Mario Schiavoni1, Carlo Pruneti2, Sara Guidotti2, Alessandra Moscatello3, Francesca Giordano4, Antonella Coluccia5, Rita Carlotta Santoro6, Maria Francesca Mansueto7, Ezio Zanon8, Renato Marino9, Isabella Cantori10 and Raimondo De Cristofaro11.
1 Past
Director of Hemophilia and Rare Coagulopathies Center - Dept. of
Internal Medicine, "I. Veris Delli Ponti" Hospital-Scorrano-ASL Lecce,
Italy.
2 Clinical Psychology, Clinical
Psychophysiology, and Clinical Neuropsychology Labs., Dept. of Medicine
and Surgery, University of Parma, Italy.
3 Penitentiary Medicine - Socio-sanitary District ASL-Lecce, Italy.
4 Service of Pathological Addictions-Gallipoli-ASL Lecce, Italy.
5
Hemophilia and Rare Coagulopathies Center -Dept. of Internal Medicine,
" I. Veris Delli Ponti" Hospital-Scorrano-ASL Lecce, Italy.
6 Hemostasis and Thrombosis Unit, Pugliese-Ciaccio Hospital, Catanzaro, Italy.
7
Regional Reference Center for Coagulopathies in Children and Adults,
Hematology Unit, Oncology Dept.- Policlinico University, Palermo, Italy.
8
Multidisciplinary HUB Regional Center for Prevention, Prophylaxis, and
Advanced Treatment of Hemophilic Arthropathy, General Medicine
University Hospital of Padua, Italy.
9 Hemophilia and Thrombosis Center, Policlinico-University, Bari, Italy.
10 Haemophilia Center, Department of Transfusion Medicine, Hospital of Macerata, Macerata, Italy.
11 Hemorrhagic and Thrombotic Diseases Center, Foundation "A. Gemelli" IRCCS University Hospital, Rome, Italy.
Correspondence to: Mario
Schiavoni. Past Director of Hemophilia and Rare Coagulopathies Center
- Dept. of Internal Medicine, "I. Veris Delli Ponti"
Hospital-Scorrano-ASL Lecce, Italy. E-mail:
marioschiavoni@gmail.com
Published: January 1, 2023
Received: September 22, 2022
Accepted: December 19, 2022
Mediterr J Hematol Infect Dis 2023, 15(1): e2023005 DOI
10.4084/MJHID.2023.005
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background:
The health-related quality of life (HRQoL) of people with hemophilia
(PWH) is an important issue, especially considering people suffering
from chronic diseases beyond hemophilia. The principal aim of this
study was to investigate the presence and relevance of psychological
symptoms, both internalizing and externalizing, lifestyle, and HRQoL in
a group of Italian PWH with chronic bloodborne co-infections and
comorbidities. Furthermore, the research describes the association
between psychological aspects and the impact of disease-related
characteristics (type of hemophilia, presence of co-infections, and
comorbidities) on them.
Methods:
Seventy patients (mean age 46.77±11.3), 64 with severe hemophilia A
(Factor VIII: C < 1 IU/dL) and 6 with severe hemophilia B (Factor IX
<1 IU/dL), were consecutively recruited from seven Hemophilia
Centers in Italy of Italian Association of Hemophilia Centers (AICE).
In order to assess psychological symptoms, HRQoL, and lifestyle, three
psychological questionnaires were administered (the SCL-90-R, SF-36,
and PSQ, respectively).
Results:
A general decline in the quality of life and an increase in the
tendency to adopt a lifestyle characterized by hyperactivity emerged.
Inverse correlations were found between HRQoL and psychological
distress. Although the SCL-90-R did not reveal symptoms above the
clinical cut-off, co-infections significantly increased anxiety,
depression, somatizations, paranoia, and social withdrawal. Lastly,
HRQoL is impaired by co-infections as well as comorbidities.
Conclusion: Our preliminary results must be confirmed to deepen the findings between mental health and hemophilia.
|
Introduction
Hemophilia
is an inherited hemorrhagic disorder that, in the most severe forms,
causes deep physical and psychological discomfort, mainly due to often
life-threatening bleeding. In the last 20 years, great progress in the
multidisciplinary management of PWH has been achieved. The availability
of increasingly innovative replacement and non-substitutive treatments
given on prophylaxis has radically changed the expectancy and the
HRQoL, particularly in the younger generations with severe hemophilia A
and B.[1]
Several previous studies investigated
the presence of psychological symptoms and the HRQoL in PWH. Most
research agrees with the idea that specific factors in the medical
history can determine a decline in specific components of HRQoL, such
as physical activity, physical health, and social and interpersonal
functioning.[2-5] Other studies underlined the role of factors such as work status and perceived physical pain.[6,7]
Nevertheless, many problems are still associated with older adults
affected by age-related comorbidities (diabetes, cardiovascular and
respiratory diseases, renal insufficiency, cancer, etc.) that require
specialized medical and psychological interventions. It is well known
that the most serious comorbidities are chronic liver diseases closely
related to hepatitis B (HBV) and hepatitis C (HCV) infections, as well
as the sequelae caused by the human immunodeficiency virus (HIV)[8,9]
occurred in the 70-80s by the use of not virus-inactivated
plasma-derived concentrates. However, even though vaccination against
hepatitis B definitively defeated the virus in new generations,
specific therapies against hepatitis C were applied,[10] and combined therapy with highly active anti-retroviral drugs slowed the progression of HIV,[11]
these infections keep on influence the concept of the disease and still
have an impact on the mental health of people affected.[12]
The
psychological dynamics in HIV-positive PWH were analyzed over the years
by considering various parameters. Increased stress and anxiety in a
population of HIV-positive hemophiliacs were observed. In addition,
psychosocial problems related to the level of school education,
familiarity with psychiatric illnesses, or a couple of problems were
also described. More specifically, HIV-positives showed a greater
negative impact on their sexual behaviors with a significantly higher
prevalence of sexual dysfunctions than HIV-negatives.[13]
However, completely different results were found by Italian authors
that demonstrated that HIV-negative hemophiliacs have worse anxiety and
depression scores, reporting more confusion and fear, than
HIV-positives.[14]
At the same time, many
research projects help to understand how to address these issues and
manage physical and psychological symptoms associated with HIV
infection.[15] Similarly, changes in psychological dynamics are also observed in hemophiliacs with age-related comorbidities.[16]
The
current literature still highlights the need to investigate these
aspects further and broaden the clinical interest in psychological
symptoms not yet evaluated. For instance, relevant emotional reactions
towards the disease were neglected, such as the presence of
externalizing symptoms (anger/hostility, paranoid ideation, etc.)
typical in the literature discussing other severe chronic diseases
(obstructive pulmonary disease, multiple sclerosis, alexithymia).[17-20]
Aims of the study.
The main purpose of our research was to describe specific psychological
aspects: psychopathological symptoms, both internalizing (anxiety,
somatic complaints, obsessions and compulsions, depression) and
externalizing (hostility, paranoia, psychoticism, etc.), lifestyle, and
HRQoL in a hemophiliac sample. A further objective was to highlight the
possible association between the psychological aspects mentioned above.
Lastly, the impact of specific factors related to hemophilia (type A or
B, co-infections, and comorbidities) on the psychological dimensions
was investigated.
Materials and Methods
Participants and Study design.
In this multicenter observational study, 70 PWH (64 with severe
hemophilia A: Factor VIII: C < 1 IU/dL and 6 with severe hemophilia
B: Factor IX <1 IU/dL) were consecutively recruited from seven
Italian Hemophilia Centers (Bari, Catanzaro, Macerata, Padova, Roma,
Palermo, and Scorrano) belonging to AICE. Criteria for inclusion in the
study were age > 18 years old; medical diagnosis of hemophilia;
absence of sensory disturbances of sight and/or hearing that limit the
administration of the tests (i.e., previous head trauma, neurological
condition, alcoholism, or substance abuse, or neoplasms).
Ethical considerations.
Informed consent was required from all persons, as well as the approval
of the Ethics Committees of the respective Hemophilia Centers. This
study complies with the Declaration of Helsinki and Italian privacy law
(Legislative decree No. 196/2003). No treatments or false feedback were
given, and no potentially harmful evaluation methods were used.
Participation was voluntary, and participants could drop out at any
time without any negative consequences. All data were stored only by
using an anonymous ID for each participant. Subjects' anonymity was
preserved, and the data obtained were used solely for scientific
purposes.
Measures.
After an accurate clinical interview, PWH underwent a
psychopathological assessment procedure by administering three
psychometric tests.
The Symptom Checklist-90-Revised was used to
investigate internalizing and externalizing symptoms such as
Somatization (SOM), Obsessive-compulsive (O-C), Interpersonal
Hypersensitivity (I-S), Depression (DEP), Anxiety (ANX), Hostility
(HOS), Phobic Anxiety (PHOB), Paranoid Ideation (PAR), and Psychoticism
(PSY) (cut-off=1.00).[21] The SCL-90-R provides three
global indices: the Global Severity Index (GSI) represents the
intensity of the level/depth of the distress; the Positive Symptom
Total (PST) corresponds to the total number of symptoms, and the
Positive Symptom Distress Index (PSDI) is used as an index of the
subject's response style to the suffering.[22,23]
The
Short Form Health Survey (SF-36) was administered to evaluate the
HRQoL. It is composed of eight scales: Physical Functioning (PF), Role
(limitations) Physical (RP), General Health (GH), Bodily Pain (BP),
Vitality (VT), Role (limitations), Emotional (RE), Mental Health (MH),
and Social Functioning (SF). Questions and sub-scales of the SF-36 are
organized so that a higher score represents better health of the
subject.[24]
The P Stress Questionnaire (PSQ)
was performed to detect whether there is a present risk for
stress-related physical disorders attributable to some characteristics
of the personality configuration known as "Type A behavior".[25]
The PSQ tool made up of 32 items, grouped into six scales: Sense of
Responsibility (SR), Vigor (V), Stress Disorders (SD), Precision and
Punctuality (PP), Spare Time (ST), and Hyperactivity (H). The
standardization provides conversion into Stanine scores that are proper
for scores that do not fall below 10 standard deviations. The Stanine
(STAndard NINE) is a method of scaling test scores that have a
distribution between 1 and 9 with mean=5 and standard deviation=1.96.
Statistical analysis.
Statistical analysis was performed using Microsoft Excel and IBM SPSS
Statistics software (Version 28.0.1.0). Considering the small sample
size and the presence of unbalanced groups when divided by type of
hemophilia, co-infections, and comorbidities, non-parametric
statistical analyses were computed. First, descriptive analyses on the
total sample were conducted: average values (mean and standard
deviation) of the scores obtained from the total sample in the
SCL-90-R, SF-36, and PSQ scales were calculated. In order to highlight
possible associations between the psychological dimensions assessed, a
Spearman Correlation was then performed considering the sub-scales of
the SCL-90-R and the total scores of the SF-36 and the PSQ. In order to
investigate the impact of specific factors related to hemophilia (type
of disease, presence of co-infections, and comorbidities) on the
psychological aspects assessed, the following analyses were made: a
Mann-Whitney U tests for independent samples were used to calculate
possible significant differences between type A group vs. Type B group
considering symptoms (SCL-90-R), lifestyle (PSQ), and HRQoL (SF-36); a
Mann-Whitney U tests for independent samples were made to detect
possible significant differences between a co-infections group compared
with a group without co-infections considering symptoms (SCL-90-R),
lifestyle (PSQ), and HRQoL (SF-36); finally a Mann-Whitney U tests for
independent samples was performed in order to assess possible
significant differences between groups with comorbidities compared with
a group without comorbidities taking into account symptoms (SCL-90-R),
lifestyle (PSQ), and HRQoL (SF-36).
Results
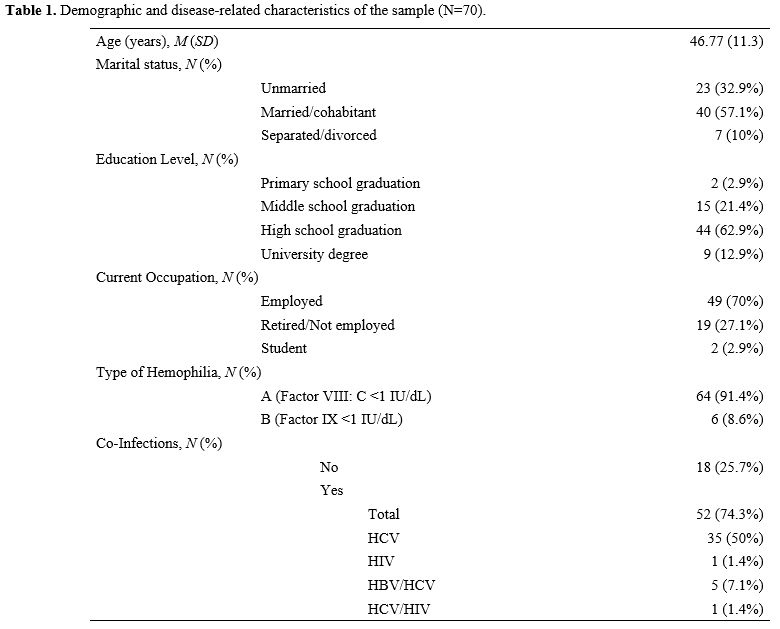
Description of the Sample. Demographic and disease-related characteristics of the total sample are shown in Table 1.
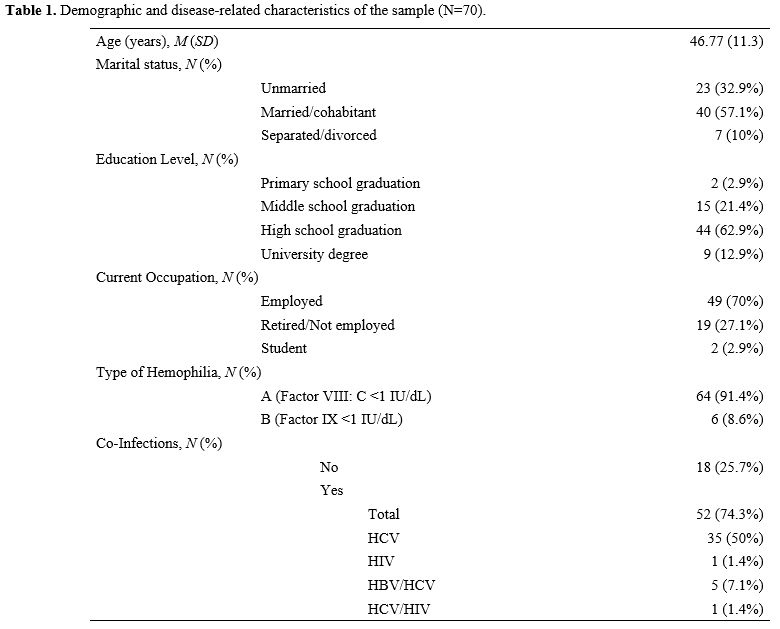 |
- Table 1. Demographic and disease-related characteristics of the sample (N=70).
|
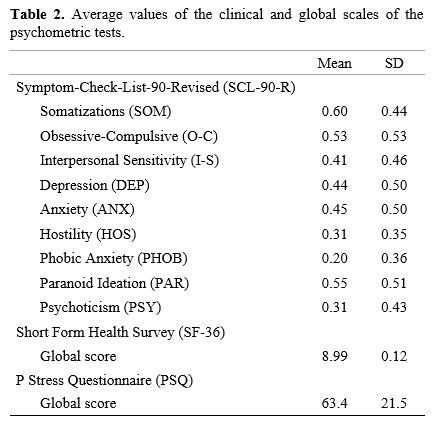
Descriptive analysis of the total sample.
Firstly, the SCL-90-R did not show scores indicative of
psychopathological symptoms of relevance (above the clinical cut-off of
1.00) while, considering the global score of the SF-36, a tendency to
perceive an impoverishment in one's health in the last year emerged.
Lastly, the descriptive analysis conducted on the total score of the
PSQ highlights the tendency to adopt behaviors and lifestyles
characterized by a high sense of responsibility, vigor, precision and
punctuality, hyperactivity, and somatic complaints (Table 2).
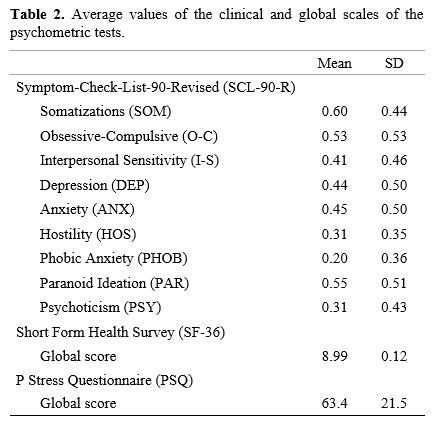 |
- Table 2. Average values of the clinical and global scales of the psychometric tests.
|
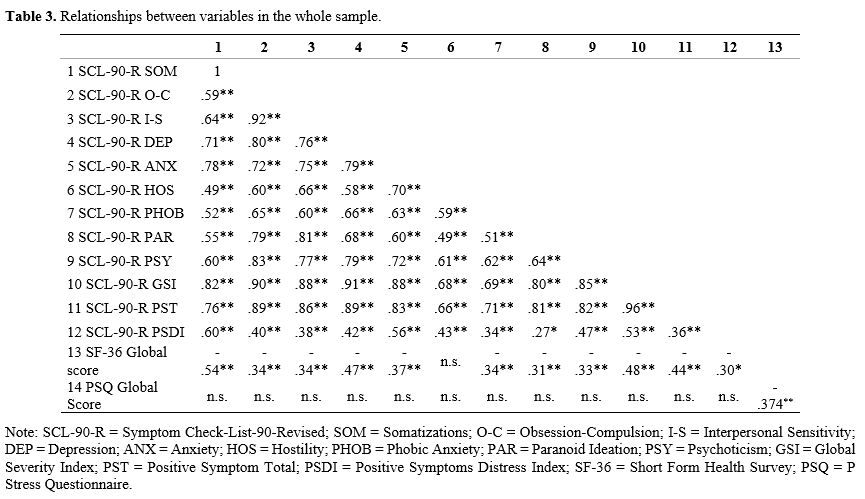
About
the three measures, the possible linear relation between them was
investigated through Spearman's Rho coefficient. In addition to the
significant associations that emerged between all the clinical and
global scales of the SCL-90-R, significant correlations can be observed
between the global score of the SF-36 and those of the SCL-90-R. More
specifically, it appears that psychological symptoms increase as the
quality-of-life decreases. However, an opposite trend can be
hypothesized: as the state of physical and mental health decreases,
symptoms related to anxiety, phobic anxiety, depression, obsession and
compulsion, somatic complaints, interpersonal hypersensitivity,
paranoid ideation, and psychoticism increase. Furthermore, the global
score of the SF-36 shows a moderate inverse correlation with the global
score of the PSQ (Table 3).
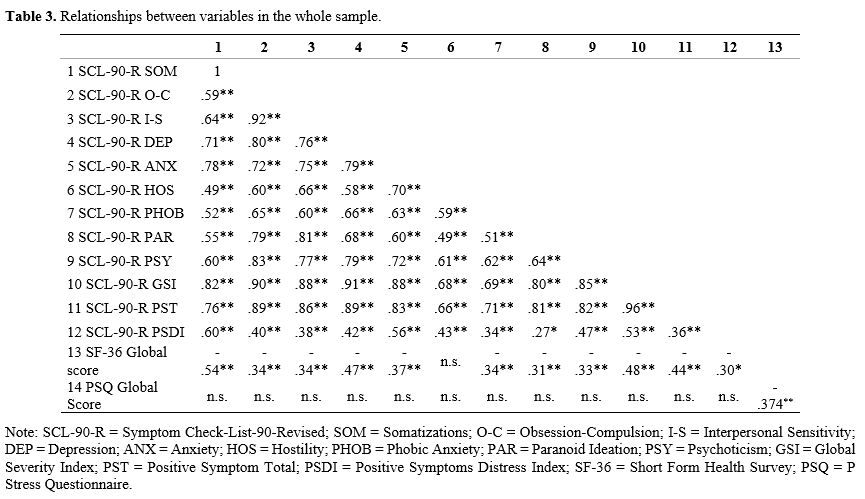 |
- Table 3. Relationships between variables in the whole sample.
|
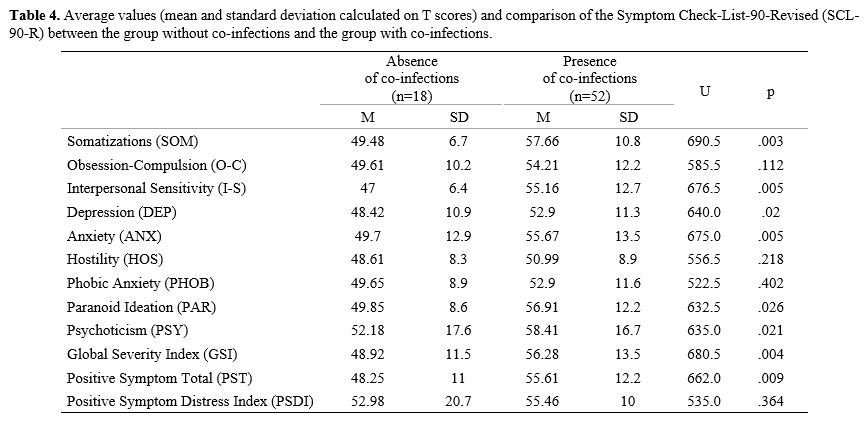
Comparison between sub-groups.
In order to identify any significant differences in the manifestation
of psychological distress attributable to disease-related
characteristics (type A or B, presence or not of co-infections and
comorbidities), the differences between these groups were assessed. The
comparison of the scores of the SCL-90-R, SF-36, and PSQ according to
the type of hemophilia (A or B) did not show noteworthy aspects. For
none of these scales, there were no significant differences. On the
contrary, the Mann-Whitney's U test that compared the scores of the
psychological measures considering the presence of co-infections vs.
the absence of co-infections highlighted noteworthy aspects. More
specifically, significant differences between groups emerge both for
SCL-90-R and for SF-36. It seems that co-infections presence favors an
increase in psychological symptoms, internalizing, such as somatic
complaints, interpersonal hypersensitivity, depression, anxiety, and
externalizing, such as paranoid ideation and psychoticism. The scores
of two global indices, the GSI and PST, are also significantly higher
in the group with co-infections (Table 4).
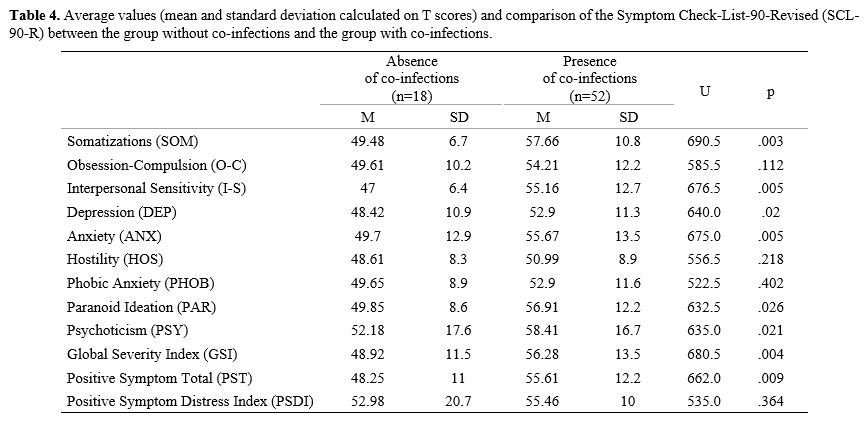 |
- Table 4. Average
values (mean and standard deviation calculated on T scores) and
comparison of the Symptom Check-List-90-Revised (SCL-90-R) between the
group without co-infections and the group with co-infections.
|
Furthermore,
the co-infections presence determines a statistically significant
worsening of the quality of life (U=270.5; p=.008).
The Mann
Whitney's U test was also performed to investigate possible differences
in the scores of SCL-90-R, SF-36, and PSQ between a group of PWH with
comorbidities and a group of PWH without comorbidities. No significant
differences emerge between these two groups, neither in the symptoms
assessed with the SCL-90-R scale nor in the behavioral and lifestyle
aspects investigated through the PSQ. Conversely, the presence of other
medical diseases in the anamnesis favors a reduction in the level of
HRQoL (U=251.0; p=.01).
Discussion
On
a descriptive level, the most interesting result is the significantly
high average score on the PSQ. These data indicate the frequent
tendency to adopt a lifestyle at risk of stress-related physical
disorders and behavior characterized by a high sense of responsibility,
vigor, hyperactivity, precision and punctuality, and reduced ability to
take free time from working activities. In this sample, one could
assume that there is a tendency to adopt a lifestyle that does not
favor the achievement of psychophysical balance but instead the
tendency to implement potentially risky health behaviors. Clinical
hypotheses are connected to the possible presence of an underestimation
of risk in terms of denial of illness and non-acceptance of the role of
the patient. For this reason, in a future perspective of evaluation, it
would be interesting to investigate the subjective perception of
disease connected to the adaptation to it (i.e., by Illness Behavior
Questionnaire).[26] Consistent with what has already
been widely described in the literature, the diagnosis of hemophilia is
envisaged as an obstacle in the life of these people who perceive a
limitation of their activities in favor of the protection of their
body.[5,6,27-29] For instance, some
authors argue that participation in activities, such as sports or
crowded social events, is influenced by the fear of incurring injuries
and bleeding.[30] Moreover, it has highlighted the
role of behavioral precautions, the uncertainty of actions, and the
fear of unexpected bleeding on depression, frustration, isolation, and
embarrassment.[31] Other studies confirmed some
aspects related to comorbidities (arthropathy, HCV/HBV/HIV
co-infections, liver cirrhosis due to HBV/HCV infections, and
coexisting heart and kidney diseases, for example) are ongoing
challenges that block the accepting health status in these persons.[32,33]
As experienced in our sample, the correlation between the perceived
quality of life and the adopted lifestyle further corroborates this
point. It is possible to sustain that a lifestyle characterized by high
activity levels is associated with a decrease in the state of health
perceived by the subject. Hence, the need to pay attention to the
lifestyle of these persons, stress management, positive thinking, and
eating habits emerges.[34]
Focusing on the
psychopathological symptoms, our group recorded no scores above the
clinical cut-off. However, noteworthy aspects emerged by investigating
the correlation between the scores of the other psychometric tests
administered. Confirming what already emerged in previous studies, the
state of health appears to have an inverse correlation with two global
indices of the SCL-90-R.[4,5,28-30]
This information describes the tendency to suffer psychologically more,
as the decline in quality of life, in terms of limitations deriving
from the physical disease, increases. Furthermore, confirming previous
studies, the HRQoL appears to have an inverse correlation with most
psychological symptoms, such as anxiety, phobic anxiety, depression,
obsessions and compulsions, interpersonal hypersensitivity, and somatic
complaints.[3-5,28-30,35]
Moreover, even the scores of paranoid ideation and psychoticism appear
to have an inverse relationship with the HRQoL, highlighting the
additional load of hostility, suspiciousness, withdrawal, and social
isolation on the state of health. However, due to our study's small
sample size, it is impossible to define the causal role of the symptoms
on the deterioration of the HRQoL. The opposite could also be true: a
reduction in psychophysical well-being could lead to mental suffering.
One
of the aims of this research was to investigate some disease-related
characteristics' effects on the observed psychological aspects.
Interesting data were highlighted by comparing the psychological
distress between the group of patients with co-infections with those of
the group without co-infections. Co-infections appear to have an
important role in increasing psychological distress in terms of
internalizing (anxiety, depression, somatic complaints) and
externalizing (paranoia and psychoticism) symptoms. If the last aspect
is considered, the expression of mental suffering on an interpersonal
level has been described for the first time. To our knowledge,
inadequacy, a sense of inferiority, self-depreciation, and
suspiciousness resulting in social withdrawal and isolation were never
detected. Our results effectively deepen previous studies supporting
the data that infections compromise the patient's well-being causing
medical complications and social impairment. Jones and colleagues focus
on HIV infection and argue that there is a possible risk factor for the
appearance of psychological symptoms, even before noticeable physical
signs.[36-40] The psychological dynamics in
HIV-positive PWH were analyzed over the years by considering only
parameters such as stress and the relationship between infections.
Specifically considering HIV and mental suffering, the association is
still confused even now that vaccinations and anti-retroviral therapies
slow the progression of the disease.[12]
Also,
considering the HRQoL, our findings agree with previous studies that
focused on co-infections impact on this aspect. For instance,
Cuesta-Barriuso et al. found significant differences between a group of
PWH with HIV/HCV and the group without co-infections in HRQoL
perceptions, concluding that the emotional representation of the
disease plays an influential role.[28] Consistent
with this assumption, other authors explained this association with the
assumption that the HRQoL would be influenced by the level of
acceptance of the infection and the ability to adapt to illness.[38,41,42,43]
Our
study underlines another aspect referred to as the HRQoL. It has been
observed that comorbidities affect the global perception of health but
not mental health. The various diseases the person suffers from
determine the perception of one's functional limitations.
In
summary, some important considerations emerge and suggest the need for
further studies. For instance, future research could investigate the
close relationship between the lifestyle characterized by hyperactivity
and the deterioration in terms of quality of life and the association
between the perception of limitations to the activities of daily living
and the increase in psychological distress. Furthermore, it would be
useful to constitute a sample in which the group of co-infected and
that of non-co-infected are balanced. This aspect would confirm the
higher levels of externalizing symptoms, including paranoia, in the
first group. In addition, various sub-groups of co-infected PWH could
highlight interesting differences.
Finally, we emphasize the need
always to consider the HRQoL, which in our study appears to be
compromised by comorbidities. Considering that quality of life is one
of the best indices for the clinician to estimate the patient's level
of well-being, it is important to investigate the psychological aspects
and the medical variables that can impact it.
Conclusions
The
results of our preliminary research focus on the well-being of PWH and
their emotional experience. Our results agree with literature reports
and confirm that co-infections influence the manifestation of distress
(in terms of anxiety and depression, while PWH experiences
comorbidities are a consistent limitation of their lives. In addition,
the study underlines for the first time that these patients also
experience externalizing symptoms, including interpersonal sensitivity,
embarrassment, and paranoia. Nevertheless, it has also emerged that the
psychological variables investigated are associated. More specifically,
a general decline in well-being is associated with more intense mental
distress, even at a sub-clinical level. First, our results must be
confirmed to deepen the findings between mental health and hemophilia.
The
poor clarity in the factors that favor the impairment in the perceived
HRQoL and mental health remains an important clinical issue, and future
studies must be carried out.
Unfortunately, more in-depth
statistical analyses could not be performed because of the small sample
size and its large heterogeneity. Nevertheless, further research may
investigate a cause-effect relationship between the adopted lifestyle
and the decrease in perceived HRQoL. In addition, it could be useful to
verify if a greater perception of the limitations of the disease
corresponds to effective psychological suffering and investigate how
personality and psychological symptoms interact with each other and
affect psychophysical well-being.
This preliminary research
underlines the importance of multidisciplinary and multidimensional
management where a psychological investigation supplements the
clinical-medical evaluation. Psychological stress is frequently
mentioned among the predisposing,[44] precipitating, or perpetuating factors[45]
of physical pathologies in most medical fields, including
cardiovascular events, malignancies, and neurodegenerative disorders.[46-48]
Despite these reports, the medicine units that benefit from the
presence of clinical psychologists with specific curricula are still
few. Nevertheless, psychological support is useful for understanding
the clinical picture better and providing tailored interdisciplinary
treatment.
References
- Davari M, Gharibnaseri Z, Ravanbod R, Sadeghi A.
Health status and quality of life in patients with severe hemophilia A:
A cross-sectional survey. Hematol Rep. 2019; 11(2):7894. doi:
10.4081/hr.2019.7894. https://doi.org/10.4081/hr.2019.7894 PMid:31285808 PMCid:PMC6589534
- Bago
M, Butkovic A, Preloznik Zupan I, Faganel Kotnik B, Prga I, Bacic Vrca
V, Zupancic Salek S. Association between reported medication adherence
and health-related quality of life in adult patients with haemophilia.
Int J Clin Pharm. 2021; 43(6):1500-1507. doi:
10.1007/s11096-021-01270-x. https://doi.org/10.1007/s11096-021-01270-x PMid:33928481
- Mohan
R, Radhakrishnan N, Varadarajan M, Anand S. Assessing the current
knowledge, attitude and behaviour of adolescents and young adults
living with haemophilia. Haemophilia. 2021; 27(2):e180-e186. doi:
10.1111/hae.14229. https://doi.org/10.1111/hae.14229 PMid:33278862
- Buckner
TW, Sidonio R Jr, Witkop M, Guelcher C, Cutter S, Iyer NN, Cooper DL.
Correlations between patient-reported outcomes and self-reported
characteristics in adults with hemophilia B and caregivers of children
with hemophilia B: analysis of the B-HERO-S study. Patient Relat
Outcome Meas. 2019; 10:299-314. doi: 10.2147/PROM.S219166. https://doi.org/10.2147/PROM.S219166 PMid:31572035 PMCid:PMC6755243
- Holstein
K, von Mackensen S, Bokemeyer C, Langer F. The impact of social factors
on outcomes in patients with bleeding disorders. Haemophilia. 2016;
22(1):46-53. doi: 10.1111/hae.12760. https://doi.org/10.1111/hae.12760 PMid:26207763
- Cutter
S, Molter D, Dunn S, Hunter S, Peltier S, Haugstad K, Frick N, Holot N,
Cooper DL. Impact of mild to severe hemophilia on education and work by
US men, women, and caregivers of children with hemophilia B: The
Bridging Hemophilia B Experiences, Results and Opportunities into
Solutions (B-HERO-S) study. Eur J Haematol. 2017; 98 Suppl 86:18-24.
doi: 10.1111/ejh.12851. https://doi.org/10.1111/ejh.12851 PMid:28319337
- FRMY
Cassis, A Buzzi, A Forsyth, M Gregory, D Nugent, C Garrido, T Pilgaard,
DL Cooper, A Iorio. Haemophilia Experiences, Results and Opportunities
(HERO) Study: influence of haemophilia on interpersonal relationships
as reported by adults with haemophilia and parents of children with
haemophilia. Haemophilia. 2014; 20(4):e287-95. https://doi.org/10.1111/hae.12454 PMid:24800872
- Isfordink
CJ, van Erpecum KJ, van der Valk M, Mauser-Bunschoten EP, Makris M.
Viral hepatitis in haemophilia: historical perspective and current
management. Br J Haematol. 2021; 195(2):174-185. doi:
10.1111/bjh.17438. https://doi.org/10.1111/bjh.17438 PMid:33955555
- Lowe GD. Haemophilia, blood products and HIV infection. Scott Med J. 1987; 32(4):109-11. doi: 10.1177/003693308703200404. https://doi.org/10.1177/003693308703200404 PMid:3672104
- Barry
V, Lynch ME, Tran DQ, Antun A, Cohen HG, DeBalsi A, Hicks D, Mattis S,
Ribeiro MJ, Stein SF, Truss CL, Tyson K, Kempton CL. Distress in
patients with bleeding disorders: a single institutional
cross-sectional study. Haemophilia. 2015; 21(6):e456-64.
doi:10.1111/hae.12748. https://doi.org/10.1111/hae.12748 PMid:26179213
- Bussin
R, Johnson SB. Psychosocial issues in hemophilia before and after the
HIV crisis: a review of current research. Gen Hosp Psychiatry. 1992;
14(6):387-403.doi: 10.1016/0163-8343(92)90006-v. https://doi.org/10.1016/0163-8343(92)90006-V PMid:1473709
- Dew
MA, Ragni MV, Nimorwicz P. Infection with human immunodeficiency virus
and vulnerability to psychiatric distress. A study of men with
hemophilia. Arch Gen Psychiatry. 1990; 47(8):737-44. doi:
10.1001/archpsyc.1990.01810200045006. https://doi.org/10.1001/archpsyc.1990.01810200045006 PMid:2378544
- Catalan
J, Klimes I, Bond A, Day A, Garrod A, Rizza C. The psychosocial impact
of HIV infection in men with haemophilia: controlled investigation and
factors associated with psychiatric morbidity. J Psychosom Res. 1992;
36(5):409-16. doi: 10.1016/0022-3999(92)90001-i. https://doi.org/10.1016/0022-3999(92)90001-I PMid:1619581
- Marsettin
EP, Ciavarella N, Lobaccaro C, Ghirardini A, Bellocco R, Schinaia N.
Psychological status of men with haemophilia and HIV infection:
two-year follow-up. Haemophilia. 1995; 1(4):255-61. doi:
10.1111/j.1365-2516.1995.tb00085.x. https://doi.org/10.1111/j.1365-2516.1995.tb00085.x PMid:27214633
- Gil
F, Arranz P, Lianes P, Breitbart W. Physical symptoms and psychological
distress among patients with HIV infection. AIDS Patient Care. 1995;
9(1):28-31. doi: 10.1089/apc.1995.9.28. https://doi.org/10.1089/apc.1995.9.28 PMid:11361352
- Coppola
A, Santoro C, Franchini M, Mannucci C, Mogavero S, Molinari AC, Schinco
P, Tagliaferri A, Santoro RC. Emerging issues on comprehensive
hemophilia care: preventing, identifying, and monitoring age-related
comorbidities. Semin Thromb Hemost. 2013; 39(7):794-802. doi:
10.1055/s-0033-1354424. Epub 2013 Sep 8.PMID: 24014070. https://doi.org/10.1055/s-0033-1354424 PMid:24014070
- Tzitzikos
G, Kotrotsiou E, Bonotis K, Gourgoulianis K. Assessing hostility in
patients with chronic obstructive pulmonary disease (COPD). Psychol
Health Med. 2019; 24 (5): 605-619. doi:10.1080/13548506.2018.1554253. https://doi.org/10.1080/13548506.2018.1554253 PMid:30522331
- Oz
HS, Oz F. A psychoeducation program for stress management and
psychosocial problems in multiple sclerosis. Niger J Clin Pract. 2020;
23(11):1598-1606. doi:10.4103/njcp.njcp_462_19 https://doi.org/10.4103/njcp.njcp_462_19 PMid:33221788
- Grassi
L, Belvederi Murri M, Riba M, et al. Hostility in cancer patients as an
underexplored facet of distress. Psychooncology. 2021; 30(4):493-503.
doi:10.1002/pon.5594 https://doi.org/10.1002/pon.5594 PMid:33205480
- Apgáua
LT, Jaeger A. Memory for emotional information and alexithymia A
systematic review. Dement Neuropsychol. 2019; 13(1):22-30. doi:
10.1590/1980-57642018dn13-010003. https://doi.org/10.1590/1980-57642018dn13-010003 PMid:31073377 PMCid:PMC6497026
- Derogatis LR. SCL-90-R: Administration, Scoring and Procedures Manual. Minneapolis, MN. National Computer Systems, 1994.
- Sarno
I, Preti E, Prunas A, Madeddu F. SCL-90-R Symptom Checklist-90-R
Adattamento italiano. Firenze: Giunti, Organizzazioni Speciali, 2011.
- Derogatis LR. Misuse of the
symptom checklist 90. Arch Gen Psychiatry. 1983; 40(10):1152-3. doi:
10.1001/archpsyc.1983.01790090114025. https://doi.org/10.1001/archpsyc.1983.01790090114025 PMid:6625866
- Apolone
G, Mosconi P. The Italian SF-36 Health Survey: translation, validation
and norming. J Clin Epidemiol. 1998; 51(11):1025-36. doi:
10.1016/s0895-4356(98)00094-8. https://doi.org/10.1016/S0895-4356(98)00094-8 PMid:9817120
- Pruneti
C. The « P Stress Questionnaire »: A new tool for the evaluation of
stress-related behaviours, European Journal of Clinical Psychology and
Psychiatry,2011;VI, 3: 1-37.
- Pilowsky
I, Spence ND. Manual for the illness behavior questionnaire (IBQ), (3rd
Edn). Adelaide: University of Adelaide, 1994.
- Gringeri
A, Leissinger C, Cortesi PA, Jo H, Fusco F, Riva S, Antmen B, Berntorp
E, Biasoli C, Carpenter S, Kavakli K, Morfini M, Négrier C, Rocino A,
Schramm W, Windyga J, Zülfikar B, Mantovani LG. Health-related quality
of life in patients with haemophilia and inhibitors on prophylaxis with
anti-inhibitor complex concentrate: results from the Pro-FEIBA study.
Haemophilia, 2013; 19(5):736-43. doi: 10.1111/hae.12178. https://doi.org/10.1111/hae.12178 PMid:23731246
- Cuesta-Barriuso
R, Torres-Ortuño A, Nieto-Munuera J, López-Pina JA. Quality of Life,
Perception of Disease and Coping Strategies in Patients with Hemophilia
in Spain and El Salvador: A Comparative Study. Patient Prefer
Adherence. 2021; 15:1817-1825. doi: 10.2147/PPA.S326434. https://doi.org/10.2147/PPA.S326434 PMid:34456562 PMCid:PMC8387734
- Bago
M, Butkovic A, Faganel Kotnik B, Prga I, Bačić Vrca V, Zupančić Šalek
S, Preloznik Zupan I. Health-Related Quality of Life in Patients with
Haemophilia and Its Association with Depressive Symptoms: A Study in
Croatia and Slovenia. Psychiatr Danub. 2021; 33(3):334-341. doi:
10.24869/psyd.2021.334. https://doi.org/10.24869/psyd.2021.334 PMid:34795175
- Pinto
PR, Paredes AC, Moreira P, Fernandes S, Lopes M, Carvalho M, Almeida A.
Emotional distress in haemophilia: Factors associated with the presence
of anxiety and depression symptoms among adults. Haemophilia. 2018;
24(5):e344-e353. doi: 10.1111/hae.13548. https://doi.org/10.1111/hae.13548 PMid:30004620
- Banchev
A, Batorova A, Faganel Kotnik B, Kiss C, Puras G, Zapotocka E,
Zupancic-Salek S; Patient Advocacy Group. A Cross-National Survey of
People Living with Hemophilia: Impact on Daily Living and Patient
Education in Central Europe. Patient Prefer Adherence. 2021;
15:871-883. https://doi.org/10.2147/PPA.S303822 PMid:33953547 PMCid:PMC8091596
- Kempton
CL, Makris M, Holme PA. Management of comorbidities in haemophilia.
Haemophilia. 2021; 27 Suppl 3:37-45. doi: 10.1111/hae.14013. https://doi.org/10.1111/hae.14013 PMid:32476243
- Zawilska
K, Podolak-Dawidziak M. Therapeutic problems in elderly patients with
hemophilia. Pol Arch Med Wewn. 2012; 122(11):567-76. https://doi.org/10.20452/pamw.1466 PMid:23207414
- Franzoni
F, Scarfò G, Guidotti S, Fusi J, Asomov M, Pruneti C. Oxidative Stress
and Cognitive Decline: The Neuroprotective Role of Natural
Antioxidants. Front Neurosci. 2021; 15:729757. doi:
10.3389/fnins.2021.729757. https://doi.org/10.3389/fnins.2021.729757 PMid:34720860 PMCid:PMC8548611
- Sumari-de
Boer IM, Sprangers MA, Prins JM, Nieuwkerk PT. HIV stigma and
depressive symptoms are related to adherence and virological response
to antiretroviral treatment among immigrant and indigenous HIV infected
patients. AIDS Behav. 2012; 16(6):1681-9. doi:
10.1007/s10461-011-0112-y. https://doi.org/10.1007/s10461-011-0112-y PMid:22198315 PMCid:PMC3401302
- Torres-Ortuño
A, Cuesta-Barriuso R, Nieto-Munuera J, Galindo-Piñana P, López-Pina JA.
Coping strategies in young and adult haemophilia patients: A tool for
the adaptation to the disease. Haemophilia. 2019;25(3):392-397 https://doi.org/10.1111/hae.13743 PMid:30994251
- Carrico
AW, Bangsberg DR, Weiser SD, Chartier M, Dilworth SE, Riley ED.
Psychiatric correlates of HAART utilization and viral load among
HIV-positive impoverished persons. AIDS. 2011; 25(8):1113-8. doi:
10.1097/QAD.0b013e3283463f09. https://doi.org/10.1097/QAD.0b013e3283463f09 PMid:21399478 PMCid:PMC3601574
- Limperg
PF, Maurice-Stam H, Heesterbeek MR, Peters M, Coppens M, Kruip MJHA,
Eikenboom J, Grootenhuis MA, Haverman L. Illness cognitions associated
with health-related quality of life in young adult men with
haemophilia. Haemophilia. 2020; 26(5):793-799. doi: 10.1111/hae.14120. https://doi.org/10.1111/hae.14120 PMid:32842171
- Jones
QJ, Garsia RJ, Wu RT, Job RF, Dunn SM. A controlled study of anxiety
and morbid cognitions at initial screening for human immunodeficiency
virus (HIV) in a cohort of people with haemophilia. J Psychosom Res.
1995;39(5):597-608. doi: 10.1016/0022-3999(94)00147-2. https://doi.org/10.1016/0022-3999(94)00147-2 PMid:7490694
- Trindade
GC, Viggiano LGL, Brant ER, Lopes CAO, Faria ML, Ribeiro PHNS, Silva
AFDC, Souza DMR, Lopes AF, Soares JMA, Pinheiro MB. Evaluation of
quality of life in hemophilia patients using the WHOQOL-bref and
Haemo-A-Qol questionnaires. Hematol Transfus Cell Ther. 2019;
41(4):335-341. doi: 10.1016/j.htct.2019.03.010. https://doi.org/10.1016/j.htct.2019.03.010 PMid:31409581 PMCid:PMC6978543
- Yuvaraj
A, Mahendra VS, Chakrapani V, Yunihastuti E, Santella AJ, Ranauta A,
Doughty J. HIV and stigma in the healthcare setting. Oral Dis. 2020; 26
Suppl 1:103-111. doi: 10.1111/odi.13585. https://doi.org/10.1111/odi.13585 PMid:32862542
- Nanni
MG, Caruso R, Mitchell AJ, Meggiolaro E, Grassi L. Depression in HIV
infected patients: a review. Curr Psychiatry Rep. 2015; 17(1):530. doi:
10.1007/s11920-014-0530-4. https://doi.org/10.1007/s11920-014-0530-4 PMid:25413636
- Dalgard
O, Egeland A, Skaug K, Vilimas K, Steen T. Health-related quality of
life in active injecting drug users with and without chronic hepatitis
C virus infection. Hepatology. 2004; 39(1):74-80. doi:
10.1002/hep.20014. https://doi.org/10.1002/hep.20014 PMid:14752825
- Cosentino
C, Sgromo D, Merisio C, Berretta R, Pruneti C. Psychophysiological
Adjustment to Ovarian Cancer: Preliminary Study on Italian Women
Condition. Appl Psychophysiol Biofeedback.. 2018; 43(2):161-168. doi:
10.1007/s10484-018-9395-3. https://doi.org/10.1007/s10484-018-9395-3 PMid:29926266
- Pruneti
C. Guidotti S. Cognition, Behavior, Sexuality, and Autonomic Responses
of Women with Hypothalamic Amenorrhea. BrainSci. 2022;12:1448. https://doi.org/10.3390/brainsci12111448 PMid:36358374 PMCid:PMC9688049
- De
Vincenzo F, Cosentino C, Quinto RM, Di Leo S, Contardi A, Guidotti S,
Iani L, Pruneti C. Psychological adjustment and heart rate variability
in ovarian cancer survivors. Mediterr J Clin Psychol. 2022; 10. https://doi.org/10.13129/2282-1619/mjcp-3318.
- Morris
G, Reiche EMV, Murru A, Carvalho AF, Maes M, Berk M, Puri BK. Multiple
Immune-Inflammatory and Oxidative and Nitrosative Stress Pathways
Explain the Frequent Presence of Depression in Multiple Sclerosis. Mol
Neurobiol. 2018; 55(8):6282-6306. doi: 10.1007/s12035-017-0843-5. https://doi.org/10.1007/s12035-017-0843-5 PMid:29294244 PMCid:PMC6061180
- Pruneti
C, Guidotti S. Physiological Stress as Risk Factor for Hypersensitivity
to Contrast Media: A Narrative Review of the Literature and a Proposal
of Psychophysiological Tools for Its Detection. Physiologia. 2022;
2:55-65. https://doi.org/10.3390/ physiologia2030006. https://doi.org/10.3390/physiologia2030006
[TOP]