Materials and Methods
Blood samples: Blood samples were taken from 4091 participants attending different hospitals, including Azadi Teaching Hospital, Zakho General Hospital, Duhok Blood Bank, Duhok Obstetrics and Gynecology Hospital, and Zakho Obstetrics and Gynecology Hospital between January 2019 and December 2023. A 5-cc syringe and needle were used to obtain 5 mL of blood from the participants. Then, the blood samples were centrifuged at 1500 rpm for 3 min to separate sera, which were then immediately tested for HBsAg or kept frozen at –20°C until the tests were performed.Data Collection: A structured questionnaire was prepared and filled out by each study participant. Data were collected through face-to-face interviews, including age, gender, residency, marital status, history of blood transfusion, history of dental procedures, history of general operation, history of tattoos, and history of regular injections. Regular use of injections was defined as the regular use of over-the-counter injections or any other injections.
Enzyme-linked Immunosorbent Assay (ELISA): The presence of HBsAg was detected in serum samples by an ELISA test using a commercial HBsAg ELISA kit (ELISA 480 Test; AVONCHEM, Cheshire, UK) and ELISA 96 microwell plates. First, the anti-HBsAg antibody was applied and fixed to microwells. Subsequently, the sera of the participants were added to the fixed anti-HBsAg antibodies. After incubation, plates were washed to remove any components of the sera that were not bound to the antibodies. Secondary conjugated monoclonal antibodies bound to horseradish peroxidase were then added to the microwells of plates. After incubation, the unbound antibodies and enzymes were washed away. The stop solution and a colored substrate were added to the wells, and the results were recorded through an ELISA reader. The concentration of antigen in a sample is calculated using the optical density (OD). Thus, as per the manufacturer's instructions, the cut-off of HBsAg results are as follows: a. sample (OD) / cut-off value (S/C.O) ≥ 1 = positive; b. sample (OD) / cut-off value (S/C.O) < 1 = negative.
Statistics: Data analysis was computed using the IBM SPSS Statistics Version 25 software. Descriptive analysis was performed to categorize and generate percentages, means ± standard deviation (SD). Then, univariate and multivariate analysis was done by performing binary logistics regression to calculate the crude and adjusted odds ratio (OR), P values, and 95% confidence intervals (CI) for all potential factors associated with HBV infection. Statistical significance was set at p-value < 0.05.
Ethical statement: The study was approved by the College of Medicine Scientific and Ethics Committee at the University of Zakho, Kurdistan Region, Iraq (UoZ18-29). Before enrollment, written informed consent was obtained from all participants.
Results
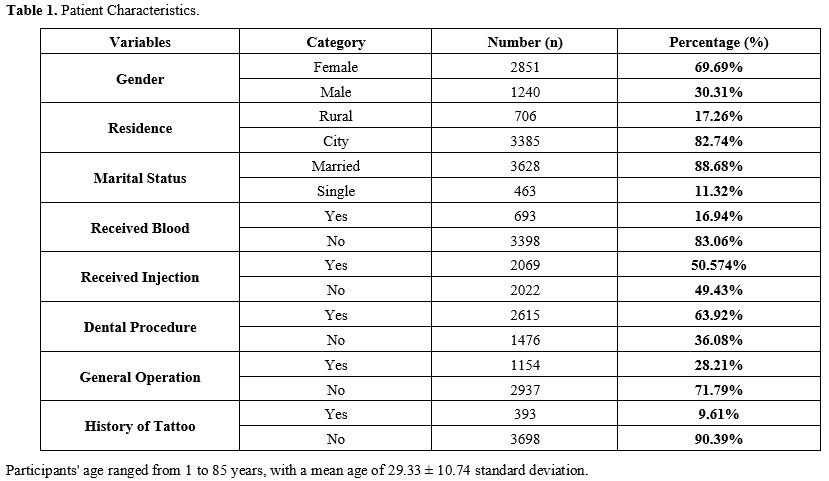
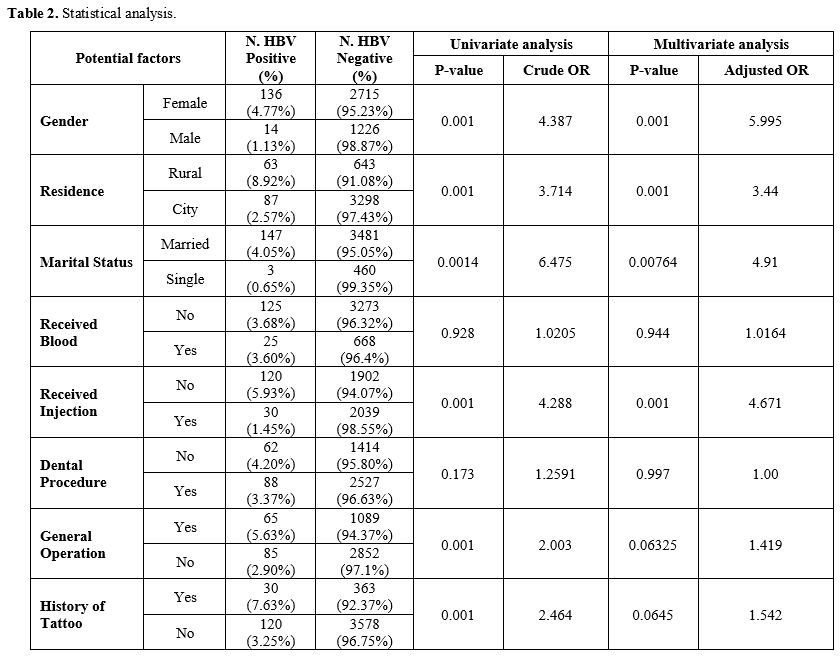
Demographic Data: The patient characteristics, including potential risk factors for HBV infection, were assessed via a questionnaire; the findings are presented in Table 1.HBV Positivity: Among the 4091 study participants, 150 tested positive for HBsAg (3.67%). The prevalence of HBV positivity among females was 4.77% (136/2851). This was significantly higher than the prevalence of HBV positivity among males, which was 1.13% (14/1240) (p = 0.001) (Table 2).
Risk factors for HBV infection: Various risk factors for HBV infection were considered, and the following factors were found to be statistically significantly associated with the HBV infection: gender, residence, marital status, receiving an injection, general operation, and history of tattoo (p = 0.001, 0.001, 0.0014, 0.001, 0.001 and 0.001 respectively). Multivariate analysis revealed that the association of surgical operation and history of tattoo to HBV infection is not statistically significant (multivariate p = 0.06325 and 0.0645, respectively) (Table 2).
Discussion
The prevalence of hepatitis B is not uniform and ranges from 0.5% in North and South America to 5.8% documented in Africa.[1,5] While this study is not a prevalence study because the sample collection was not random, HBV positivity was shown to be 3.67%, a rate that is higher than that of previous studies in the same region, which ranged from 0.54% to 1.37% during 2016 to 2022.[4,6,8,9] Our results are similar to what was found recently in Iran (3.4%) and Turkey (3%).[10,11] Although the reported prevalence of HBV positivity is high in our region, it is lower than the prevalence reported before the implementation of the HBV vaccine and its inclusion in the Expanded Program on Immunization in Iraq in 2000. Such a reduction was observed in other countries where vaccination programs have significantly reduced HBV prevalence over time.[12] In many high-income countries, the evaluation of HBsAg is performed using molecular techniques, which offer higher sensitivity and specificity. However, in our study, we used ELISA, and the differences in diagnostic approaches should be considered when comparing HBV prevalence across different regions.[13,14]The rate of HBsAg positivity among females was 4.77%, which was higher than the previously reported HBsAg positivity among exclusively pregnant women in Zakho (1.13%).[9] This finding is very important considering that women also have the possibility of vertically transmitting HBV to their offspring, who have a high risk of becoming chronically infected, especially when prenatal planning and treatment are not received.
Living in a rural area was significantly associated with HBsAg positivity as 8.97% of rural participants were infected compared to 2.57% of city residents; this aligns with a previous study result from Ethiopia.[15] However, no such difference was reported in another study conducted in our region.[9] The higher prevalence might be associated with the lack of knowledge regarding HBV, limited healthcare access, or preventive programs in rural areas. Furthermore, being married was also identified as predictive of HBsAg positivity, which might be due to the sexual transmission of the disease. Further studies are needed to investigate this.
A history of receiving blood was not associated with HBsAg positivity, similar to previous studies conducted in the region,[4,9] conceivably due to the viral screening practices required before donating blood or receiving a transfusion. No significant association between HBV infection and a history of prior dental procedures was identified.
In our region, therapeutic injections are readily delivered by untrained professionals in unsupervised settings. However, our study revealed that the rate of HBsAg positivity among those who have not received injections is significantly higher than those who received such injections (5.93% compared to 1.45%). This might be due to selection bias or different vaccination rates among such groups.
A history of surgical operation was found to be significantly associated with HBsAg positivity, but after a multivariate analysis, the association was not significant. Two other studies in the same region were also not able to identify an association,[4,9] but other studies in the same region[16] and from China[17] did find a significant correlation between the history of surgery and HBV positivity. Finally, a history of tattooing was similarly found to be significantly associated with HBsAg positivity, but after multivariate analysis, the association was not significant. While previous studies also could not find such associations,[4,16] an association was found between the history of tattooing and HBV infection in a study from the same region.[9] It is important to consider that the use and reuse of contaminated instruments in tattooing have the potential of transmitting the disease. The loss of association between a history of general operation or tattooing and HBV infection after multivariate analysis might indicate a confounding effect from other factors.
Our study's strengths include a large sample size, inclusion of both genders, all ages, and several centers. However, it also has limitations. First, it was a cross-sectional study design with questionnaires that were liable for recall bias and limited geographical coverage.
To conclude, 3.67% of the participants in this study were HBsAg positive; the predictive factors of infection were female gender, rural residency, and being married. Further population-based studies with larger sample sizes are needed to unify the results and be used to build a strong healthcare infrastructure to screen for hepatitis B.
References
- Global hepatitis report 2024: Action for access in
low- and middle-income countries. Geneva: World Health Organization;
2024. License: CC BY-NC-SA 3.0 IGO. Available at: https://www.who.int/publications/i/item/9789240091672
- Li,
Chunzheng, Chenyu Wei, and Xianguang Yang. "Hepatitis B Virus: Modes of
Transmission, Immune Pathogenesis, and Research Progress on Therapeutic
Vaccines." Exploration of Digestive Diseases 3, no. 6 (2024): 443-58. https://doi.org/10.37349/edd.2024.00060
- Pattyn,
Jade, Greet Hendrickx, Alex Vorsters, and Pierre Van Damme. "Hepatitis
B Vaccines." The Journal of Infectious Diseases 224, no. Supplement_4
(2021): S343-S51. https://doi.org/10.1093/infdis/jiaa668
- Hussein,
Nawfal. "Risk Factors of Hepatitis B Virus Infection among Blood Donors
in Duhok City, Kurdistan Region, Iraq." babol-caspjim 9, no. 1 (2018):
22-26. https://doi.org/10.22088/cjim.9.1.22.
- Patel,
Ankoor, Zahra Dossaji, Kapil Gupta, Katerina Roma, Toni-Marie Chandler,
Carlos D. Minacapelli, Kaitlyn Catalano, Robert Gish, and Vinod Rustgi.
"The Epidemiology, Transmission, Genotypes, Replication, Serologic and
Nucleic Acid Testing, Immunotolerance, and Reactivation of Hepatitis B
Virus." Gastro Hep Advances 3, no. 2 (2024): 139-50. https://doi.org/10.1016/j.gastha.2023.10.008 19
- Hussein,
Nawfal R., Dildar H. Musa, Dawan Jamal Hawezy, Ferhad M. R. Ahmed,
Fatma Kamal Khalid, Ibrahim A. Naqid, and Mahde Saleh Assafi. "A Study
on the Prevalence and the Risk Factors of Hepatitis B Virus Infection
in Kurdistan Region, Iraq: A Multicenter Study: Prevalence and the Risk
Factors of HBV." Journal of Contemporary Medical Sciences 7, no. 5
(10/26 2021). https://doi.org/10.22317/jcms.v7i5.1037
- Hussein
N R, Mohammed Abdullah I, Mohammed Younus O, Taher A M, Salim A A, et
al. "Prevalence of HBV, HCV and HIV Infections Among Syrian Refugees in
Kurdistan Region, Iraq." Int J Infect. 2017;4(2):e39420. https://doi.org/10.5812/iji.39420
- Nawfal,
Hussein, Zana Zana, Ibrahim Nashwan, Assafi Mahde, and Daniel Shameran.
"The Prevalence of HBV Infection in Renal Transplant Recipients and the
Impact of Infection on Graft Survival." Acta Medica Iranica 57, no. 6
(11/17 2019). https://doi.org/10.18502/acta.v57i6.1884
- Khalid
FK, Rasheed NA, Hussein NR, Naqid IA. "A study of HBV infection and its
risk factors in pregnant women in Zakho city, Iraq." PLoS ONE 17(8):
e0273362. (2022). https://doi.org/10.1371/journal.pone.0273362
- Mokhayeri,
Hamid, Banafsheh Hasanvand, Mehdi Birjandi, Habibollah Mirzaei, Paras
sasaei, Sara Zamani, Sakineh bajlan, Atefeh Akbari, and Sayyad
Khanizadeh. "Prevalence of HIV, HBV, and HCV Infections and High-Risk
Behaviors among Women Referred to Drop-in Centers of Lorestan Province,
Western Iran." [In en]. Archives of Razi Institute 79, no. 3 (2024):
623-28. https://doi.org/10.32592/ARI.2024.79.3.623
- Yekenkurul,
Dilek, Ali Rıza Gürbüz, Nevin Ince, and Emel Çalışkan. "Prevalence of
HBV, HCV, HIV and Effect on Clinical Course in COVID-19 Patients." [In
en]. Online Turkish Journal of Health Sciences 9, no. 1 (March 2024):
21-26. https://doi.org/10.26453/otjhs.1329992
- Chongsrisawat,
Voranush, Pornsak Yoocharoen, Apiradee Theamboonlers, Piyanit
Tharmaphornpilas, Porpit Warinsathien, Supakarn Sinlaparatsamee,
Siriraj Paupunwatana, et al. "Hepatitis B Seroprevalence in Thailand:
12 Years after Hepatitis B Vaccine Integration into the National
Expanded Programme on Immunization." Tropical Medicine &
International Health 11, no. 10 (2006/10/01 2006): 1496-502. https://doi.org/10.1111/j.1365-3156.2006.01709.x
- Yasseen,
Abdool S., Jeffrey C. Kwong, Jordan J. Feld, Rafal Kustra, Liane
MacDonald, Christina C. Greenaway, Naveed Z. Janjua, et al. "The Viral
Hepatitis B Care Cascade: A Population‐Based Comparison of Immigrant
Groups." Hepatology 75, no. 3 (2022). https://journals.lww.com/hep/fulltext/2022/03000/the_viral_hepatitis_b_care_cascade__a.19.aspx.
- Mishra
K., Shah A., Patel K., Ghosh K, Bharadva S. "Seroprevalence of HBV,
HCV, and HIV-1 and correlation with molecular markers among
multi-transfused thalassemia patients in Western India." Mediterr J
Hematol Infect Dis 2020, 12(1): e2020038. https://doi.org/10.4084/mjhid.2020.038
- Mohammed,
Hussein, Aragaw Eshetie, and Dessie Melese. "Prevalence of Hepatitis B
Virus and Associated Risk Factors among Adults Patients at Dessie
Referral and Kemise General Hospitals in Northeastern Ethiopia." Health
Science Reports 5, no. 3 (2022/05/01 2022): e659. https://doi.org/10.1002/hsr2.659
- Khalil,
Amira S., Nawfal R. Hussein, and Maida Y. Shamdeen. "Impact of Maternal
HBsAg Carrier Status on Pregnancy Outcomes in Duhok City, Iraq." Asian
Pacific Journal of Tropical Biomedicine 7, no. 11 (2017/11/01/ 2017):
1010-13. https://doi.org/10.1016/j.apjtb.2017.09.023
- Li, Xiaoqing, Yingjun Zheng, Adrian Liau, Biao Cai, Dongqing Ye, Feng Huang, Xiaorong Sheng, et al. "Hepatitis B Virus Infections and Risk Factors among the General Population in Anhui Province, China: An Epidemiological Study." BMC Public Health 12, no. 1 (2012/04/05 2012): 272..https://doi.org/10.1186/1471-2458-12-272