Marcelo Nóbrega Litvoc1, Fabio Eudes Leal2, Diogo Boldim Ferreira3, Max Igor Banks Ferreira Lopes1, Ligia Capuani4, Vanderson Geraldo Rocha5 and Silvia Figueiredo Costa1,4.
1 Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil.
2 Instituto Nacional de Câncer, Rio de Janeiro, Brazil.
3 Hospital São Paulo, Escola Paulista de Medicina da Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil.
4 Departamento de Doenças Infecciosas e Parasitárias,
Laboratório de Investigação Médica em Protozoologia, Bacteriologia e
Resistência Antimicrobiana (LIM 49), Faculdade de Medicina da
Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil.
5 Haematology Department, NHS BT, Oxford University, Oxford, UK.
Correspondence to:
Marcelo Nóbrega Litvoc, MD. Av. Dr. Enéas de Carvalho Aguiar
255-Cerqueira César. São Paulo, SP CEP 05403-000, Brazil. E-mail:
malitvoc@gmail.com Orcid: 0000-0002-5144-5451
Published: July 1, 2023
Received: January 5, 2023
Accepted: June 2, 2023
Mediterr J Hematol Infect Dis 2023, 15(1): e2023037 DOI
10.4084/MJHID.2023.037
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
To the editor
There
is limited data regarding tuberculosis in hematopoietic stem cell
transplantation (HSCT), especially in endemic countries. We conducted a
retrospective cohort study including all patients who underwent matched
unrelated allo-HSCT from 2007-2016 in the state of São Paulo, Brazil.
Tuberculosis in this population was identified by record linkage
between the national HSCT database (REREME) and the São Paulo State
Tuberculosis Control Program database. Five tuberculosis cases (3
males) were identified and described among 1,223 allo-HSCT. The mean
age was 25, and the mean time between HSCT and Tuberculosis diagnosis
was 376 days. Density incidence rate and standardized incidence ratios
(SIR) were compared between matched unrelated donor allo-HSCT and the
São Paulo state Tuberculosis database (172,925 cases). Considering
2,718 patients/year, the density incidence rate in the allo-HSCT
population was 183 cases/100.000 patients/year (SIR:4.9 and 95% CI
1.8-11:), much higher than the average rate for the whole population in
the state of São Paulo for the same period: 38.8/100.000
inhabitants. In our study, allo-HSCT patients are highly vulnerable to
tuberculosis disease, almost five times higher than in the general
population.
Tuberculosis incidence in hematopoietic stem cell transplant (HSCT)
recipients seems to be related to the prevalence in the country.[1,2]
In HSCT patients, the risk of tuberculosis is higher in allogeneic stem
cell transplantation (allo-HSCT). Tuberculosis incidence among
allo-HSCT has been reported from 0.014% to 16.0%.[3]
Data regarding Tuberculosis among HSCT is scarce even in endemic
countries such as Brazil, one of the 30 most high-burden tuberculosis
countries in the world.[4]
We aimed to describe tuberculosis's density incidence rate and standard incidence ratios (SIR) in matched unrelated allo-HSCT.
Methods
This
retrospective cohort study includes all matched unrelated allo-HSCT
patients in the São Paulo state from 2007 to 2016. We collected data
from the São Paulo State Tuberculosis Control Program and the national
allo-HSCT database from REREME at the National Institute of Cancer
(INCA.,2021).[5]
REREME collects data from all matched unrelated donors allo-HSCT in the
country. Probabilistic record linkage compares similarities between
databases applying mathematical functions. Data were reviewed to
correct errors and to standardize the content of the key variables –
name, surname, and date of birth. Those fields are recorded in a
Soundex code through parsing, substring, and transforming the text into
a phonetic code to make the linkage between misrecorded information.[6]
Record pairs are formed to be compared and classified into true pairs,
non-pairs, and doubtful pairs and then manually reviewed to accept or
reject the cases.
Available clinical, demographic, and epidemiological data of patients
with tuberculosis were compared to the entire allo-HSCT patient cohort.
During the study period, fluoroquinolones were recommended as bacterial
prophylaxis in Brazil during the neutropenia until the engraftment.
Microbiologic and molecular tests to diagnose tuberculosis are
available in all centers. However, the decision to perform
bronchoalveolar lavage (BAL) was of the clinical physician of each
Hospital.
In order to calculate the incidence density rate of tuberculosis, we
consider the contribution time from each patient, from the transplant
date until death or until December 31st,
2016, the final follow-up date. Long-term follow-up was characterized
by death (outcome) or tuberculosis diagnosis. No autopsy cases data
were available.
The study was approved by the institutional review board of the
Hospital das Clínicas da Faculdade de Medicina da Universidade de São
Paulo.
Statistical Analysis.
Density incidence rate and standard incidence ratios (SIR) were
calculated to compare the incidence of tuberculosis in matched
unrelated donor allo-HSCT and the general population in São Paulo
during the study period. Nominal and ordinal variables were described
as frequency and percentage; quantitative data, in median and range.
All calculations were performed with Epi-Info 7.2.
Results
In
the state of Sao Paulo, from 2007 until 2016, 1,223 matched unrelated
donor allo-HSCTs were performed. Among those, 1172 were new
transplants, 39 were second-time transplant recipients, and 12 patients
did the first transplant before the beginning of the study. Most
patients were males (713 cases-60%), and the mean age at the onset of
allo-HSCT was 25 years old. Acute Lymphoblastic Leukemia was the most
common diagnosis (359 patients), followed by Acute Myeloid Leukemia and
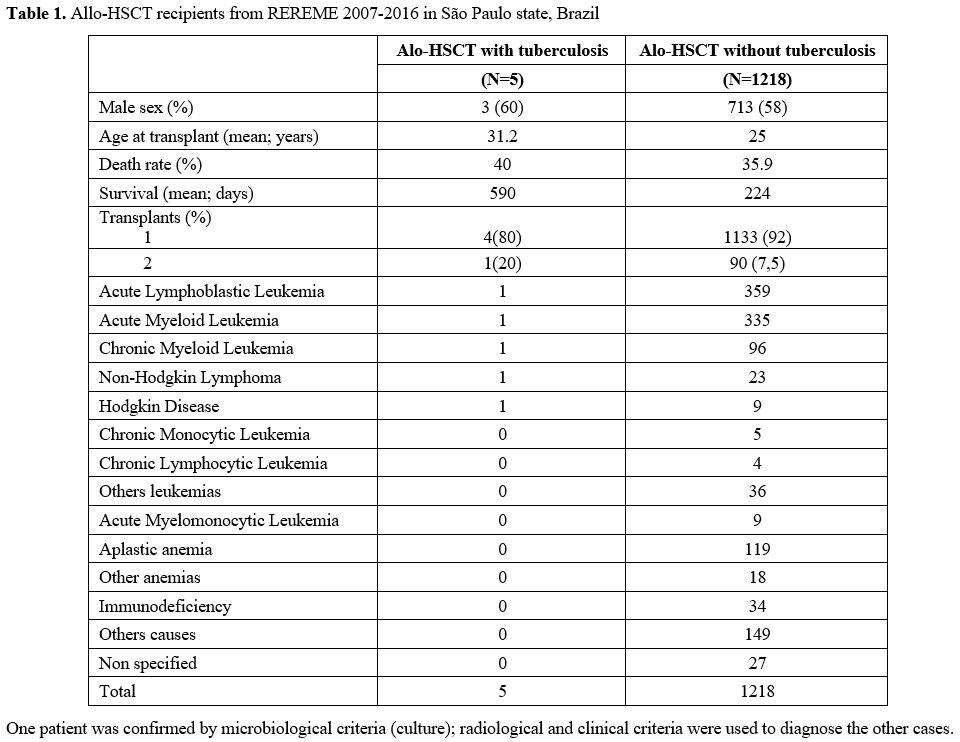
Chronic Myeloid Leukemia (Table 1).
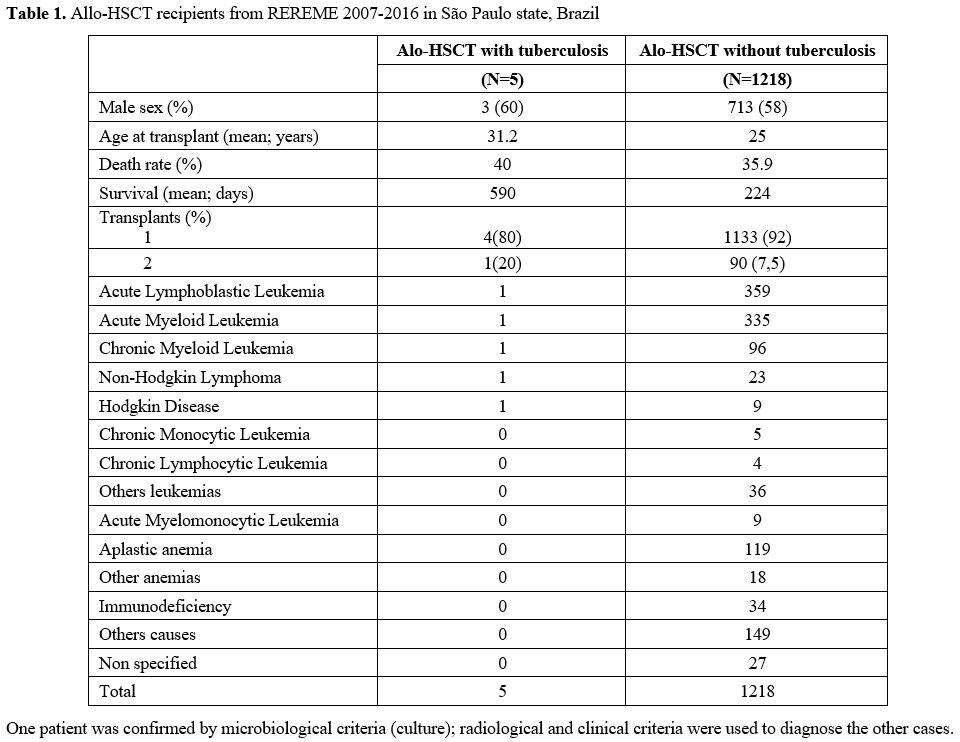 |
- Table 1. Allo-HSCT recipients from REREME 2007-2016 in São Paulo state, Brazil.
|
After
transplantation, 440 patients have not survived, with a death rate of
35.9% and an average survival time until the death of 182.7 days;
172,925 cases were identified in the São Paulo State Tuberculosis
Control Program database during the study period. Record linkage found
60 record pairs from two databases. After manual checking, 23
tuberculosis cases were identified among allo-HSCT patients. Five
tuberculosis cases were diagnosed after, and 17 cases were diagnosed
before the HSCT (Table 1 and supplementary material).
The period without TB of all HSCT patients ranged from 11 days to 9
years. Post-transplantation cases were diagnosed in four different
hospitals (2 public and 2 private) in the state of São Paulo. All new
cases were pulmonary forms of tuberculosis except one neurological
manifestation. The mean days between HSCT and Tuberculosis
diagnosis were 376 days (ranging from 61 days until 1048 days). Four
patients were cured after treatment with four drugs (RIPE); one case
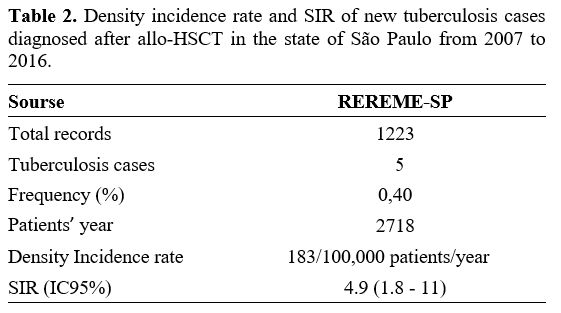
abandoned the treatment (Table 2).
The incidence rate was 183 cases per 100.000 patients/year, and the
SIR(4,9-95%CI:1.8-11.0). None of the 17 patients with previously
treated Tuberculosis before HSCT reactivated during the follow-up
period. The mean age of patients with previous tuberculosis was 19.3
years old. The mean time of diagnosis
of active tuberculosis was 439.2 days before HSCT. The RIPE
regimen was the most used in 10 cases (58.0%). The indication for HSCT
was: Acute myeloid leukemia (AML) 8 (47.0%), Combined immunodeficiency
3 (17.0%), unspecified neutrophil functional disorder 3 (17.0%),
Unspecified immunodeficiency 1 (5.8%) and other combined deficiencies
01 (5.8%). The clinical form of tuberculosis was pulmonary in 7 cases
(41.1%), disseminated in 4 cases (23.5%), lymph node in 2 cases
(11.7%), unspecified in 2 cases (11.7%), bone in 1 case (11.7%) and
"extrapulmonary", without other definitions, in 1 case (11.7%).cTn.
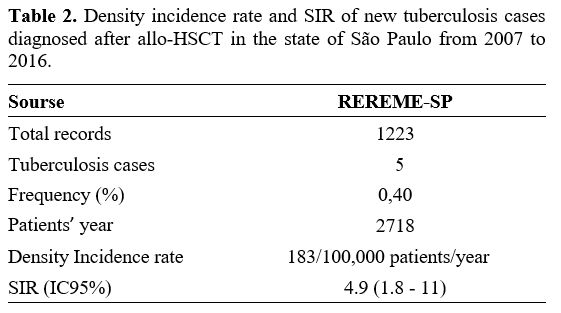 |
- Table
2. Density incidence rate and SIR of new tuberculosis cases diagnosed
after allo-HSCT in the state of São Paulo from 2007 to 2016.
|
Discussion
Our
study is the first attempt to improve epidemiological data about
Tuberculosis in HSCT in Brazil. Incidence of Tuberculosis matched
unrelated allo-HSCT (183 cases/100,000 patients/year) was 4.9 times
higher than the average rate for the population in the state of São
Paulo (38.8/100,000 inhabitants). A Spanish mathematical modeling study
has estimated an incidence rate of 135.6 cases per 100,000 inhabitants
after allo-HSCT.[2] A recent Brazilian study reported a cumulative tuberculosis incidence of 3% among allo-HSCT.[7]
Other authors observed a higher Tuberculosis incidence rate compared
with our study. In Korea, a retrospective study examined 845 matched
unrelated allo-HSCT and reported a Tuberculosis incidence of 654.2
/100,000 patients/year.[8]
Our study has limitations as most cases were treated based on clinical
and radiological findings. However, a relevant finding was the number
of patients, 17 with previously treated tuberculosis, that underwent
HSCT and did not reactivate during the follow-up period. Another
limitation of the study was that the susceptible testing was not
available. However, four of the five patients that developed TB after
HSCT were cured after treatment with four drugs, and one case abandoned
the treatment. Thus, there was probably no tuberculosis resistance
among the cases.
Conclusions
Tuberculosis
remains a healthcare concern in endemic countries. It should be
addressed in immunosuppressive conditions like allo-HSCT since its
incidence could be almost five times higher than in the general
population.
References
- Cordonnier C, Martino R, Trabasso P, Held TK, Akan
H, Ward MS, et al; European Blood and Marrow Transplant Group
Infectious Disease Working Party. Mycobacterial infection: a difficult
and late diagnosis in stem cell transplant recipients. Clin Infect Dis
2004;38(9):1229-36. https://doi.org/10.1086/383307 PMid:15127333
- De
la Cámara R, Martino R, Granados E, Rodriguez-Salvanés FJ, Rovira M,
Cabrera R, et al. Tuberculosis after hematopoietic stem cell
transplantation: incidence, clinical characteristics and outcome.
Spanish Group on Infectious Complications in Hematopoietic
Transplantation. Bone Marrow Transplant 2000;26(3):291-8.
https://doi.org/10.1038/sj.bmt.1702506 PMid:10967568
- Russo RL,
Dulley FL, Suganuma L, França IL, Yasuda MA, Costa SF. Tuberculosis in
hematopoietic stem cell transplant patients: case report and review of
the literature. Int J Infect Dis 2010;14 Suppl 3:e187-91.
https://doi.org/10.1016/j.ijid.2009.08.001 PMid:19819176
- Ministério da Saúde. Tuberculose - 2021. Boletim Epidemiológico. 2021;3(1):44.
- INCA
(Instituto Nacional de Câncer José Alencar Gomes da Silva) REDOME |
REDOME - Registro Nacional de Doadores de Medula Óssea - Site Oficial
[Internet]. 2021 [acesso em: 2021 10 set 10]. Disponível em:
http://redome.inca.gov.br/o-redome/conheca-o-redome/
- Oliveira
GP, Bierrenbach AL, Camargo KR Júnior, Coeli CM, Pinheiro RS. Accuracy
of probabilistic and deterministic record linkage: the case of
tuberculosis. Rev Saude Publica 2016;50:49.
https://doi.org/10.1590/S1518-8787.2016050006327 PMid:27556963
PMCid:PMC4988803
- De Oliveira MR, de Almeida Testa LH, Dos Santos
ACF, Zanetti LP, da Silva Ruiz L, de Souza MP, et al. Latent and active
tuberculosis infection in allogeneic hematopoietic stem cell transplant
recipients: a prospective cohort study. Bone Marrow Transplant
2021;56(9):2241-7. https://doi.org/10.1038/s41409-021-01329-3
PMid:33966056
- Lee HJ, Lee DG, Choi SM, Park SH, Cho SY, Choi JK,
et al, Min WS, Jung JI. The demanding attention of tuberculosis in
allogeneic hematopoietic stem cell transplantation recipients: High
incidence compared with general population. PLoS One
2017;12(3):e0173250. https://doi.org/10.1371/journal.pone.0173250
PMid:28278166 PMCid:PMC5344370
Online Supplement
 |
- Supplementary material. Clinical characteristics of tuberculosis in allo-HSCT in the state of São Paulo, Brazil.
|