Complete Kawasaki disease was diagnosed in 6 patients (60%) and its incomplete form in 4 patients (40%) by the opinion of pediatric and cardiovascular specialists (Table 2).
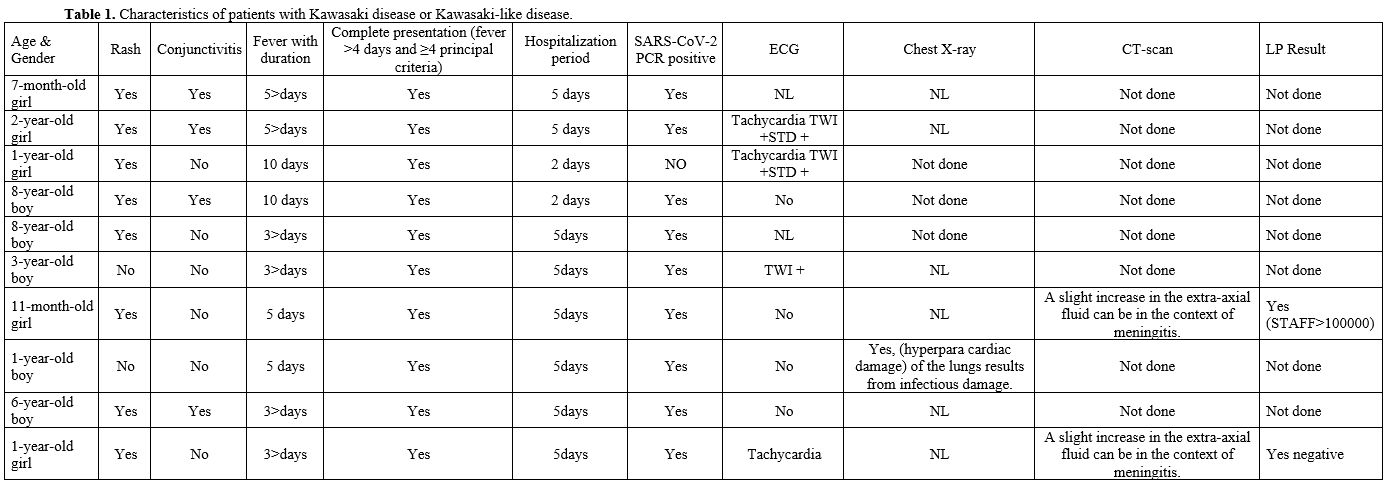 |
Table 1. Characteristics of patients with Kawasaki disease or Kawasaki-like disease. |
 |
Table 2. Diagnosis strategies. |
None of the patients developed coronary aneurysms, dilatations, or myocarditis. Pericardial effusion was seen in one patient (10%). Kawasaki disease has a wide range of clinical signs and symptoms.[6-9] The most common presenting symptoms are high fever, rash, conjunctivitis, lymphadenopathy, and strawberry tongue.[7,10] In addition, gastrointestinal manifestations of fever lasting more than 5 days have been suggested as a predictor of coronary artery involvement. In a study by Jafari et al. (2023) in Iran, the results of multivariate regression analysis showed that the duration of fever until diagnosis (fever more than 5 days) was a predictor of coronary artery involvement.[10] In the present study, more than three-quarters of children had a fever for more than 5 days, and coronary artery involvement was observed in one-quarter of children. Seven children (70%) had positive CRP. The study conducted by Li et al. (2024) also confirmed that a nomogram can effectively predict the risk of coronary artery lesions using CRP, IL-6, ESR, HDL, ox-HDL, etc. These findings suggest that when hospital laboratory resources are limited, standard detection indices such as HDL, ox-HDL, and ESR can be used to forecast the level of oxidative stress and inflammation-associated targets in coronary artery lesions associated with Kawasaki disease.[11] Although cardiac manifestations were less observed in the present study, gastrointestinal symptoms were reported in almost 100% of children. Early diagnosis and timely treatment when gastrointestinal symptoms are observed are recommended.[4]
Kawasaki disease lacks a definitive association with any single agent, and several infectious triggers, such as rhinovirus, Para influenza virus, respiratory syncytial virus, adenovirus,[10] human coronavirus,[6] and novel coronavirus, are known. However, some studies have ruled out the association of human coronavirus with Kawasaki disease.[10] At the same time, a study by Feldstein et al. (2020) in the U.S. reported Kawasaki-like disease during the COVID-19 epidemic.[2] Therefore, it is still unclear whether the diagnosis of COVID-19 in children with Kawasaki-related symptoms should be treated with a diagnosis of Kawasaki disease or whether a new separate diagnosis of COVID-19 infection is required. There is a need to differentiate coincidental COVID-19 infection with Kawasaki disease from Kawasaki disease caused by COVID-19. This article will help to understand and address the Kawasaki-like manifestations of pediatric COVID-19 infection, especially in intensive care units, and its possible complications. It will also help to make timely and appropriate decisions about its treatment and management. Based on the results of the present study, the manifestations of Kawasaki disease overlap with acute infectious diseases such as COVID-19, so timely identification and treatment of children with Kawasaki manifestations is essential to prevent acute and chronic cardiac, pulmonary, and renal complications. Therefore, the preparation of standard guidelines for screening and early identification of children with symptoms of acute inflammatory diseases (MISC, COVID-19, and KD) seems necessary.
References
- Sharma C, Ganigara M, Galeotti C, Burns J, Berganza
FM, Hayes DA, et al. Multisystem inflammatory syndrome in children and
Kawasaki disease: a critical comparison. Nat Rev Rheumatol 2021;
17:731-48 https://doi.org/10.1038/s41584-021-00709-9 PMid:34716418 PMCid:PMC8554518
- Feldstein
LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MBF, et al.
Multisystem inflammatory syndrome in U.S. children and adolescents. N
Engl J Med 2020; 383:334-46. https://doi.org/10.1056/NEJMoa2021680 PMid:32598831 PMCid:PMC7346765
- Belhadjer Z, Meot M, Bajolle F, et al. Acute heart failure in multisystem inflammatory syndrome in children in the context of global SARS-CoV-2 pandemic. Circulation. 2020; 142:429-436. https://doi.org/10.1161/CIRCULATIONAHA.120.048360 PMid:32418446
- Jones
VG, Mills M, Suarez D, et al.: COVID-19 and Kawasaki disease: novel
virus and novel case. Hosp Pediatr. 2020, 10:537-540.
10.1542/hpeds.2020-0123. https://doi.org/10.1542/hpeds.2020-0123 PMid:32265235
- Freeman
AF, Shulman ST: Kawasaki disease: American Heart Association guidelines
summary. Am Fam Physician. 2006, 74:1141-1148.
- Toubiana
J, Poirault C, Corsia A, et al. Outbreak of Kawasaki disease in
children during COVID-19 pandemic: a prospective observational study in
Paris, France. medRxiv. 2020; doi: 2020.05.10.20097394. https://doi.org/10.1101/2020.05.10.20097394
- Verdoni
L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like
disease at the Italian epicentre of the SARS-CoV-2 epidemic: an
observational cohort study. Lancet 2020; 395:1771-8. https://doi.org/10.1016/S0140-6736(20)31103-X PMid:32410760
- Mardi,
Parham, et al. Characteristics of children with Kawasaki disease-like
signs in COVID-19 pandemic: a systematic review. Frontiers in
pediatrics, 2021, 9: 625377. https://doi.org/10.3389/fped.2021.625377 PMid:33816398 PMCid:PMC8012548
- Kwak
JH, Lee SY, Choi JW, the Korean Society of Kawasaki Disease. Clinical
features, diagnosis, and outcomes of multisystem inflammatory syndrome
in children associated with coronavirus disease 2019. Clin Exp Pediatr
2021; 64:68-75. https://doi.org/10.3345/cep.2020.01900 PMid:33445833 PMCid:PMC7873390
- Sarouei
MJ, Kamali M, Charati FG, Shahbaznejad L, Hajialibeig A, Razavi-Amoli
SK, & et al. Epidemiological and Clinical Characteristics of
Kawasaki Disease in Journal Mazandaran Univ Med Sci 2022; 32 (212):
97-106 (Persian).
- Li Y., Lan S., Zhang H. Expression of oxidative stress and inflammatory indicators for coronary artery disease in Kawasaki disease. Mediterr J Hematol Infect Dis 2024, 16(1): e2024052. https://doi.org/10.4084/MJHID.2024.052 PMid:38984102 PMCid:PMC11232689