Orthop 2020. HTTP://DX.DOI.ORG/10.1007/s00264-020-04590-1
- Randelli
PS, Compagnoni R. Management of orthopaedic and traumatology patients
during the Coronavirus disease (COVID-19) pandemic in northern Italy.
Knee Surg Sports Traumatol Arthrosc 2020; 28: 1683–9.
- Casiraghi
A, Domenicucci M, Cattaneo S, et al. Operational strategies of a trauma
hub in early coronavirus disease 2019 pandemic. Int Orthop 2020. HTTP://DX.DOI.ORG/10.1007/s00264-020-04635-5.
- Placella
G, Salvato D, Delmastro E, Bettinelli G, Salini V. CoViD-19 and ortho
and trauma surgery: The Italian experience. Injury 2020; 51: 1403–5.
- Di Martino A, Faldini C. Trauma service reorganization in Bologna (Italy) during COVID-19 pandemic. Injury. 2020; 51: 1684.
- Maniscalco
P, Poggiali E, Quattrini F, et al. The deep impact of novel CoVID-19
infection in an Orthopedics and Traumatology Department: the experience
of the Piacenza Hospital. Acta Biomed 2020; 91: 97–105.
- Bettinelli
G, Delmastro E, Salvato D, Salini V, Placella G. Orthopaedic patient
work fl ow in CoViD-19 pandemic in Italy. J Orthop 2020; 22: 158–9.
- Grassi
A, Pizza N, Tedesco D, Zaffagnini S. The COVID-19 outbreak in Italy:
perspectives from an orthopaedic hospital. Int Orthop 2020; 1–5.
- Maniscalco
P, Poggiali E, Quattrini F, et al. Proximal femur fractures in COVID-19
emergency: the experience of two Orthopedics and Traumatology
Departments in the first eight weeks of the Italian epidemic. Acta
Biomed 2020; 91: 89–96.
- D’Apolito R, Faraldi
M, Ottaiano I, Zagra L. Disruption of Arthroplasty Practice in an
Orthopedic Center in Northern Italy During the Coronavirus
Disease 2019 Pandemic. J Arthroplasty 2020; 35: S6-9.
- Facchin
F, Messana F, Sonda R, Faccio D, Tiengo C, Bassetto F. COVID-19:
Initial experience of hand surgeons in Northern Italy. Hand Surg.
Rehabil. 2020; published online May. HTTP://DX.DOI.ORG/10.1016/j.hansur.2020.04.007
- Scalise
A, Torresetti M, Di Benedetto G. Wound Healing Center: Analysis of
preventive measures and new indications in a teaching hospital in
central Italy during the Covid-19 emergency. Int Wound J; n/a. HTTP://DX.DOI.ORG/10.1111/iwj.13430
- Pignatti
M, Pinto V, Miralles MEL, Giorgini FA, Cannamela G, Cipriani R. How the
COVID-19 pandemic changed the Plastic Surgery activity in a regional
referral center in Northern Italy. J Plast Reconstr Aesthetic Surg
2020; : 1–9.
- Ranno R, Vestita M, Verrienti P,
et al. The role of enzymatic debridement in burn care in the COVID-19
pandemic . Commentary by the Italian Society of Burn Surgery ( SIUST ).
Burns 2020; : 2019–20.
- Ficarra V, Novara G,
Abrate A, et al. Urology practice during COVID-19 pandemic. Minerva
Urol Nefrol 2020; published online March. HTTP://DX.DOI.ORG/10.23736/S0393-2249.20.03846-1
- Novara
G, Bartoletti R, Crestani A, et al. Impact of the COVID-19 pandemic on
urological practice in emergency departments in Italy. BJU Int
2020; published online May. HTTP://DX.DOI.ORG/10.1111/bju.15107
- Simonato
A, Giannarini G, Abrate A, et al. Pathways for urology patients during
the COVID-19 pandemic. Minerva Urol Nefrol 2020; published online
March. HTTP://DX.DOI.ORG/10.23736/S0393-2249.20.03861-8
- Luciani
LG, Mattevi D, Giusti G, et al. Guess Who’s Coming to Dinner: COVID-19
in a COVID-free Unit. Urology 2020; published online May. HTTP://DX.DOI.ORG/10.1016/j.urology.2020.05.011
- Cini C, Bortot G, Sforza S, et al. Paediatric urology practice during COVID-19 pandemic. J Pediatr Urol 2020; 16: 295–6.
- Rocco
B, Sighinolfi MC, Sandri M, et al. The dramatic COVID-19 outbreak in
italy is responsible of a huge drop in urological surgical activity: A
multicenter observational study. BJU Int 2020; n/a. HTTP://DX.DOI.ORG/10.1111/bju.15149
- Campi RR, Amparore D. Letter to the Editor. Eur Urol 2020; 9–10.
- Allevi
F, Dionisio A, Baciliero U, et al. Impact of COVID-19 epidemic on
maxillofacial surgery in Italy. Br J Oral Maxillofac Surg 2020;
published online May. HTTP://DX.DOI.ORG/10.1016/j.bjoms.2020.04.035
- De
Bernardi F, Turri-Zanoni M, Battaglia P, Castelnuovo P. How to
Reorganize an Ear, Nose, and Throat Outpatient Service During the
COVID-19 Outbreak: Report From Northern Italy. Laryngoscope 2020;
published online May. HTTP://DX.DOI.ORG/10.1002/lary.28716
- Ralli
M, Minni A, Candelori F, Cialente F, Greco A, de Vincentiis M. Effects
of COVID-19 Pandemic on Otolaryngology Surgery in Italy: The Experience
of Our University Hospital. Otolaryngol Neck Surg
2020; 0194599820928970.
- Veritti D, Sarao
V, Bandello F, Lanzetta P. Infection control measures in ophthalmology
during the COVID-19 outbreak: A narrative review from an early
experience in Italy. Eur J Ophthalmol 2020. HTTP://DX.DOI.ORG/10.1177/1120672120927865
- Arrigo
A, Aragona E, Parodi MB, Loperfido F, Bandello F. Ophthalmology and
SARS-CoV-2: Blind toward those who fight blindness? Eur J Ophthalmol
2020; 1120672120929961.
- Tognetto D,
Pastore MR, De Giacinto C, et al. Managing ophthalmic practices in a
referral emergency COVID-19 hospital in north-east Italy. Acta
Ophthalmol 2020; n/a. HTTP://DX.DOI.ORG/10.1111/aos.14488
- Lanni
V, Iuliano A, Laezza MP, Uccello G, Tranfa F, Strianese D. Oculoplastic
management of patients in the Covid-19 era: experience from an Italian
tertiary referral center. Orbit 2020; 1–3.
- Parravano
M, Borrelli E, Costanzo E, Sacconi R, Varano M, Querques G. Protect
Healthcare Workers and Patients from COVID-19: The Experience of
Two Tertiary Ophthalmology Care Referral Centers in Italy.
Ophthalmol Ther 2020; 9: 231–4.
- Barca I,
Cordaro R, Kallaverja E, Ferragina F, Cristofaro MG. Management in oral
and maxillofacial surgery during the COVID-19 pandemic: Our experience.
Br J Oral Maxillofac Surg 2020; S0266--4356(20)30177--7.
- Galli
J, Settimi S, Tricarico L, Almadori G, Paludetti G. Clinical and
surgical management of patients with head and neck cancer in a
COVID-19 dedicated center in Italy. Head Neck 2020; published
online June. HTTP://DX.DOI.ORG/10.1002/hed.26263
- Saibene
AM, Allevi F, Biglioli F, Felisati G. Role and Management of a Head and
Neck Department during the COVID-19 Outbreak in Lombardy. Otolaryngol
Neck Surg 2020; 162: 795–6.
- Riva G, Pizzo C,
Fassone E, Pecorari G. Head and neck cancer surgery in COVID-19
pandemic in Northern Italy. Oral Oncol 2020; 104835.
- Pezzulla
D, Macchia G, Taccari F, Sticca G, Deodato F. Radiotherapy in Southern
Italy at the time of COVID-19: options for radiation oncology
units. Int. J. Gynecol. cancer Off. J. Int. Gynecol. Cancer
Soc. 2020; published online May. HTTP://DX.DOI.ORG/10.1136/ijgc-2020-001523
- Montesi
G, Di Biase S, Chierchini S, et al. Radiotherapy during COVID-19
pandemic. How to create a No fly zone: a Northern Italy
experience. Radiol Med 2020; 125: 600–3.
- Jereczek-fossa
BA, Pepa M, Marvaso G, et al. COVID-19 outbreak and cancer radiotherapy
disruption in Italy: Survey endorsed by the Italian Association of
Radiotherapy and Clinical Oncology (AIRO). 2020.
- Jereczek-Fossa
BA, Palazzi MF, Soatti CP, et al. COVID-19 Outbreak and Cancer
Radiotherapy Disruption in Lombardy, Northern Italy. Clin. Oncol. (R.
Coll. Radiol). 2020; 32: e160–1.
- Filippi AR,
Russi E, Magrini SM, Corvò R. Letter from Italy: First practical
indications for radiation therapy departments during COVID-19 outbreak.
Int J Radiat Oncol Biol Phys 2020. HTTP://DX.DOI.ORG/10.1016/j.ijrobp.2020.03.007
- Meattini
I, Franco P, Belgioia L, et al. Radiation therapy during the
coronavirus disease 2019 (covid-19) pandemic in Italy: A view of the
nation’s young oncologists. ESMO Open 2020; 5: 2019–21.
- Alterio
D, Volpe S, Marvaso G, et al. Head and neck cancer radiotherapy amid
COVID-19 pandemic: Report from Milan, Italy. Head Neck; n/a. HTTP://DX.DOI.ORG/10.1002/hed.26319.
- Rinaldi
CG, Ippolito E, Greco C, Matteucci P, D’Angelillo RM, Ramella S.
Radiotherapy for pain relief from bone metastases during Coronavirus
(COVID-19) pandemic. Eur J Pain (United Kingdom) 2020; 1211–2.
- Barra
S, Guarnieri A, di Monale E Bastia MB, et al. Short fractionation
radiotherapy for early prostate cancer in the time of COVID-19:
long-term excellent outcomes from a multicenter Italian trial suggest a
larger adoption in clinical practice. Radiol Med 2020; : 1–5.
- Krengli
M, Ferrara E, Mastroleo F, Brambilla M, Ricardi U. Running a Radiation
Oncology Department at the time of coronavirus: an Italian
experience. Adv Radiat Oncol 2020; published online March. HTTP://DX.DOI.ORG/10.1016/j.adro.2020.03.003
- Portaluri
M, Tramacere F, Portaluri T, Gianicolo EAL. Southern Italy: How the
supply of radiation therapy, patient outcomes, and risk to health
care providers have changed during the COVID-19 Pandemic. Adv Radiat
Oncol 2020; published online April. HTTP://DX.DOI.ORG/10.1016/j.adro.2020.03.016
- Valenti
M, Gargiulo L, Pavia G, et al. Reorganization of a Northern Italy
dermatology department during the COVID-19 pandemic: is it temporary or
the beginning of a new era in dermatology? J Dermatolog Treat 2020; 1–2.
- Pacifico
A, Ardigò M, Frascione P, Damiani G, Morrone A. Phototherapeutic
approach to dermatological patients during the 2019 Coronavirus
pandemic: Real-life Data from the Italian Red Zone. Br J Dermatol 2020;
n/a. HTTP://DX.DOI.ORG/10.1111/bjd.19145
- Patrizi
A, Bardazzi F, Filippi F, Abbenante D, Piraccini BM. The covid-19
outbreak in Italy: preventive and protective measures adopted by the
dermatology unit of bologna university hospital. Dermatol Ther
2020; 1–2.
- Marasca C, Ruggiero A,
Annunziata MC, Fabbrocini G, Megna M. Face the COVID-19 emergency:
measures applied in an Italian Dermatologic Clinic. J Eur Acad
Dermatology Venereol 2020; 0–3.
- Rossi E,
Trakatelli M, Giacomelli L, et al. The COVID-19 outbreak in
dermatologic surgery: resetting clinical priorities. J Eur Acad
Dermatol Venereol 2020; published online May. HTTP://DX.DOI.ORG/10.1111/jdv.16672
- Radi
G, Diotallevi F, Campanati A, Offidani A. Global coronavirus pandemic
(2019-nCOV): implication for an Italian medium size dermatological
clinic of a II level hospital. J Eur Acad Dermatology Venereol 2020;
34: e213–4.
- Micali G, Musumeci ML, Peris K.
The Italian dermatologic community facing COVID-19 pandemic :
recommendation from the Italian society of dermatology and venereology.
2020; 155: 123–5.
- Atzori L, Mugheddu C, Addis
G, et al. Psoriasis health care in the time of the coronavirus
pandemic: insights from dedicated centers in sardinia (Italy). J Eur
Acad Dermatology Venereol 2020. HTTP://DX.DOI.ORG/10.1111/jdv.16473
- Gisondi
P, Facheris P, Dapavo P, et al. The impact of the COVID-19 pandemic on
patients with chronic plaque psoriasis being treated with
biological therapy: the Northern Italy experience. Br J Dermatol 2020;
published online April. HTTP://DX.DOI.ORG/10.1111/bjd.19158
- COVID-19 and biologics for psoriasis: a high-epidemic area experience - Bergamo, 2 Lombardy, Italy. 2020.
- Posteraro
B, Marchetti S, Romano L, et al. Clinical microbiology laboratory
adaptation to COVID-19 emergency: experience at a large teaching
hospital in Rome, Italy. Clin Microbiol Infect 2020; 2019–21.
- Manganaro
M, Baldovino S, Besso L, et al. First considerations on the SARS-CoV-2
epidemic in the Dialysis Units of Piedmont and Aosta Valley, Northern
Italy. J Nephrol 2020; 33: 393–5.
- Brioni E,
Leopaldi D, Magnaghi C, et al. [Covid-19 in patients on dialysis:
infection prevention and control strategies]. G Ital di Nefrol
organo Uff della Soc Ital di Nefrol 2020; 37.
- Rombolà
G, Heidempergher M, Pedrini L, et al. Practical indications for the
prevention and management of SARS-CoV-2 in ambulatory dialysis
patients: lessons from the first phase of the epidemics in Lombardy. J.
Nephrol. 2020; 33: 193–6.
- Pascale MM, Bianco
G, Ferri L, Agnes S. COVID-19 health restrictions in a transplanted
Italian cohort. Transpl. Int. Off. J. Eur. Soc. Organ
Transplant. 2020; published online May. HTTP://DX.DOI.ORG/10.1111/tri.13661
- De
Simone P, Melandro F, Balzano E, et al. COVID 19 infection requires
strengthening of the chronic care model: the impact on liver transplant
practice at a high-volume center in Italy. Liver Transplant; n/a. HTTP://DX.DOI.ORG/10.1002/lt.25821
- Umberto
M, Luciano DC, Daniel Y, et al. The impact of the COVID-19 outbreak on
liver transplantation programs in Northern Italy. Am J Transplant 2020;
n/a. HTTP://DX.DOI.ORG/10.1111/ajt.15948.
- Angelico
R, Trapani S, Manzia TM, Lombardini L, Tisone G, Cardillo M. The
COVID-19 outbreak in Italy: Initial implications for organ
transplantation programs. Am J Transplant 2020; published online April.
HTTP://DX.DOI.ORG/10.1111/ajt.15904
- Agnes
S, Andorno E, Avolio AW, et al. Preliminary Analysis of the Impact of
COVID-19 Outbreak on Italian Liver Transplant Programs. Liver
Transplant. Off. Publ. Am. Assoc. Study Liver Dis. Int.
Liver Transplant. Soc. 2020; published online May. HTTP://DX.DOI.ORG/10.1002/lt.25790
- Vistoli F, Furian L, Maggiore U, et al. COVID-19 and kidney transplantation: an Italian Survey and Consensus. J Nephrol 2020. HTTP://DX.DOI.ORG/10.1007/s40620-020-00755-8
- Lauterio
A, De Carlis R, Belli L, Fumagalli R, De Carlis L. How to guarantee
liver transplantation in the north of Italy during the COVID-19
pandemic: A sound transplant protection strategy. Transpl. Int. 2020;
published online April. HTTP://DX.DOI.ORG/10.1111/tri.13633
- Cacciola
R. Response to ‘The COVID-19 outbreak in Italy: Initial implications
for organ transplantation programs’. Am. J. Transplant.
Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2020;
published online May. HTTP://DX.DOI.ORG/10.1111/ajt.15968
- Cesari M, Proietti M. Geriatric Medicine in Italy in the Time of COVID-19. J Nutr Heal Aging 2020; 24: 459–60.
- Berardi
G, Colasanti M, Levi Sandri GB, et al. Continuing our work: transplant
surgery and surgical oncology in a tertiary referral COVID-19 center.
Updates Surg 2020. HTTP://DX.DOI.ORG/10.1007/s13304-020-00825-3
- Mauro
V, Lorenzo M, Paolo C, Sergio H. Treat all COVID 19-positive patients,
but do not forget those negative with chronic diseases. Intern
Emerg Med 2020; 1–4.
- Iasevoli F, Fornaro
M, D’Urso G, et al. Psychological distress in patients with serious
mental illness during the COVID-19 outbreak and one-month mass
quarantine in Italy. Psychol Med 2020; 1–3.
- Costi S, Caporali R, Cimaz R. Dealing with COVID-19 in a Pediatric Rheumatology Unit in Italy. Pediatr Drugs 2020; 22: 263–4.
- Ohannessian
R, Duong TA, Odone A. Global Telemedicine Implementation and
Integration Within Health Systems to Fight the COVID-19 Pandemic: A
Call to Action. JMIR Public Heal Surveill 2020; 6: e18810.
- Brunasso
AMG, Massone C. Teledermatologic monitoring for chronic cutaneous
autoimmune diseases with smartworking during Covid-19 emergency
in a tertiary center in Italy. Dermatol Ther 2020; : e13495
- Luciani
LG, Mattevi D, Cai T, Giusti G, Proietti S, Malossini G. Teleurology in
the Time of Covid-19 Pandemic: Here to Stay? Urology 2020; 140: 4–6.
- Salzano
A, D’Assante R, Stagnaro FM, et al. Heart failure management during
COVID-19 outbreak in Italy. Telemedicine experience from a heart
failure university tertiary referral centre. Eur. J. Heart Fail. 2020;
published online May. HTTP://DX.DOI.ORG/10.1002/ejhf.1911
- Capozzo
R, Zoccolella S, Musio M, Barone R, Accogli M, Logroscino G.
Telemedicine is a useful tool to deliver care to patients with
Amyotrophic Lateral Sclerosis during COVID-19 pandemic: results from
Southern Italy. Amyotroph Lateral Scler Front Degener 2020; : 1–7.
- Hammad
TA, Parikh M, Tashtish N, et al. Impact of COVID-19 pandemic on
ST-elevation myocardial infarction in a non-COVID-19 epicenter.
Catheter Cardiovasc Interv 2020; published online June. HTTP://DX.DOI.ORG/10.1002/ccd.28997
- Bres
Bullrich M, Fridman S, Mandzia JL, et al. COVID-19: Stroke Admissions,
Emergency Department Visits, and Prevention Clinic Referrals. Can
J Neurol Sci Le J Can des Sci Neurol 2020; 1–10.
- Hajdu,
Steven D et al. “Acute Stroke Management During the COVID-19 Pandemic:
Does Confinement Impact Eligibility for Endovascular Therapy?.” Stroke
vol. 51,8 (2020): 2593-2596. http://dx.doi.org/10.1161/STROKEAHA.120.030794
- Di
Liberto, Ilenia Alessandra, et al. "Impact on hospital admission of
ST-elevation myocardial infarction patients during coronavirus disease
2019 pandemic in an Italian Hospital." Journal of Cardiovascular
Medicine 21.9 (2020): 722-724.
- Del Pinto,
Rita, et al. "Increased cardiovascular death rates in a COVID‐19 low
prevalence area." The Journal of Clinical Hypertension (2020).
- Chiesa,
Roberto, et al. "Emergency management of the COVID‐19 pandemic in a
vascular surgery department of a large metropolitan hospital in Italy.
Preparation, escalation, de‐escalation, and normal activity." Journal
of cardiac surgery (2020).
- Brunasso AMG,
Massone C. Teledermatologic monitoring for chronic cutaneous autoimmune
diseases with smartworking during Covid-19 emergency in a
tertiary center in Italy. Dermatol Ther 2020; e13495.
- Pinto,
F. J., Piñeiro, D., Banerjee, A., Perel, P., Pervan, B., & Eiselé,
J. L. (2021). World Heart Day 2021: COVID-19, digital health, and
tackling cardiovascular disease. The Lancet, 398(10310), 1467-1468
- Luciani
LG, Mattevi D, Cai T, Giusti G, Proietti S, Malossini G. Teleurology in
the Time of Covid-19 Pandemic: Here to Stay? Urology 2020; 140: 4–6.
- Caroppo
E, Lega I, Cognetti D, Rotunno V. Community Mental Health Care in the
COVID-19 Response: An Italian Example. Prim care companion CNS Disord
2020; 22. HTTP://DX.DOI.ORG/10.4088/PCC.20com02659
- Gambardella
C, Pagliuca R, Pomilla G, Gambardella A. COVID-19 risk contagion:
Organization and procedures in a South Italy geriatric oncology
ward. J Geriatr Oncol 2020; published online May. HTTP://DX.DOI.ORG/10.1016/j.jgo.2020.05.008
- Starace
F, Ferrara M. COVID-19 disease emergency operational instructions for
Mental Health Departments issued by the Italian Society of
Epidemiological Psychiatry. Epidemiol Psychiatr Sci 2020; 29: e116.
- Omboni S. Telemedicine During The COVID-19 in Italy: A Missed Opportunity? Telemed J E Health 2020; 00: 19–21.
- Volpato
S, Landi F, Incalzi RA. A Frail Health Care System for an Old
Population: Lesson form the COVID-19 Outbreak in Italy. J
Gerontol A Biol Sci Med Sci 2020; published online April. HTTP://DX.DOI.ORG/10.1093/gerona/glaa087
- Giansanti
D. The Italian Fight Against the COVID-19 Pandemic in the Second Phase:
The Renewed Opportunity of Telemedicine. Telemed e-Health 2020;00:1–4. http://dx.doi.org/10.1089/tmj.2020.0212
- Perrone
G, Zerbo S, Bilotta C, Malta G, Argo A. Telemedicine during Covid-19
pandemic: Advantage or critical issue? Med Leg J
2020; 002581722092692.
- Sossai P, Uguccioni S, Casagrande S. Telemedicine and the 2019 Coronavirus (SARS-CoV-2). Int J Clin Pract; n/a: e13592.
- Goulabchand
R, Claret P-G, Lattuca B. What if the worst consequences of COVID-19
concerned non-COVID patients? J Infect Public Health 2020. https://doi.org/10.1016/j.jiph.2020.06.014
- Holler
JG, Eriksson R, Jensen TØ, van Wijhe M, Fischer TK, Søgaard OS,
Israelsen SB, Mohey R, Fabricius T, Jøhnk F, Wiese L, Johnsen S, Søborg
C, Nielsen H, Kirk O, Madsen BL, Harboe ZB. First wave of COVID-19
hospital admissions in Denmark: a Nationwide population-based cohort
study. BMC Infect Dis. 2021 Jan 9;21(1):39. http://dx.doi.org/10.1186/s12879-020-05717-w PMID: 33421989; PMCID: PMC7794638.
- Bignamini
E, Cazzato S, Cutrera R, et al. Italian pediatric respiratory society
recommendations on pediatric pulmonary function testing during
COVID-19 pandemic. Ital. J. Pediatr. 2020; 46: 68.
- Salzano
A, D’Assante R, Stagnaro FM, et al. Heart failure management during
COVID-19 outbreak in Italy. Telemedicine experience from a heart
failure university tertiary referral centre. Eur. J. Heart Fail. 2020;
published online May. HTTP://DX.DOI.ORG/10.1002/ejhf.1911
- Mureddu
GF, Ambrosetti M, Venturini E, et al. Cardiac rehabilitation activities
during the COVID-19 pandemic in Italy. Position Paper of the AICPR
(Italian Association of Clinical Cardiology, Prevention and
Rehabilitation). Monaldi Arch Chest Dis 2020; 90. HTTP://DX.DOI.ORG/10.4081/monaldi.2020.1439
- Scaldaferri
F, Pugliese D, Privitera G, et al. Impact of COVID-19 pandemic on the
daily management of biotechnological therapy in inflammatory bowel
disease patients: Reorganisational response in a high-volume Italian
inflammatory bowel disease centre. United Eur Gastroenterol J
2020; 1–7.
- Danese S, Ran ZH, Repici A,
et al. Gastroenterology department operational reorganisation at the
time of covid-19 outbreak: An Italian and Chinese experience. Gut
2020; 1–3.
- Siniscalchi M, Zingone F,
Savarino EV, D’Odorico A, Ciacci C. COVID-19 pandemic perception in
adults with celiac disease: an impulse to implement the use of
telemedicine: COVID-19 and CeD. Dig liver Dis Off J Ital
Soc Gastroenterol Ital Assoc Study Liver 2020; published online
May. HTTP://DX.DOI.ORG/10.1016/j.dld.2020.05.014
- Catassi
GN, Vallorani M, Cerioni F, Lionetti E, Catassi C. A negative fallout
of COVID-19 lockdown in Italy: life-threatening delay in the
diagnosis of celiac disease. Dig liver Dis Off J Ital Soc
Gastroenterol Ital Assoc Study Liver 2020; published online May.
HTTP://DX.DOI.ORG/10.1016/j.dld.2020.05.016 - Rubin
DT, Abreu MT, Rai V, Siegel CA. Management of Patients With Crohn’s
Disease and Ulcerative Colitis During the Coronavirus
Disease-2019 Pandemic: Results of an International Meeting.
Gastroenterology. 2020; published online April. HTTP://DX.DOI.ORG/10.1053/j.gastro.2020.04.002
- Curigliano
G. How to Guarantee the Best of Care to Patients with Cancer During the
COVID‐19 Epidemic: The Italian Experience. Oncologist 2020. HTTP://DX.DOI.ORG/10.1634/theoncologist.2020-0267
- Gebbia
V, Piazza D, Valerio MR, Borsellino N, Firenze A. Patients With Cancer
and COVID-19: A WhatsApp Messenger-Based Survey of Patients’
Queries, Needs, Fears, and Actions Taken. JCO Glob Oncol 2020; 6: 722–9.
- Buonomo
OC, Materazzo M, Pellicciaro M, Caspi J, Piccione E, Vanni G. Tor
Vergata University-Hospital in the Beginning of COVID-19-Era:
Experience and Recommendation for Breast Cancer Patients. In Vivo 2020;
34: 1661–5.
- Viale G, Licata L, Sica L, et al.
Personalized Risk-Benefit Ratio Adaptation of Breast Cancer Care at the
Epicenter of COVID-19 Outbreak. Oncologist 2020; published online
May. HTTP://DX.DOI.ORG/10.1634/theoncologist.2020-0316
- Corsi
F, Caruso A, Albasini S, et al. Management of breast cancer in an
EUSOMA-accredited Breast Unit in Lombardy, Italy, during the COVID-19
pandemic. Breast J 2020; n/a. HTTP://DX.DOI.ORG/10.1111/tbj.13926
- Rossi
B, Zoccali C, Baldi J, et al. Reorganization Tips from a Sarcoma Unit
at Time of the COVID-19 Pandemic in Italy: Early Experience from
a Regional Referral Oncologic Center. J Clin Med 2020; 9. HTTP://DX.DOI.ORG/10.3390/jcm9061868.
- DOCUMENTO
DI INDIRIZZO PER LA VALUTAZIONE E LA GESTIONE DEL RISCHIO DEI PAZIENTI
E DEGLI OPERATORI NEI REPARTI DI RADIOTERAPIA ONCOLOGICA IN CORSO DI
DIFFUSIONE DEL COVID-19. www.radioterapiaitalia.it (accessed July 4, 2020).
- Tomelleri
A, Sartorelli S, Campochiaro C, Baldissera EM, Dagna L. Impact of
COVID-19 pandemic on patients with large-vessel vasculitis in Italy:
a monocentric survey. Ann. Rheum. Dis. 2020; published online
April. HTTP://DX.DOI.ORG/10.1136/annrheumdis-2020-217600
- Minniti
A, Maglione W, Pignataro F, Cappadona C, Caporali R, Del Papa N. Taking
care of systemic sclerosis patients during COVID-19 pandemic: rethink
the clinical activity. Clin Rheumatol 2020; 39: 2063–5.
- Malipiero
G, Paoletti G, Puggioni F, et al. An academic allergy unit during
COVID-19 pandemic in Italy. J. Allergy Clin. Immunol. 2020; published
online April. HTTP://DX.DOI.ORG/10.1016/j.jaci.2020.04.003
- Pulvirenti
F, Cinetto F, Milito C, et al. Health-Related Quality of Life in Common
Variable Immunodeficiency Italian Patients Switched to Remote
Assistance During the COVID-19 Pandemic. J Allergy Clin Immunol Pract
2020; 8: 1894-1899.e2.
- Cocci A, Presicce F,
Russo GI, Cacciamani G, Cimino S, Minervini A. How sexual medicine is
facing the outbreak of COVID-19: experience of Italian urological
community and future perspectives. Int J Impot Res 2020; 1–3.
- Rizzo
M, Liguori G, Verze P, Palumbo F, Cai T, Palmieri A. How the
andrological sector suffered from the dramatic Covid 19 outbreak in
Italy: supportive initiatives of the Italian Association of
Andrology (SIA). Int J Impot Res 2020; 1–2.
- La
Marca A, Niederberger C, Pellicer A, Nelson SM. COVID-19: lessons from
the Italian reproductive medical experience. Fertil. Steril. 2020; 113:
920–2.
- Requena A, Cruz M, Vergara V, Prados
N, Galliano D, Pellicer A. A picture of the covid-19 impact on IVIRMA
fertility treatment clinics in Spain and Italy. Reprod Biomed
Online 2020; 41: 1–5.
- De Santis L, Anastasi
A, Cimadomo D, et al. COVID-19: the perspective of Italian
embryologists managing the IVF laboratory in pandemic emergency.
Hum. Reprod. 2020; 35: 1004–5.
- Corona G,
Baldi E, Isidori AM, et al. SARS-CoV-2 infection, male fertility and
sperm cryopreservation: a position statement of the Italian
Society of Andrology and Sexual Medicine (SIAMS) (Società Italiana di
Andrologia e Medicina della Sessualità). J Endocrinol Invest 2020; :
1–5.
- Vaiarelli A, Bulletti C, Cimadomo D, et
al. COVID-19 and ART: the view of the Italian Society of Fertility and
Sterility and Reproductive Medicine. 2020.
- Grazzi
L, Rizzoli P. The Adaptation of Management of Chronic Migraine Patients
With Medication Overuse to the Suspension of Treatment Protocols
During the COVID-19 Pandemic: Lessons From a Tertiary Headache Center
in Milan, Italy. Headache 2020; published online April. HTTP://DX.DOI.ORG/10.1111/head.13825
- Sechi
A, Macor D, Valent S, et al. Impact of COVID-19 related healthcare
crisis on treatments for patients with lysosomal storage
disorders, the first Italian experience. Mol Genet Metab 2020; 130:
170–1.
- Dubbioso R, Nobile-Orazio E,
Manganelli F, et al. Dealing with immune-mediated neuropathies during
COVID-19 outbreak: practical recommendations from the task force
of the Italian Society of Neurology (SIN), the Italian Society of
Clinical Neurophysiology (SINC) and the Italian Peripheral Nervous
System . Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc.
Clin. Neurophysiol. 2020; 41: 1345–8.
- Capozzo
R, Zoccolella S, Musio M, Barone R, Accogli M, Logroscino G.
Telemedicine is a useful tool to deliver care to patients with
Amyotrophic Lateral Sclerosis during COVID-19 pandemic: results from
Southern Italy. Amyotroph Lateral Scler Front Degener 2020; : 1–7.
- Bersano A, Pantoni L. On being a neurologist in Italy at the time of the COVID-19 outbreak. Neurology 2020; 94: 905—906.
- Schirinzi
T, Cerroni R, Di Lazzaro G, et al. Self-reported needs of patients with
Parkinson’s disease during COVID-19 emergency in Italy. Neurol
Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol 2020;
41: 1373–5
- Tornese G, Ceconi V, Monasta L,
Carletti C, Faleschini E, Barbi E. Glycemic Control in Type 1 Diabetes
Mellitus During COVID-19 Quarantine and the Role of In-Home Physical
Activity. Diabetes Technol Ther 2020; 22. HTTP://DX.DOI.ORG/10.1089/dia.2020.0169
- Maria
B, Federico B, Angelo B. Glycaemic Control Among People with Type 1
Diabetes During Lockdown for the SARS-CoV-2 Outbreak in Italy. Diabetes
Ther 2020. HTTP://DX.DOI.ORG/10.1007/s13300-020-00829-7
- Capaldo
B, Annuzzi G, Creanza A, et al. Blood Glucose Control During Lockdown
for COVID-19: CGM Metrics in Italian Adults With Type 1 Diabetes.
Diabetes Care 2020. HTTP://DX.DOI.ORG/10.2337/dc20-1127
- Brunasso
AMG, Massone C. Teledermatologic monitoring for chronic cutaneous
autoimmune diseases with smartworking during Covid-19 emergency
in a tertiary center in Italy. Dermatol Ther 2020; : e13495.
- Marasca
C, Ruggiero A, Megna M, Annunziata MC, Fabbrocini G. Biologics for
patients affected by hidradenitis suppurativa in the COVID-19
era: data from a referral center of Southern Italy. J.
Dermatolog. Treat. 2020; : 1.
- Villani A,
Megna M, Scalvenzi M, Fabbrocini G, Ruggiero A. Teledermatology and
chronic skin diseases: real life experience in a Southern Italian
Dermatologic Centre. Dermatol Ther 2020; n/a: e13839.
- de
Girolamo G, Cerveri G, Clerici M, et al. Mental Health in the
Coronavirus Disease 2019 Emergency-The Italian Response. JAMA
psychiatry 2020; published online April. HTTP://DX.DOI.ORG/10.1001/jamapsychiatry.2020.1276
- D’Agostino
A, Demartini B, Cavallotti S, Gambini O. Mental health services in
Italy during the COVID-19 outbreak. The lancet. Psychiatry. 2020; 7:
385–7.
- Percudani M, Corradin M, Moreno M,
Indelicato A, Vita A. Mental Health Services in Lombardy during
COVID-19 outbreak. Psychiatry Res 2020; 288: 112980.
- Fagiolini A, Cuomo A, Frank E. COVID-19 Diary From a Psychiatry Department in Italy. J Clin Psychiatry 2020; 81. HTTP://DX.DOI.ORG/10.4088/JCP.20com13357
- Tullio
V, Perrone G, Bilotta C, Lanzarone A, Argo A. Psychological support and
psychotherapy via digital devices in Covid-19 emergency time:
Some critical issues. Med Leg J 2020; :5817220926942.
- Carpiniello
B, Tusconi M, di Sciascio G, Zanalda E, di Giannantonio M, Psychiatry
EC of the IS of. Mental health services in Italy during the Covid-19
Pandemic. Psychiatry Clin Neurosci 2020; 10.1111/pcn.13082.
- Zucchetti
G, Bertolotti M, Fagioli F. How Paediatric Psycho-oncology is changing
during the COVID-19 Epidemic in Italy: New approaches. Psychooncology;
n/a. HTTP://DX.DOI.ORG/10.1002/pon.5444
- Balduzzi
A, Brivio E, Rovelli A, et al. Lessons after the early management of
the COVID-19 outbreak in a pediatric transplant and hemato-oncology
center embedded within a COVID-19 dedicated hospital in Lombardia,
Italy. Estote parati. Bone Marrow Transplant 2020. HTTP://DX.DOI.ORG/10.1038/s41409-020-0895-4
- Brunetti-pierri
N, Fecarotta S, Staiano A, Strisciuglio P, Parenti G. Ensuring
continuity of care for children with inherited metabolic diseases at
the time of COVID-19 : the experience of a metabolic unit in Italy.
Genet Med 2020; 0: 3–5.
- Cardinale F, Ciprandi
G, Barberi S, et al. Consensus statement of the Italian society of
pediatric allergy and immunology for the pragmatic management of
children and adolescents with allergic or immunological diseases during
the COVID-19 pandemic. Ital J Pediatr 2020; 46: 84.
- Mascagni
D, Eberspacher C, Mascagni P, et al. From high volume to ‘zero’
proctology: Italian experience in the COVID era. Int J Colorectal Dis
2020; 1–4.
- SAGES and EAES Recommendations Regarding Surgical Response to COVID-19 Crisis - SAGES. https://www.sages.org/recommendations-surgical-response-covid-19/ (accessed July 4, 2020).
- Usuelli
FG, D’Ambrosi R. Being a foot and ankle surgeon in Italy in the era of
COVID-19. Knee Surg. Sports Traumatol. Arthrosc. 2020; 28: 1679–82
- Angileri
FF, Sabatino G, Cavallo LM, et al. Natura non facit saltus: a phase 2
proposal to manage brain tumors cases from the neuro-oncology
section of the Italian Society of Neurosurgery (SINch®). J Neurosurg
Sci 2020; published online June. HTTP://DX.DOI.ORG/10.23736/S0390-5616.20.05054-7
- Ciavattini
A, Delli Carpini G, Giannella L, et al. Expert consensus from the
Italian Society for Colposcopy and Cervico-Vaginal Pathology (SICPCV)
for colposcopy and outpatient surgery of the lower genital tract during
the COVID-19 pandemic. Int J Gynecol Obstet 2020; 149: 269–72.
- Sciarra
A, Salciccia S, Maggi M, et al. Elective procedures for prostate cancer
in the time of Covid-19: a multidisciplinary team experience.
Prostate Cancer Prostatic Dis 2020; : 1–3.
- Luciani
LG, Mattevi D, Cai T, Giusti G, Proietti S, Malossini G. Teleurology in
the Time of Covid-19 Pandemic: Here to Stay? Urology 2020; 140: 4–6.
- Negrini
S, Kiekens C, Bernetti A, et al. Telemedicine from research to practice
during the pandemic. ‘Instant paper from the field’ on
rehabilitation answers to the Covid-19 emergency. Eur J Phys Rehabil
Med 2020; published online April. HTTP://DX.DOI.ORG/10.23736/S1973-9087.20.06331-5
- Boldrini
P, Bernetti A, Fiore P. Impact of COVID-19 outbreak on rehabilitation
services and Physical and Rehabilitation Medicine (PRM) physicians’
activities in Italy. An official document of the Italian PRM Society
(SIMFER). Eur J Phys Rehabil Med 2020. HTTP://DX.DOI.ORG/10.23736/S1973-9087.20.06256-5
- Boldrini
P, Kiekens C, Bargellesi S, et al. First impact on services and their
preparation. ‘Instant paper from the field’ on rehabilitation answers
to the Covid-19 emergency. Eur J Phys Rehabil Med 2020. HTTP://DX.DOI.ORG/10.23736/S1973-9087.20.06303-0
- Pedersini
P, Corbellini C, Villafañe JH. Italian Physical Therapists’ Response to
the Novel COVID-19 Emergency. Phys Ther 2020; published online April
13. HTTP://DX.DOI.ORG/10.1093/ptj/pzaa060
- Iannaccone
S, Castellazzi P, Tettamanti A, et al. Role of Rehabilitation
Department for Adult Covid-19 Patients: the Experience of the San
Raffaele Hospital of Milan. Arch Phys Med Rehabil 2020. HTTP://DX.DOI.ORG/10.1016/j.apmr.2020.05.015
Supplementary Material
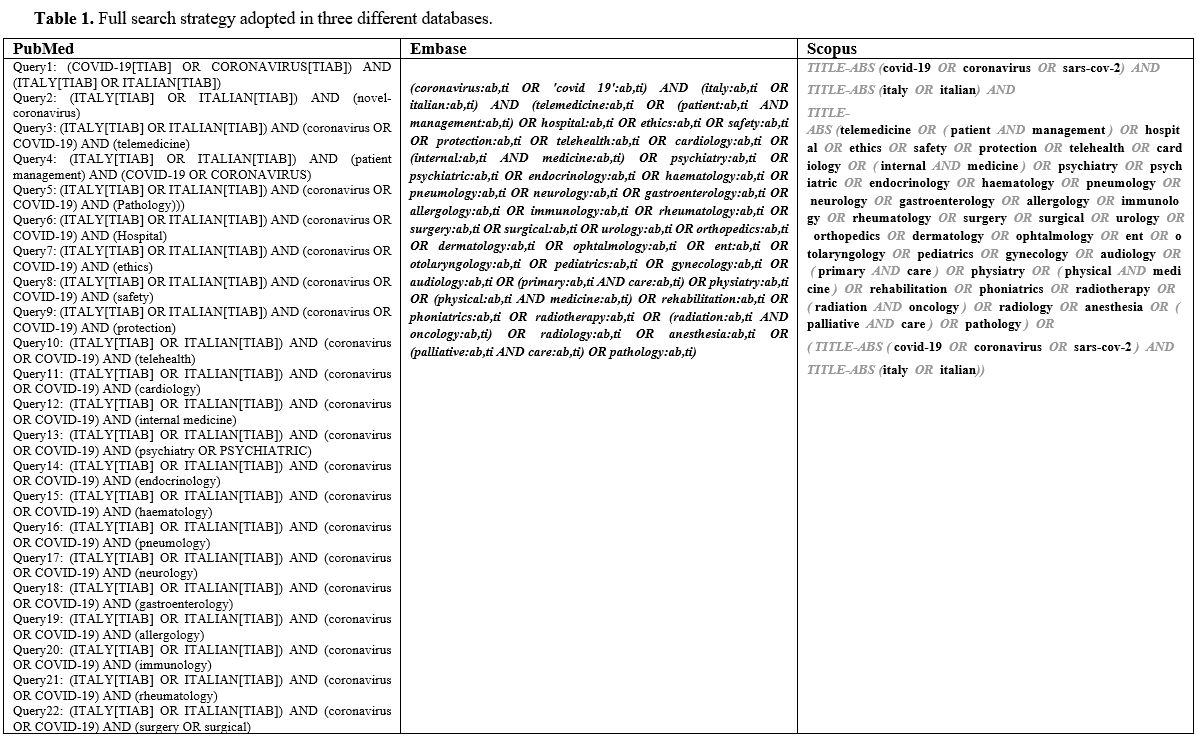 |
Table
1. Full search strategy adopted in three different databases. |
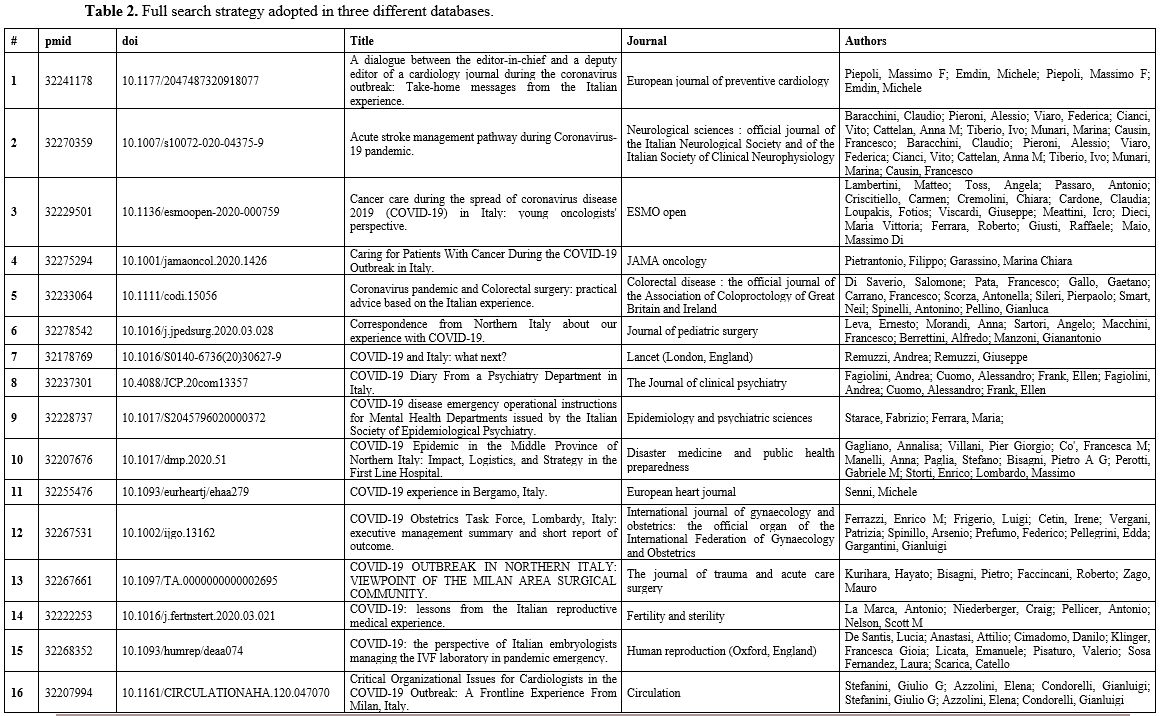 |
Table 2. Full search strategy adopted in three different databases. |
[TOP]